Brain Infections
Lee Finkelstone
Ernst Garcon
Gaurav Jindal
Gul Moonis
QUESTIONS
1 A previously healthy 30-year-old presents with seizures and recent travel history.
|
1a What is the most likely diagnosis?
A. Toxoplasmosis
B. Neurocysticercosis
C. Metastatic disease
D. Tumefactive multiple sclerosis
View Answer
1a Answer B. Neurocysticercosis. In a young patient with travel history, seizures, and multiple peripherally enhancing cystic lesions, neurocysticercosis is the most likely diagnosis. Also, there is a suggestion of enhancing nodules at the posterior aspect of the lesions, likely representing the scolex.
1b In regard to neurocysticercosis, edema surrounding the cystic lesions is greatest in which stage of the disease?
A. Vesicular
B. Colloidal vesicular
C. Granular nodular
D. Nodular calcified
View Answer
1b Answer B. Colloidal vesicular. There are four stages of neurocysticercosis: vesicular, colloidal vesicular, granular nodular, and nodular calcified. Surrounding edema is greatest in the colloidal vesicular phase.
|
Imaging Findings: Figures A and B show T2 hyperintense cystic lesions in the medial right temporal lobe and left parietal lobe at the convexity, although the hyperintense signal is not as bright as CSF and is heterogeneous. Figures C and D show peripheral ring-like enhancement of the cystic lesions.
Discussion: Neurocysticercosis is caused by a parasitic infection from the pork tapeworm Taenia solium. It is the most common parasitic disease of the central nervous system worldwide, and travel and globalization have caused the disease to now spread beyond endemic regions. Patients most commonly present with seizures. Treatment depends on viability of the lesions, number of lesions, and extent of surrounding edema but is often with albendazole and steroids. Surgical intervention may be needed if hydrocephalus has developed.
Lesions can be parenchymal, intraventricular, or within the subarachnoid spaces. When parenchymal, the cysts are most commonly located at the gray-white matter junction. When intraventricular, the cysts are often solitary with predilection for the fourth ventricle. When subarachnoid, cysts tend to occur at the cortical sulci. When in the basilar cisterns, cysts may be racemose or “grape-like.”
There are four stages of the disease with distinct imaging findings. In the vesicular stage, the cyst is thin walled and has signal characteristics similar to CSF without contrast enhancement or edema. An eccentric, discrete scolex can be seen. In the colloidal vesicular phase, the larva begins to degenerate creating an inflammatory response and resultant surrounding edema. The hyperintense cyst at this stage will demonstrate ring-like peripheral enhancement. In the granular nodular stage, the cyst decreases in size and the cyst wall retracts, surrounding edema decreases, and nodular or ring-like enhancement persists. Finally in the nodular calcified stage, the cyst is shrunken and calcified with hypointensity on T2 and gradient echo sequences.
References: Kiumura-Hayama ET, et al. Neurocysticercosis: radiologic-pathologic correlation. Radiographics 2010;30(6):1705-1720.
Lucato LT, et al. The role of conventional MR imaging sequences in the evaluation of neurocysticercosis: impact on characterization of the scolex and lesion burden. AJNR Am J Neuroradiol 2007;28:1501-1504.
Zhao JL, et al. Imaging spectrum of neurocysticercosis. Radiol Infect Dis 2015;1(2):94-102.
2 A 50-year-old presents with fever, headaches, and new-onset seizures. Brain MRI with gadolinium was done, and selected images are submitted for review.
|
2a The abnormal MRI findings are:
A. Parenchymal
B. Intraventricular
C. Extra-axial
D. Parenchymal and extra-axial
View Answer
2a Answer D. Parenchymal and extra-axial. The prioritization of differential diagnosis considerations in the evaluation of a neuroimaging study depends on the anatomic location of the findings, whether intra-axial/parenchymal, extra-axial, or both. The images provided clearly identify parenchymal and extra-axial signal abnormalities and enhancement (option D).
2b What is the most likely diagnosis?
A. Herpes encephalitis
B. Cerebral abscess
C. Subdural empyema
D. Gangliocytoma
View Answer
2b Answer C. Subdural empyema. The extra-axial loculated enhancing collection with associated restricted diffusion and adjacent parenchymal edema favors a subdural empyema with cerebritis.
|
Imaging Findings: Axial T2-weighted image demonstrates gyral crowding in the left parietal lobe with prolonged T2 signal in the involved subcortical white matter consistent with vasogenic edema/cerebritis. Please note the preservation of the normal cortical thickness. Axial postgadolinium T1-weighted image demonstrates a small loculated extra-axial collection with a rim of enhancement in the left parietal region. The crescentic shape of the collection suggests a subdural location. In addition, there is diffuse smooth thickening and enhancement of the adjacent left frontoparietal pachymeninges. Diffusion-weighted image shows restricted diffusion in the extra-axial collection consistent with an empyema.
