Clinical Presentation
The patient is a 24-year-old female who states that at approximately 2:30 p.m. today, she jumped off a second-floor balcony for fun. The patient states that she landed on her feet on a grassy surface. The patient states that she had immediate onset of low back pain. The patient, at this time, rates that pain at 9 out of 10. She states it is constant and aching in nature and made worse with any movements. The patient denies leg pain, neck pain, paresthesias, or alteration in motor function. The patient states that she has a numb feeling in both hips and has been incontinent of urine.
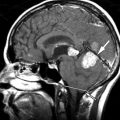
Imaging Presentation
Frontal and lateral radiographs reveal compression of the superior and inferior L2 endplates with bone fragments and anterior and posterior extension of bone compatible with a burst fracture. There is evidence of spinal stenosis at the fracture level from the retropulsed fragment ( Fig. 13-1 ) .

Discussion
Thoracolumbar fractures can be divided into several different types including wedge-compression deformities, flexion-distraction injuries (including Chance [seat belt] fractures) and burst fractures. Approximately 90% of all spinal fractures occur in the thoracolumbar spine with burst fractures comprising 10% to 20% of them).
Burst fractures result from an axial compressive load applied to the spinal column with varying degrees of flexion and/or rotation. There is centripetally oriented disruption of the vertebral body. There is typically a comminuted vertical fracture of the vertebrae originating near the region of the basivertebral vein (88% of cases) with unilateral (38.7%) or bilateral (46.6%) posterior element fractures, anterior wedge deformity (average height loss of 35.4%), increased interpediculate distance (81%), and a retropulsed fragment into the spinal canal, usually from the posterosuperior corner of the vertebral body causing significant narrowing of the spinal canal (average anterosposterior canal compromise of 57.3%). The comminuted fracture of the superior endplate may extend through the vertebral body to connect with a comminuted fracture of the inferior endplate (type A fracture). The more common classic burst fracture (type B) has retropulsion of bone into the spinal canal from a fracture of the posterosuperior endplate with an intact inferior endplate. Type B fractures can lead to acute or late kyphosis. A type C fracture is a rare, isolated fracture of the inferior endplate. Type D fractures are burst fractures with lateral translation, and type E is a unilateral burst fracture.
The T12-L2 vertebrae are the most vulnerable to burst fractures. Above T12, the facet joints limit extension and the costotransverse and costovertebral joints add stability. Below L2, stability is added by the psoas muscle and strong intraspinous and supraspinous ligaments. At the thoracolumbar junction, the facet joints change from coronal to sagittal orientation, and the spine changes from kyphosis to lordosis allowing for greater flexion, extension, and sliding motion during trauma.
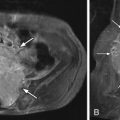
The stability of a thoracolumbar burst fracture is a topic of much debate because stability is the most important determinant for the choice of treatment. Instability can be defined as the loss of the spine’s ability to maintain relationship between the vertebrae under normal physiologic loads. The two-column concept of spinal stability was described by Holdsworth. The spine is divided into anterior and posterior columns. The anterior column consists of the vertebral body, intervertebral disc, and anterior and posterior longitudinal ligaments. The posterior column consists of the pedicles, articular facets, ligamentum flavum, and the interspinous and supraspinous ligaments. A three-column concept was introduced by Denis. In the three-column concept, the posterior column remains the same; however, the Holdsworth’s anterior column is divided into anterior and middle columns. The middle column is in essence the posterior half of Holdworth’s anterior column. The middle column contains the posterior half of the vertebral body, the posterior annulus fibrosis, and the posterior longitudinal ligament ( Fig. 13-2 ) . Holdsworth considered burst fractures to be stable, because although the anterior column (Denis’ anterior and middle columns) was compressed, the posterior column was sufficiently intact. Denis believed that involvement of the middle column was sufficient evidence to consider the fracture to be unstable. Denis’ three-column theory is the more widely used concept today; however, since the advent of magnetic resonance imaging (MRI), evaluation of the posterior ligamentous complex (supraspinous ligament, interspinous ligament, ligamentum flavum, and facet joint capsules) has been used to assess stability of a thoracolumbar burst fracture. If the posterior ligamentous complex demonstrates abnormal increased T2-weighted signal intensity, then this would suggest relative instability. Radiographic signs of instability also include widening of the interspinous distance, translation of greater than 2 mm, kyphosis of greater than 20 degrees, loss of 50% or more, and fractures of the articular processes.

Patients with thoracolumbar burst fractures present with back pain and/or back tenderness on palpation. Neurologic injury from burst fractures is common, seen in nearly two thirds of patients. Because the spinal cord terminates at the same level of typical thoracolumbar fractures, patients can present with bowel and bladder signs and decreased movement/sensation in the lower extremities.
Discussion
Thoracolumbar fractures can be divided into several different types including wedge-compression deformities, flexion-distraction injuries (including Chance [seat belt] fractures) and burst fractures. Approximately 90% of all spinal fractures occur in the thoracolumbar spine with burst fractures comprising 10% to 20% of them).
Burst fractures result from an axial compressive load applied to the spinal column with varying degrees of flexion and/or rotation. There is centripetally oriented disruption of the vertebral body. There is typically a comminuted vertical fracture of the vertebrae originating near the region of the basivertebral vein (88% of cases) with unilateral (38.7%) or bilateral (46.6%) posterior element fractures, anterior wedge deformity (average height loss of 35.4%), increased interpediculate distance (81%), and a retropulsed fragment into the spinal canal, usually from the posterosuperior corner of the vertebral body causing significant narrowing of the spinal canal (average anterosposterior canal compromise of 57.3%). The comminuted fracture of the superior endplate may extend through the vertebral body to connect with a comminuted fracture of the inferior endplate (type A fracture). The more common classic burst fracture (type B) has retropulsion of bone into the spinal canal from a fracture of the posterosuperior endplate with an intact inferior endplate. Type B fractures can lead to acute or late kyphosis. A type C fracture is a rare, isolated fracture of the inferior endplate. Type D fractures are burst fractures with lateral translation, and type E is a unilateral burst fracture.
The T12-L2 vertebrae are the most vulnerable to burst fractures. Above T12, the facet joints limit extension and the costotransverse and costovertebral joints add stability. Below L2, stability is added by the psoas muscle and strong intraspinous and supraspinous ligaments. At the thoracolumbar junction, the facet joints change from coronal to sagittal orientation, and the spine changes from kyphosis to lordosis allowing for greater flexion, extension, and sliding motion during trauma.
The stability of a thoracolumbar burst fracture is a topic of much debate because stability is the most important determinant for the choice of treatment. Instability can be defined as the loss of the spine’s ability to maintain relationship between the vertebrae under normal physiologic loads. The two-column concept of spinal stability was described by Holdsworth. The spine is divided into anterior and posterior columns. The anterior column consists of the vertebral body, intervertebral disc, and anterior and posterior longitudinal ligaments. The posterior column consists of the pedicles, articular facets, ligamentum flavum, and the interspinous and supraspinous ligaments. A three-column concept was introduced by Denis. In the three-column concept, the posterior column remains the same; however, the Holdsworth’s anterior column is divided into anterior and middle columns. The middle column is in essence the posterior half of Holdworth’s anterior column. The middle column contains the posterior half of the vertebral body, the posterior annulus fibrosis, and the posterior longitudinal ligament ( Fig. 13-2 ) . Holdsworth considered burst fractures to be stable, because although the anterior column (Denis’ anterior and middle columns) was compressed, the posterior column was sufficiently intact. Denis believed that involvement of the middle column was sufficient evidence to consider the fracture to be unstable. Denis’ three-column theory is the more widely used concept today; however, since the advent of magnetic resonance imaging (MRI), evaluation of the posterior ligamentous complex (supraspinous ligament, interspinous ligament, ligamentum flavum, and facet joint capsules) has been used to assess stability of a thoracolumbar burst fracture. If the posterior ligamentous complex demonstrates abnormal increased T2-weighted signal intensity, then this would suggest relative instability. Radiographic signs of instability also include widening of the interspinous distance, translation of greater than 2 mm, kyphosis of greater than 20 degrees, loss of 50% or more, and fractures of the articular processes.