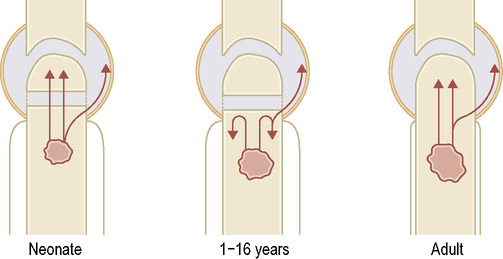
• The haematogenous pattern of infection differs depending on the patients age: • Blood supply to a long bone: • Infants up to 12 months: vessels penetrate the growth plate in both directions, allowing infection to easily pass to the epiphysis and joint space (pyogenic arthritis is a common sequelae of osteomyelitis in infants) • Older children: metaphyseal vessels terminate in slow-flowing sinusoids (promoting blood-borne infections) but few vessels cross the epiphyseal plate (resulting in less frequent epiphyseal and joint infections) • Adults: after growth plate fusion the metaphyseal and epiphyseal vessels are reconnected, allowing a septic arthritis • Haematogenous: Staphylococcus aureus (the most important) • Foreign body or implant: coagulase-negative staphylococci (skin commensals of low virulence) • Open fracture: aerobic Gram-negative rods (e.g. Pseudomonas) and anaerobic Gram-positive rods (e.g. Clostridium spp.) • Tumour: this tends to demonstrate a more homogeneous appearance than infection • Langerhans’ histiocytosis: with disseminated disease, multiple lesions of the same age are less likely to be infective • Aggressive degenerative disease: Milwaukee shoulder (rapidly progressive osteoarthritis) may mimic a septic arthritis • Irradiation: subsequent bone necrosis with osteopenia traversing a joint can mimic infection • SAPHO: synovitis + acne + pustulosis + hyperostosis + osteomyelitis. A series of similar conditions linking a sclerotic reaction that can mimic infection Haematogenous osteomyelitis of tubular bones†
Bone and soft tissue infection
ACUTE OSTEOMYELITIS
ACUTE OSTEOMYELITIS
Location
 Nutrient artery: the major source supplying the marrow and inner cortex
Nutrient artery: the major source supplying the marrow and inner cortex
 Periosteal vessels: these supply the outer cortex
Periosteal vessels: these supply the outer cortex
 the loose periosteum also allows pus to extend along the shaft to the epiphyseal plate (resulting in septic arthritis if the metaphysis is intracapsular)
the loose periosteum also allows pus to extend along the shaft to the epiphyseal plate (resulting in septic arthritis if the metaphysis is intracapsular)
 the periosteum is now well bound down and articular infections via a metaphyseal route are less likely
the periosteum is now well bound down and articular infections via a metaphyseal route are less likely
Causative organisms
 Haemophilus influenzae (in immunocompromised patients)
Haemophilus influenzae (in immunocompromised patients)  Streptococcus pneumoniae
Streptococcus pneumoniae  beta-haemolytic streptococci
beta-haemolytic streptococci  aerobic Gram-negative rods
aerobic Gram-negative rods
Differential diagnosis
 infection is more likely to produce soft tissue fluid-filled cavities
infection is more likely to produce soft tissue fluid-filled cavities  diagnosis is often only resolved with biopsy
diagnosis is often only resolved with biopsy
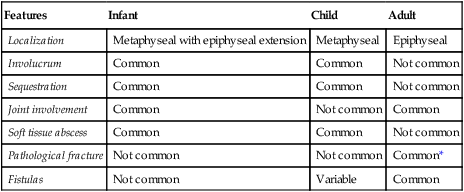
Features
Infant
Child
Adult
Localization
Metaphyseal with epiphyseal extension
Metaphyseal
Epiphyseal
Involucrum
Common
Common
Not common
Sequestration
Common
Common
Not common
Joint involvement
Common
Not common
Common
Soft tissue abscess
Common
Common
Not common
Pathological fracture
Not common
Not common
Common*
Fistulas
Not common
Variable
Common
Get Clinical Tree app for offline access

 it can also include contiguous spread (e.g. from trauma, surgery or chronic ulceration)
it can also include contiguous spread (e.g. from trauma, surgery or chronic ulceration) soft tissue redness and swelling (± discharging abscess)
soft tissue redness and swelling (± discharging abscess)  reduced function
reduced function  pyrexia and systemic ill health
pyrexia and systemic ill health
 there is early increased uptake
there is early increased uptake  it can be problematic in children as the growth plates are often adjacent to any involved areas
it can be problematic in children as the growth plates are often adjacent to any involved areas it initially extends beyond the limits of the true bone infection
it initially extends beyond the limits of the true bone infection  T1WI + Gad: enhancement
T1WI + Gad: enhancement a Codman’s triangle may also be present
a Codman’s triangle may also be present T2WI/STIR: a double line observed at the lesion margin
T2WI/STIR: a double line observed at the lesion margin

 there is a slow, chronic, infiltrative pattern that may mimic malignancy
there is a slow, chronic, infiltrative pattern that may mimic malignancy  it is hard to eradicate
it is hard to eradicate
 palmoplantar pustulosis
palmoplantar pustulosis  acne
acne  chronic relapsing multifocal osteomyelitis
chronic relapsing multifocal osteomyelitis  unilateral sacroiliitis
unilateral sacroiliitis  psoriasis vulgaris
psoriasis vulgaris  generalized pustular psoriasis
generalized pustular psoriasis

 it involves the same infective organisms as for an acute osteomyelitis
it involves the same infective organisms as for an acute osteomyelitis