Discussion: Subdural empyema (SDE) is an uncommon infected extra-axial fluid collection located in the subdural space. SDE usually occurs as a complication of acute sinusitis, mastoiditis, meningitis, or trauma and can result in severe complications such as cortical vein thrombosis, venous infarcts, cerebritis, or abscess.
The clinical presentation depends on the etiology and anatomic location of the SDE. The patient is usually very sick with seizures, headaches, focal neurologic deficits, or altered sensorium.
The imaging evaluation may start with a noncontrast head CT that will demonstrate diffuse or focal brain swelling. If the clinical suspicion of SDE is high, a contrast-enhanced CT or MRI is preferred. The postcontrast images demonstrate enhancement of the wall of a crescentic-shaped extra-axial collection. SDE crosses the calvarial sutures like any other types of subdural collection. On MRI, the diffusion-weighted images (DWI) will establish the infected nature of the fluid.
The treatment is surgical evacuation and appropriate antibiotic therapy.
Differential Diagnosis: The main differential diagnosis is an epidural empyema that is meniscal in shape. Other extra-axial fluid collections containing blood products or cerebrospinal fluid should also be considered. Subdural lymphoma may occasionally be a diagnostic challenge on imaging (restricted diffusion), but clinical findings are very different from an acutely infected patient.
Reference: Wong AM, Zimmerman RA, Simon EM, et al. Diffusion-weighted MR imaging of subdural empyemas in children. AJNR Am J Neuroradiol 2004;25(6):1016-1021.
3 A 63-year-old status post bone marrow transplant (BMT) for plasmacytoma of the skull base complains of new headaches. Selected images from MRI are presented below.
|
3a What is the best explanation for the imaging findings taking into account the patient’s clinical history and presentation?
A. Ischemic lacunar infarcts
B. Hemorrhagic infarcts
C. Hematogenous metastases
D. Multiple small abscesses
View Answer
3a Answer D. Multiple small abscesses. The best explanation is multiple small abscesses in an immunocompromised patient.
3b What is the most likely diagnosis?
A. CNS cryptococcal infection
B. Herpes encephalitis
C. Acute stroke
D. Multiple sclerosis
View Answer
3b Answer A. CNS cryptococcal infection. The most likely diagnosis in an immunocompromised patient with enhancing cystic lesions and restricted diffusion at the base of the brain is CNS cryptococcal infection (option A).
|
Imaging Findings: Axial DWI of the brain shows punctate foci of hyperintense signal in the bilateral basal ganglia that may represent restricted diffusion or T2 shine through. After correlation with dark ADC map signal (not shown) that confirmed true restricted diffusion, the postgadolinium images in axial and coronal planes demonstrate multiple ring-enhancing lesions in the basal ganglia that are consistent with parenchymal cryptococcoma.
Discussion: CNS cryptococcosis is a fungal infection of the brain caused by Cryptococcus neoformans. It is predominately seen in immune-suppressed patient with AIDS or cancer or after bone marrow transplant.
The histology of CNS involvement is primarily meningeal, less frequently parenchymal with typical distribution in the basal ganglia and midbrain, resulting in the three most common imaging patterns of meningitis, cryptococcoma, or gelatinous pseudocysts.
Clinically, the patient may present with signs and symptoms of meningitis or meningoencephalitis including headaches, seizures, blurry vision, or altered mental status.
CT scan is nonspecific and may demonstrate hydrocephalus or localized brain swelling. This case illustrates the typical MRI appearance of parenchymal cryptococcomas with accumulation of a mucinous exudate in the dilated perivascular spaces of the basal ganglia. DWI and postgadolinium images are sufficient to suggest the diagnosis and start appropriate therapy.
The treatment is amphotericin B or fluconazole with a 20% mortality rate in AIDS patients despite antifungal treatment. A fatal outcome will occur without prompt diagnosis and treatment.
Differential Diagnosis: The differential diagnoses include other CNS infections like toxoplasmosis and tuberculosis, which also occur in immunocompromised patients. A lumbar puncture with CSF analysis, culture, and sensitivity may confirm the diagnosis for targeted antibiotic therapy. Other diagnostic considerations will include primary or secondary CNS lymphoma.
Reference: Charlier C, Dromer F, Lévêque C, et al. Cryptococcal neuroradiological lesions correlate with severity during cryptococcal meningoencephalitis in HIV-positive patients in the HAART era. PLoS One 2008;3(4):e1950.
4 A 30-year-old with HIV not compliant with HAART therapy presents with confusion and ataxia.
|
4a What is the most likely diagnosis?
A. Metastatic disease
B. Toxoplasmosis
C. Lymphoma
D. Active demyelinating disease
View Answer
4a Answer B. Toxoplasmosis. Given that there are multiple lesions with distribution including the basal ganglia, corticomedullary junction, and cerebellum, the diagnosis favors toxoplasmosis over lymphoma. Metastatic disease can have a similar imaging appearance, but given the provided history of a young patient with HIV, toxoplasmosis is the most likely diagnosis.
4b In regard to imaging findings on thallium 201 SPECT in toxoplasmosis and lymphoma, which statement is correct?
A. Toxoplasmosis and lymphoma are both hypometabolic.
B. Toxoplasmosis is hypometabolic and lymphoma is hypermetabolic.
C. Toxoplasmosis is hypermetabolic and lymphoma is hypometabolic.
D. Toxoplasmosis and lymphoma are both hypermetabolic.
View Answer
4b Answer B. Toxoplasmosis is hypometabolic and lymphoma is hypermetabolic. Similarly, lymphoma is hypermetabolic on 18F-FDG PET and demonstrates increased relative cerebral blood flow on MR perfusion. An easy way to remember this is that lymphoma is an active tumor, so no matter how you image it, it should be “hot!”
|
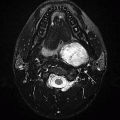
Imaging Findings: Axial FLAIR and postgadolinium images through the posterior fossa show a large rim-enhancing left cerebellar lesion with surrounding vasogenic edema and resultant mass effect on the fourth ventricle. The lesion is centrally mildly T2 hyperintense with hypointense rim. Higher axial scans demonstrate an additional right frontal rim-enhancing lesion. The multiplicity of the ring-enhancing lesions in an HIV patient favors toxoplasmosis as the leading diagnosis.
Discussion: Toxoplasmosis is an opportunistic infection caused by the parasite Toxoplasma gondii. It is the most common opportunistic CNS infection in AIDS patients, often when the CD4 count is <200. Toxoplasmosis is often spread by eating poorly cooked meat exposed to infected cat feces and can be transferred from mother to fetus leading to congenital toxoplasmosis. Patients with CNS toxoplasmosis can present with fever, malaise, headaches, and seizures. Treatment for toxoplasmosis is pyrimethamine and sulfadiazine.
On imaging, toxoplasmosis and lymphoma can look very similar in AIDS patients. Toxoplasmosis tends to reveal multiple ring-enhancing lesions in the basal ganglia and corticomedullary junction. Lymphoma is usually a single, solid-enhancing periventricular lesion in immunocompetent patients but is more often multifocal and irregularly enhancing or rim enhancing in AIDS patients. Both can restrict diffusion; however, it has been shown that toxoplasmosis demonstrates greater restriction on average when compared to lymphoma.
Given the overlap of imaging findings, advanced MR imaging and nuclear medicine are both helpful tools. On MR perfusion, lymphoma has increased perfusion and toxoplasmosis has decreased perfusion. On MR spectroscopy, both can have lipid-lactate peaks, but lymphoma tends to have significantly increased Cho/Cr ratio. On thallium 201 SPECT and 18F-FDG PET, lymphoma is hypermetabolic and toxoplasmosis is hypometabolic.
References: Camacho D, et al. Differentiation of toxoplasmosis and lymphoma in AIDS patients by using apparent diffusion coefficients. AJNR Am J Neuroradiol 2003;24:633-637.
Haldorsen IS, et al. Central nervous system lymphoma: characteristic findings on traditional and advanced imaging. AJNR Am J Neuroradiol 2011;32:984-992.
Ruiz A, et al. Use of thallium-201 brain SPECT to differentiate cerebral lymphoma from toxoplasma encephalitis in AIDS patients. AJNR Am J Neuroradiol 1994;15:1885-1894.
5 A 4-year-old presents with fever, failure to thrive, and altered mental status.
|
5a What best describes the imaging findings?
A. Basilar pachymeningeal enhancement with hydrocephalus
B. Basilar pachymeningeal enhancement without hydrocephalus
C. Basilar leptomeningeal enhancement with hydrocephalus
D. Basilar leptomeningeal enhancement without hydrocephalus
A chest x-ray was obtained.
|
View Answer
5a Answer C. Basilar leptomeningeal enhancement with hydrocephalus. Pachymeningeal enhancement refers to dura-arachnoid enhancement adjacent to the inner table of the skull, in the falx, and in the tentorium. On the other hand, leptomeningeal enhancement refers to pia-arachnoid enhancement, which follows the pial surface of the brain in the subarachnoid spaces of the sulci and cisterns. As a result of the basilar leptomeningeal meningitis, hydrocephalus has developed with dilated temporal horns for the patient’s age.
5b Given the chest x-ray, what is the most likely diagnosis for the brain imaging findings?
A. Neurosarcoid
B. TB meningitis
C. CNS lymphoma
D. Subarachnoid hemorrhage
View Answer




5b Answer B. TB meningitis. Given the diffuse miliary nodules on the chest x-ray in a sick child with fever, the most likely diagnosis for the brain imaging findings is TB meningitis.
|
|
Imaging Findings: Sagittal, axial, and coronal postgadolinium images demonstrate robust basilar leptomeningeal enhancement along the surface of the midbrain, within the suprasellar cistern, and extending to the right sylvian fissure. The chest x-ray demonstrates an intubated child with innumerable bilateral miliary nodules. Although both basilar leptomeningeal enhancement and miliary nodules can have their own differential considerations, when the two findings are seen together, TB meningitis is the most likely diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree