Blunt thoracic trauma is a common indication for hospital admission, with the predominant cause of trauma being motor vehicle collisions. The thorax is the fourth most injured area in unrestrained passengers, but it is the most commonly injured area in individuals who are restrained by a seat belt. Other common causes of blunt thoracic trauma include falls from heights of greater than 10 feet and motor vehicle collisions involving pedestrians/bicyclists. Radiologists must know the typical injuries associated with thoracic trauma to provide the proper diagnosis and contribute to the immediate treatment plan.
The initial screening test in thoracic trauma is the frontal chest radiograph obtained in the trauma bay. After the chest radiograph, computed tomography (CT) is the next most used diagnostic modality, although in the stable patient, cross-sectional imaging is often performed concurrently with radiographs. CT allows evaluation of the airways, pulmonary parenchyma, aorta and great vessels, pericardium, pleura, chest wall, diaphragm, and osseous structures.
The rapid acquisition of data with multidetector helical CT scanners has led to a significant increase in cross-sectional imaging in the setting of trauma. The value of multiplanar reformation, as allowed by the current CT scanners, cannot be overemphasized in the trauma setting.
Acute Traumatic Aortic Injury
Acute traumatic aortic injury (ATAI) is a common cause of prehospital mortality, accounting for approximately 15% to 20% of prehospital traumatic deaths. Of individuals with ATAI, 70% to 90% die at the trauma scene. Surviving trauma patients require prompt and accurate diagnosis to allow timely repair of the injury, especially given that 60% may have no overt clinical sign of thoracic trauma. The incidence of ATAI is approximately 1/100,000 per year.
Seven criteria have been described as important clinical predictors for the presence of ATAI. They are age older than 50 years; unrestrained patient; hypotension (defined as systolic blood pressure <90 mm Hg); thoracic injury; abdominopelvic injury requiring emergent laparotomy; concomitant fractures of the lumbar spine, pelvis, or long bones; and major head injury. If more than four of these criteria are present, the likelihood for ATAI is greater than 30%. A more recent evaluation of these criteria found that only four of the seven criteria were predictive of ATAI (abdominopelvic injury, thoracic injury, hypotension, and being unrestrained). Furthermore, the likelihood of ATAI in patients with three or four of these criteria was much lower, at 2%, which may be due to differences in patient populations and injury detection over the years.
Acute Traumatic Aortic Injury Anatomy
Most blunt aortic injuries occur at the level of the aortic isthmus just distal to the subclavian artery origin. The aortic isthmus extends from the origin of the subclavian artery to the insertion of the ligamentum arteriosum. The propensity for injury to occur at this location is not completely understood, but multiple mechanisms have been proposed. The osseous pinch mechanism suggests that the isthmus becomes compressed between the spine and the sternum. Shearing stress caused by sudden deceleration with force vectors pointing in opposite directions, centered at the aortic isthmus, is another hypothesis. The sudden increase in intraaortic pressure at the time of trauma, termed the water hammer effect , is a third possibility. The fourth theory is the viscous response theory, which states that the velocity of compression is the most important determining factor in internal chest trauma.
The ascending aorta is injured in less than 5% of patients with blunt ATAI who survive transport for further treatment. However, the ascending aorta is injured in approximately 22% of patients examined at autopsy. Ascending aorta injuries are frequently (80%) associated with significant cardiac damage, including valvular damage or pericardial tamponade, a lethal combination of injuries. Traumatic aortic injuries located at the diaphragmatic hiatus account for less than 2% of cases.
A mediastinal hematoma should prompt a close look at its proximity to the aorta and subsequent determination of aortic integrity. Hematoma is invariably present in the setting of aortic rupture but may also occur because of adjacent sternal or thoracic spine fractures or venous injury.
The continuous motion of the heart during cross-sectional scanning leads to motion artifacts of the ascending aorta that can have the appearance of aortic dissection or pseudoaneurysm; these artifacts are present even with current rapid-acquisition multidetector CT scanners. Care should be taken when interpreting the aorta in this area, especially as the ascending aorta is statistically less often injured.
Because the majority of patients with ATAI do not survive to hospitalization, and less than 5% of surviving patients will have an ascending aortic injury, the benefit of gated cardiac CT at initial presentation is limited. Most patients with ATAI are too unstable to undergo prolonged imaging, and thus evaluation of the aorta with standard, nongated CT is generally preferred. Finally, given the additional time and training requirements for technologists to adequately perform gated CT, in most cases only large academic trauma centers will have the resources to provide gated CT at all times of the day. However, in stable patients or those who require additional imaging after their initial presentation, gated CT can be an excellent resource to better evaluate potential ascending aortic injuries.
Pathology
ATAI ranges from intimal hemorrhage to complete transection. A transverse tear is the most common initial event, which can be segmental (55%) or circumferential (45%) and may be partial (65%) or transmural (35%). Spiral/irregular tears are very rare. The adventitia may be injured in up to 40% of cases, and adventitial injury is almost universally fatal because of rapid exsanguination, although in rare cases, temporary tamponade may be achieved by surrounding mediastinal soft tissues. Of those patients who survive and reach the hospital after aortic rupture, 22% die during initial resuscitation, 28% die during or shortly after surgical repair, and 14% develop subsequent paraplegia. Approximately 60% of tears involve the intima and media with an intact adventitia. Although infrequent, aortic dissection occurs in approximately 11% of trauma patients and may be secondary to baseline hypertension, along with subsequent acute increase in intraaortic blood pressure during the insult.
Manifestations of the Disease
Radiography
The chest radiograph is used to evaluate for the presence of a mediastinal hematoma, a finding that can be seen secondary to ATAI, sternal/thoracic spine fracture, or small artery or vein damage within the mediastinum. A mediastinal hematoma may represent free or partial flowing blood, indicative of small mediastinal vessel rupture, versus a contained rupture, the latter being more concerning for an ATAI.
The chest radiograph is most useful for exclusion of ATAI. The negative predictive value of a properly obtained chest radiograph is 98%. However, the positive predictive value is low, only 15%. Mediastinal fat, anomalous vessels, and the thymus can mimic mediastinal hemorrhage on the chest radiograph. Furthermore, technical considerations, such as supine imaging, magnification factors, and rotational factors, can also mimic mediastinal hematoma. The mechanism of injury should dictate the need for CT rather than the presence of a wide mediastinum. A more specific sign for mediastinal hematoma involves comparing the right paratracheal density with the left aortic arch region. When the right paratracheal region is equally dense or denser than the aortic arch, a mediastinal hematoma is more likely present ( Figs. 67.1 and 67.2 ).


Findings indicative of a contained aortic rupture include rightward deviation of a gastric tube (see Fig. 67.1 ), rightward deviation of the trachea, downward displacement of the left main bronchus, loss of aortic arch definition, increased aortic arch density (see Fig. 67.2 ), and increased width and density of the descending aorta. Findings indicative of a free- or partial-flowing hematoma include increased right paratracheal density in relation to the aortic arch, loss of aortic arch definition, left apical cap, and widened mediastinum (see Figs. 67.1 and 67.2 ).
The presence of a mediastinal hematoma is a sensitive but nonspecific finding in the setting of ATAI. The remaining signs have varying levels of specificity, the strongest of which include left apical cap (present in 65%), downward deviation of the left main bronchus (65%), and obscuration and increased density of the descending thoracic aorta (67%).
Signs With High Sensitivity and Low Specificity
- •
Mediastinal widening
- •
Abnormal or indistinct contour of the aorta
Signs With Relatively High Specificity and Low Sensitivity
- •
Rightward deviation of trachea at level of T4
- •
Rightward deviation of nasogastric tube at level of T4
- •
Thickening of right paratracheal stripe
- •
Negative predictive value of normal radiograph: 98%
Computed Tomography
Multidetector helical CT is a very sensitive diagnostic tool for exclusion of ATAI, often quoted as the gold standard for ATAI detection. A morphologically normal aorta with no mediastinal hematoma has a 100% negative predictive value for exclusion of ATAI. The positive predictive value is unclear at this time, however, with equivocal studies (hematoma only) requiring follow-up CT, aortography, or clinical observation.
Minimal aortic injury, defined as lesions only affecting the aortic intima without secondary signs of injury, represent about 10% of all cases of ATAI. Imaging findings suggesting minimal aortic injury include a polypoid intraluminal clot, low-density filling defect, or small intimal tear ( Fig. 67.3 ). Minimal aortic injury is important to recognize, as the treatment is different. Increasing reports show resolution of the injury on follow-up CT using conservative, nonoperative management (see Fig. 67.3 ).

Direct signs of ATAI that often require surgery or endovascular repair include a change in caliber of the aorta, aortic wall or contour abnormality (pseudoaneurysm) (see Figs. 67.1 and 67.2 ), contrast extravasation ( Fig. 67.4 ), and dissection. Diffuse circumferential perimural hematoma, which can extend down to the abdominal portion of the aorta, is another important finding ( Fig. 67.5 ). It is important to distinguish ATAI and the congenital variant of a “ductus bump.” A ductus bump is a mild, smooth, regular contour change of the aorta in the region of the ligamentum arteriosum and is a normal variant ( Fig. 67.6 ).



Transesophageal echocardiography is another valid option for exclusion of ATAI if there are no contraindications, such as vertebral body fracture or severe maxillofacial injury. The disadvantages of transesophageal echocardiography include the logistical time required to perform the study and the user dependence. If involvement of the ascending aorta is suspected, further evaluation with cardiac-gated computed tomography angiography should be considered.
Great Vessel and Supraaortic Branch Vessel Injury
The great vessels include the superior and inferior vena cava, pulmonary arteries, pulmonary veins, and aorta. Injury to the great vessels other than the aorta is rare. The supraaortic branch vessels comprise the brachiocephalic artery (right subclavian/right common carotid arteries), left common carotid artery, left subclavian artery, and brachiocephalic veins. Blunt traumatic injury to the supraaortic branch vessels is uncommon. When branch vessel injury is suspected, angiography can be a useful tool to diagnose subtle injury. One case review of 166 aortograms with 24 cases of positive aortic or supraaortic branch vessel injury, performed in high-mechanism thoracic trauma, revealed 4% with isolated injury to the aortic branch vessels and 1% with injuries to the aorta and its branches.
Manifestations of the Disease
Radiography
The screening trauma radiograph is unlikely to aid in the diagnosis of great vessel and supraaortic branch vessel injury. As in ATAI, a mediastinal hematoma may be present ( Fig. 67.7 ).

Computed Tomography
Multidetector CT and possibly subsequent angiography for evaluation of the great and supraaortic branch vessels are the most important diagnostic modalities. Similar to the setting of ATAI, CT may show endoluminal/intimal irregularity compatible with intimal tear. Alternatively, subtle findings, such as asymmetric vascular caliber, localized hematoma ( Fig. 67.8 ), or decreased contrast enhancement, may provide further evidence of vascular injury. Finally, dissection and complete disruption, if present, should reveal the dissection flap and pseudoaneurysm ( Fig. 67.9 ; see Fig. 67.7 ) that are typically seen with these entities. Although multidetector CT scans are likely to detect a traumatic injury to the supraaortic branch vessel, angiography is still considered the diagnostic gold standard.


Cardiac Injury
Significant cardiac injuries are uncommon in patients with blunt trauma who are seen in the emergency department. Autopsy data indicate that numerous prehospital deaths result from traumatic cardiac or valvular rupture.
Blunt cardiac injury can be divided into cardiac contusion and, more rarely, pericardial or myocardial rupture. The most innocuous and most common of these injuries, cardiac contusion, is usually a clinical diagnosis. Although CT can reveal multiple ancillary signs of cardiac contusion, the presence of normal myocardial enhancement should not be used to rule out cardiac injury. However, cardiac magnetic resonance imaging (MRI) and/or echocardiography may be beneficial if cardiac contusion is suspected to evaluate for wall motion abnormalities. Hemopericardium is visible on nearly all CT scans in cases of pericardial rupture.
Pathology
Hemopericardium may be the result of cardiac chamber rupture (prehospital death) or damage to the small surrounding pericardial vessels from displaced rib fractures (patient survives to hospitalization). Pericardial rupture more commonly occurs on the left side, although it can also occur along its pulmonary or diaphragmatic borders, or both. Such injuries become significant when the heart herniates through the tear, resulting in cardiac filling impedance or coronary vessel occlusion. The proposed mechanism of injury for pericardial rupture likens the injury to a pendulum because the inferior portion of the heart is free floating without significant attachments. In the setting of a lateral deceleration injury, the heart presumably collides with the adjacent pericardium, creating the rupture. Cardiac herniation through a pericardial defect may not be present initially and may occur after the administration or discontinuation of positive-pressure ventilation. The most commonly ruptured cardiac chamber in the autopsy population is the right ventricle, whereas the atria are the most commonly ruptured chambers in individuals who survive to hospitalization.
Manifestations of the Disease
Radiography
Hemopericardium may or may not be evident on chest radiography at presentation and usually manifests with an enlarged cardiac silhouette. Cardiac herniation should be suspected by an unusual position or configuration of the heart.
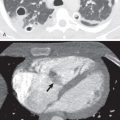
Computed Tomography
Most patients who have a mechanism of injury to produce hemopericardium are imaged with CT if stable, which reveals a hyperdense fluid collection in the pericardial space ( Fig. 67.10 ). Not all pericardial tears are associated with cardiac herniation; the chest radiograph and CT scan may be unrevealing. The presence of a focal pericardial defect with a collar sign of herniating cardiac tissue is the usual imaging manifestation ( Fig. 67.11 ). The presence of adjacent pneumothorax, pneumomediastinum, or both may complicate the diagnosis because the pericardium may be mistaken for the pleura in these settings.


Finally, pneumopericardium can rarely be seen in the trauma setting. Pneumopericardium, as opposed to pneumomediastinum, conforms more tightly to the cardiac contour and does not extend beyond the superior aortic recess. In addition, pneumopericardium, if significant, may result in compression of the heart with tamponade physiology.
Pulmonary Contusion
Pulmonary contusion is seen in 30% to 70% of patients with blunt thoracic injury. It is the most common cause of pulmonary parenchymal opacification on chest radiography in blunt thoracic trauma. Short-term morbidity is substantial, and clinical signs and symptoms include hypoxia, mild fever, hemoptysis, and dyspnea. Acute respiratory failure may develop, requiring intubation and mechanical ventilation. Pulmonary contusion is also associated with long-term respiratory dysfunction in patients with blunt chest trauma. The mortality rate is estimated at 10% to 25%.
Mechanism of Injury
Pulmonary contusion represents pulmonary hemorrhage and edema from disruption of the alveolar capillary membrane. It is often caused by a direct blow to the chest wall, with injury of the adjacent lung. Contrecoup injuries are common, and parenchymal contusion is frequently seen where the lungs have been compressed against the denser heart, liver, chest wall, and spine. In deceleration injuries, such as motor vehicle accidents, the alveolar capillary membrane is disrupted as the lower-density alveoli shear from the higher-density bronchovascular bundles. Pulmonary contusions may also be the result of rib fracture fragments directly lacerating the lung.
Although rare, disruption of the alveolar capillary membrane also occurs via spallation and implosion. Spallation is a bursting phenomenon that occurs when pressure waves deposit energy at liquid-gas interfaces, such as the blood-air interface of the alveolus. Spallation can occur from a blast injury or a direct blow. Implosion occurs after the transmission of a pressure wave through the alveolus, when there is overexpansion of alveolar gas.
Manifestations of the Disease
Radiography
Pulmonary contusions manifest as focal, patchy, or diffuse ground-glass opacities or parenchymal consolidation ( Fig. 67.12 ). These opacities cross segmental and fissural boundaries and are often present at the site of impaction and adjacent to rib fractures. The lung bases are most frequently affected secondary to increased basilar mobility. Air bronchograms are usually absent owing to blood filling the airways.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree