• The breast lies on the chest wall and on the deep pectoral fascia • High spatial resolution is required to detect microcalcification: a short exposure time limits any movement artefact • There is a narrow range of inherent breast densities (as it is predominantly fatty tissue): low molybdenum energy peaks (17.5 and 19.6keV) provide high contrast (filtering reduces extraneous radiation) • Breast compression: this reduces geometric and movement unsharpness • Mediolateral oblique (MLO) view (standard): • Craniocaudal (CC) view (standard): • Paddle views (supplementary): • True lateral view (supplementary): • Magnification views (supplementary): • Eklund technique (supplementary): • Exaggeration of the normal cyclical proliferation and involution of breast tissue with the development of fibrosis • A benign tumour arising from the TDLU (fibrous stroma + epithelial ductal structures) • Requires biopsy for diagnosis unless <25 years old (to exclude malignancy) • Juvenile fibroadenoma: a more cellular variant occurring at a younger age • Phyllodes tumour: a fibroepithelial tumour similar to a giant fibroadenoma, affecting an older age group
Breast
NORMAL ANATOMY
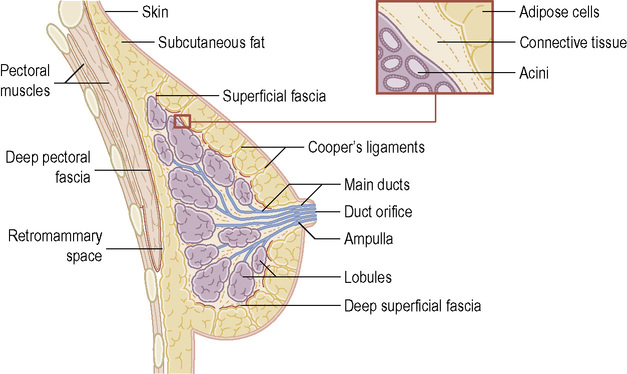
 the superficial pectoral fascia envelops the breast
the superficial pectoral fascia envelops the breast  suspensory ligaments (Cooper’s ligaments) connect the two layers
suspensory ligaments (Cooper’s ligaments) connect the two layers
2 components
 Collecting ducts open onto the tip of the nipple
Collecting ducts open onto the tip of the nipple
 Sebaceous glands within the nipple–areolar complex are called Montgomery’s glands
Sebaceous glands within the nipple–areolar complex are called Montgomery’s glands  ducts open onto the skin surface (and are seen as small raised nodular structures called Morgagni’s tubercles)
ducts open onto the skin surface (and are seen as small raised nodular structures called Morgagni’s tubercles)
 This is divided into 15–25 lobes, each consisting of a branching duct system leading from the collecting ducts to the terminal duct lobular units (TDLUs)
This is divided into 15–25 lobes, each consisting of a branching duct system leading from the collecting ducts to the terminal duct lobular units (TDLUs)
 Each duct drains a lobe made up of 20–40 lobules
Each duct drains a lobe made up of 20–40 lobules
 Young women usually have dense glandular breast tissue
Young women usually have dense glandular breast tissue  this is usually replaced by fatty tissues in older women with loss of the lobular units
this is usually replaced by fatty tissues in older women with loss of the lobular units
 Lymphatic drainage is usually to the axillary and internal mammary nodes
Lymphatic drainage is usually to the axillary and internal mammary nodes
METHODS OF IMAGING
Imaging in mammography
 it requires a very small focal spot (0.1–0.3mm)
it requires a very small focal spot (0.1–0.3mm)  grids are used to reduce scatter and increase contrast
grids are used to reduce scatter and increase contrast  digital mammography is now used
digital mammography is now used
 it improves contrast (it reduces scatter)
it improves contrast (it reduces scatter)  it reduces radiation dose (less tissue needs to be penetrated)
it reduces radiation dose (less tissue needs to be penetrated)  it achieves uniform image density
it achieves uniform image density  it separates superimposed breast tissues
it separates superimposed breast tissues  it highlights rigid tumours (glandular tissue is compressible)
it highlights rigid tumours (glandular tissue is compressible)
Mammography (digital/analogue) (MMG)
 Evaluation of breast symptoms and signs, including masses, skin thickening, deformity, nipple retraction, nipple discharge and nipple eczema
Evaluation of breast symptoms and signs, including masses, skin thickening, deformity, nipple retraction, nipple discharge and nipple eczema
 Follow-up of breast cancer patients
Follow-up of breast cancer patients
 Guidance for biopsy or localization of lesions not visible on ultrasound
Guidance for biopsy or localization of lesions not visible on ultrasound
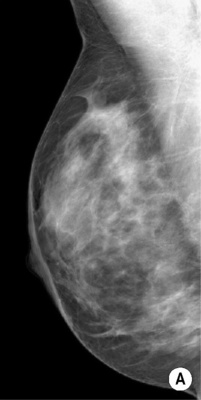
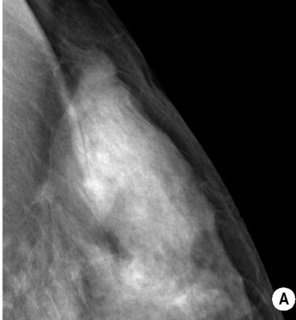
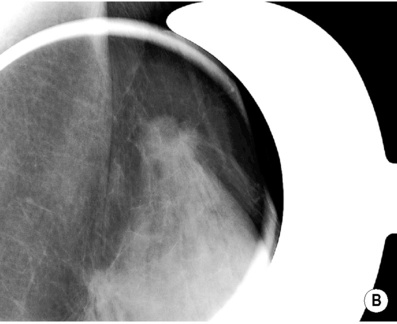
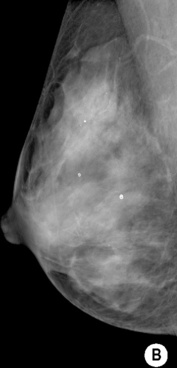
 The XR beam is directed from superomedial to inferolateral (usually at 30–60°)
The XR beam is directed from superomedial to inferolateral (usually at 30–60°)  compression is applied obliquely across the chest wall and perpendicular to the long-axis pectoralis major
compression is applied obliquely across the chest wall and perpendicular to the long-axis pectoralis major
 The only view demonstrating the entire breast tissue on a single image
The only view demonstrating the entire breast tissue on a single image
 Well positioned if: the inframammary angle is demonstrated
Well positioned if: the inframammary angle is demonstrated  the nipple is in profile
the nipple is in profile  the nipple is positioned at the level of the lower border of the pectoralis major, with the muscle across the posterior border of the film at 25–30° to the vertical
the nipple is positioned at the level of the lower border of the pectoralis major, with the muscle across the posterior border of the film at 25–30° to the vertical
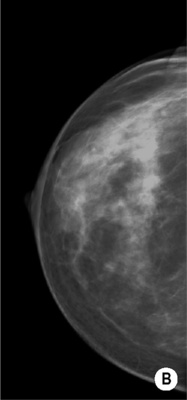
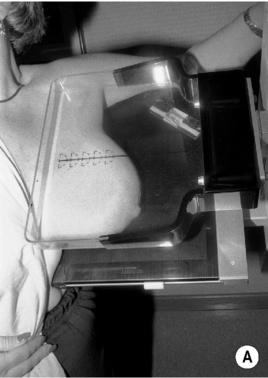
 The XR beam travels from superior to inferior
The XR beam travels from superior to inferior  the breast is pulled forward and away from the chest wall with compression applied from above
the breast is pulled forward and away from the chest wall with compression applied from above
 Well positioned if: the nipple is in profile
Well positioned if: the nipple is in profile  it demonstrates virtually all of the medial tissue and the majority of the lateral tissue (with exclusion of the axillary tail of the breast)
it demonstrates virtually all of the medial tissue and the majority of the lateral tissue (with exclusion of the axillary tail of the breast)  the depth of breast tissue should be < 1cm of the distance from the nipple to the pectoralis major on the MLO projection
the depth of breast tissue should be < 1cm of the distance from the nipple to the pectoralis major on the MLO projection
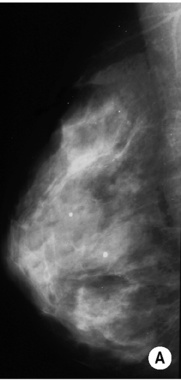
 Localized compression applied with a compression paddle
Localized compression applied with a compression paddle
 It distinguishes a real lesion from superimposition of normal tissues
It distinguishes a real lesion from superimposition of normal tissues  it defines the margins of a mass
it defines the margins of a mass
 The mammography unit is turned through 90° and a mediolateral or lateromedial XR beam used
The mammography unit is turned through 90° and a mediolateral or lateromedial XR beam used
 It distinguishes superimposition of normal structures from real lesions
It distinguishes superimposition of normal structures from real lesions  it increases the accuracy of wire localizations of non-palpable lesions
it increases the accuracy of wire localizations of non-palpable lesions
 Performed in the craniocaudal and lateral projections
Performed in the craniocaudal and lateral projections
 These interrogate areas of microcalcification and can demonstrate ‘teacups’ with benign calcification
These interrogate areas of microcalcification and can demonstrate ‘teacups’ with benign calcification
INTRODUCTION
FIBROCYSTIC CHANGE
DEFINITION
 regression with pregnancy and menopause
regression with pregnancy and menopause  increased risk for developing certain types of cancer (e.g. ductal carcinoma in situ (DCIS))
increased risk for developing certain types of cancer (e.g. ductal carcinoma in situ (DCIS))
BENIGN MASS LESIONS
FIBROADENOMA
DEFINITION
 it often enlarges during pregnancy and regresses after the menopause
it often enlarges during pregnancy and regresses after the menopause  it is the most common cause of a benign solid mass in the breast
it is the most common cause of a benign solid mass in the breast
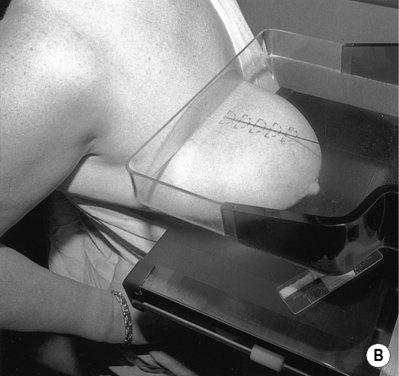
RADIOLOGICAL FEATURES
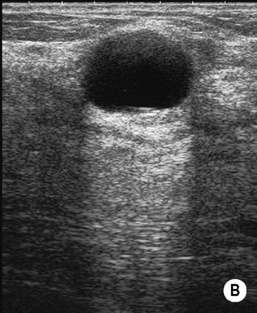
US
 < 25% are locally aggressive requiring clear surgical margins
< 25% are locally aggressive requiring clear surgical margins  large fibroadenomas or those rapidly increasing in size are excised to avoid missing a phyllodes tumour
large fibroadenomas or those rapidly increasing in size are excised to avoid missing a phyllodes tumour
Breast







 T2WI: diffuse high SI (2nd half of cycle): T1WI + Gad: patchy enhancement
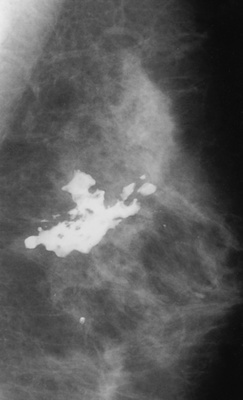
T2WI: diffuse high SI (2nd half of cycle): T1WI + Gad: patchy enhancement diffusely scattered calcifications
diffusely scattered calcifications a ‘teacup’ configuration of calcium within the cystic spaces
a ‘teacup’ configuration of calcium within the cystic spaces common between 20 and 50 years old (peak between 40 and 50 years old)
common between 20 and 50 years old (peak between 40 and 50 years old) perform cytology only if there are suspicious imaging features or if the aspirate is bloodstained
perform cytology only if there are suspicious imaging features or if the aspirate is bloodstained coarse mural curvilinear calcification
coarse mural curvilinear calcification
 they can occur at any age and are often palpable
they can occur at any age and are often palpable on histology it may be reported as normal breast tissue
on histology it may be reported as normal breast tissue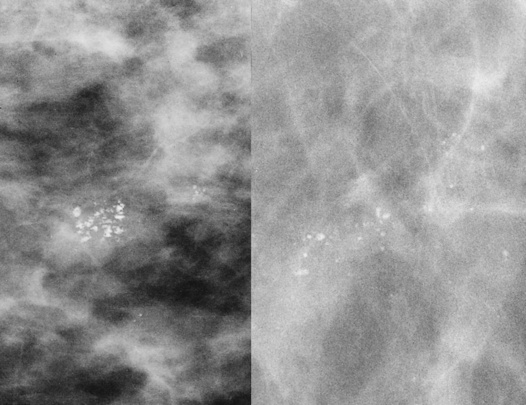
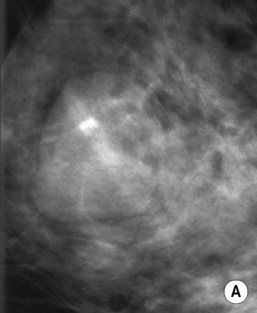
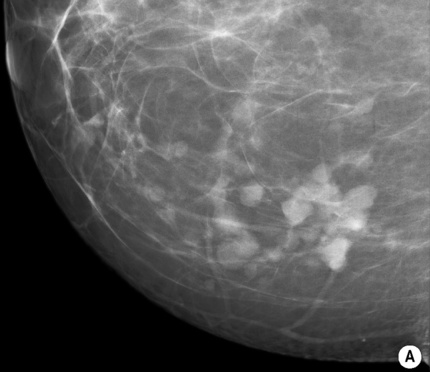
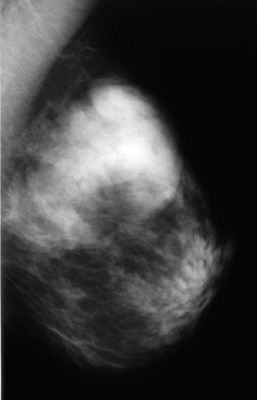
 peak incidence – 3rd decade
peak incidence – 3rd decade  multiple in 10–20%
multiple in 10–20% coarse calcifications may develop (particularly in older women)
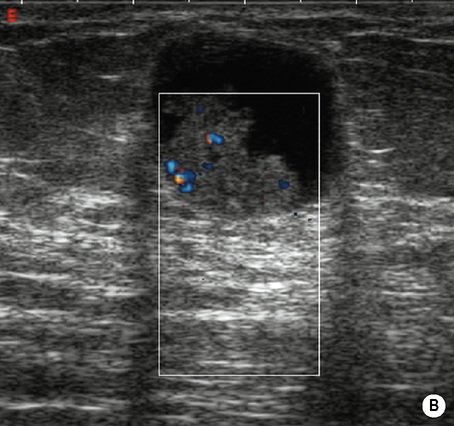
coarse calcifications may develop (particularly in older women) isoechoic or mildly hypoechoic relative to fat ± a thin echogenic pseudocapsule
isoechoic or mildly hypoechoic relative to fat ± a thin echogenic pseudocapsule  a surrounding halo (Mach effect)
a surrounding halo (Mach effect)  displaced normal vessels around the edge of the lesion
displaced normal vessels around the edge of the lesion





