Presentation and Presenting Images
( ▶ Fig. 19.1, ▶ Fig. 19.2, ▶ Fig. 19.3, ▶ Fig. 19.4)
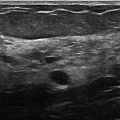
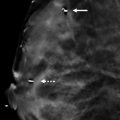
A 52-year-old female with a history of left breast cancer treated with a mastectomy presents for screening mammography.
19.2 Key images
( ▶ Fig. 19.5, ▶ Fig. 19.6, ▶ Fig. 19.7, ▶ Fig. 19.8, ▶ Fig. 19.9)
19.2.1 Breast Tissue Density
The breasts are almost entirely fatty.
19.2.2 Imaging Findings
In the posterior central aspect of the right breast, there is a low-density focal asymmetry ( ▶ Fig. 19.5 and ▶ Fig. 19.6). The digital breast tomosynthesis (DBT) images ( ▶ Fig. 19.7 and ▶ Fig. 19.8) verify that this focal asymmetry has a very faint rim calcification that partially surrounds a fat-containing mass. There is some faint architectural changes around this mass seen on the DBT images that suggest that this is related to the patient’s prior reduction surgery. The outside magnetic resonance (MR) image ( ▶ Fig. 19.9) confirms that this area is composed of fat.
19.3 BI-RADS Classification and Action
Category 2: Benign
19.4 Differential Diagnosis
Fat necrosis at the surgical scar: Characteristic findings are present mammographically after reduction surgery. One of these findings is fat necrosis. The degree of fat necrosis can also vary.
Lipoma: Lipomas are fatty masses that can occur anywhere in the body and have a characteristic thin capsule. The mammographic finding in this case does not share this characteristic finding.
Developing asymmetry: Patients with breast reduction surgery have the same risk of breast cancer as the rest of the population. New or developing masses need to be distinguished from the development of cancer and postsurgical changes. The surgical history combined with the imaging findings and the prior MRI favor this to be postsurgical changes rather than a developing asymmetry of a possible carcinoma.
19.4.1 Essential Facts
Fat necrosis can present as oil cysts, spiculated lesions, focal masses, or calcifications.
During breast-reduction surgery there is redistribution of the breast tissue resulting in characteristic sites of scarring.
Fat necrosis in breast reduction often occurs along the scar lines.
The thin capsule of a lipid cyst of fat necrosis is better seen on DBT due to the decrease in summation artifacts. The DBT images can also reveal scar lines that may extend to the skin surface because of this uncovering effect.
Lipid cysts can have components that are encapsulated fat-containing masses and others that are lined with thin rim-shell calcification.
19.4.2 Management and Digital Breast Tomosynthesis Principles
Similar fat-necrosis changes can be seen in the breast from a lumpectomy and from reduction surgery. The location and distribution of the findings should help to distinguish the origin. Oncoplastic surgery has become more common in the treatment of breast cancer. Some these patients may have a lumpectomy for their cancer treatment combined with reduction mammoplasty. These scars can be more difficult to follow mammographically.
Early changes of fat necrosis, especially when appearing as a spiculated lesion or calcifications, can mimic carcinoma. Occasionally these will require a biopsy to confirm benignity.
All spiculated masses that contain fat should be evaluated and/or strongly correlated with a surgical history before dismissing then as fat necrosis due to surgery. DBT is superior to FFDM for revealing the central fat that can be present in some malignant tumors.
19.5 Further Reading
[1] Freer PE, Wang JL, Rafferty EA. Digital breast tomosynthesis in the analysis of fat-containing lesions. Radiographics. 2014; 34(2): 343‐358 PubMed

Fig. 19.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree