CALCIFICATION, OSSIFICATIONS, MATRICES, RADIODENSE FOREIGN BODIES, AND THEIR MIMICS
KEY POINTS
- Calcification, ossification, and the presence of a matrix are frequently crucial to the diagnostic process.
- Calcification, ossification, and matrices are more easily and accurately appreciated on computed tomography.
- Radiodense foreign bodies, blood, impacted secretions, and reactive changes may mimic calcification and ossification. This may impede or enlighten the diagnostic process.
- Protocols for imaging approaches to clinical problem solving must take into account the relative strength of computed tomography over magnetic resonance imaging for identifying calcification, ossification, matrices, and foreign bodies that are radiodense on computed tomography.
The presence of calcification, ossification, or their mimics is often not important if such findings are physiologic or just part of the natural aging process (Fig. 12.1). Sometimes, calcification, when present, is not a critical factor in evaluating a related disease process (Fig. 12.2). However, sometimes calcification can prove crucial for differential diagnosis and medical decision making (Fig. 12.3). The cause of some calcifications often remains unknown. In all cases, calcifications and all calcified matrices are better seen and appreciated for what they are on computed tomography (CT) and plain films than magnetic resonance (MR), and this becomes a critical issue for planning the proper imaging approach to clinical problems. The latter point is the main issue of interest in this introductory material. Calcifications are marginally appreciable on ultrasound.
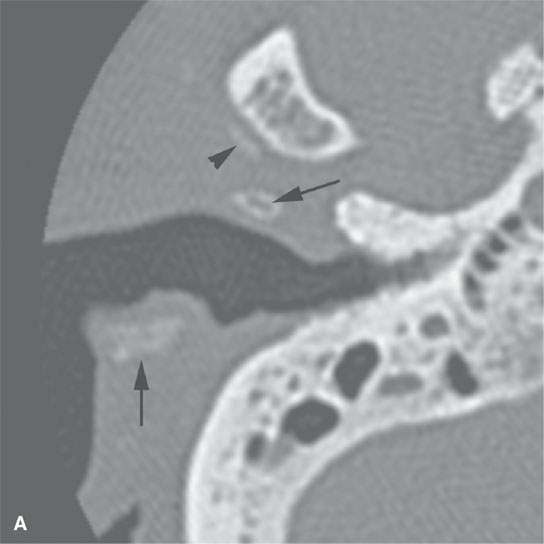
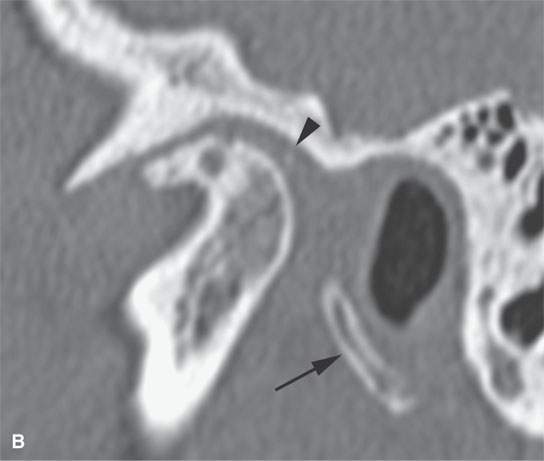
FIGURE 12.1. Computed tomography at bone windows showing calcification of the ear cartilage, a normal variant (arrows), and dystrophic temporomandibular joint disc and capsule calcification (arrowheads).
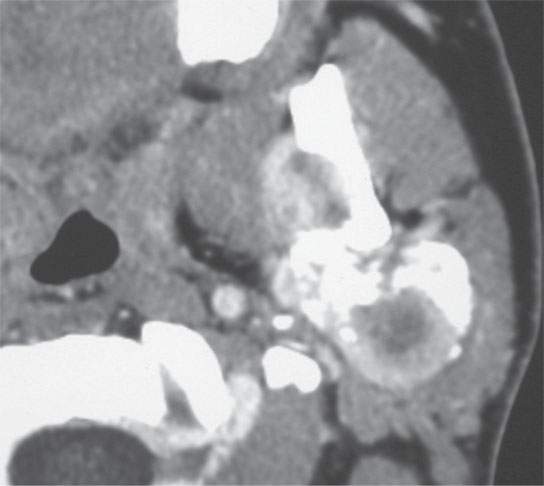
FIGURE 12.2. Contrast-enhanced computed tomography of a partially calcified synovial cell sarcoma where the likely dystrophic tumoral calcification is not helpful in differential diagnosis.
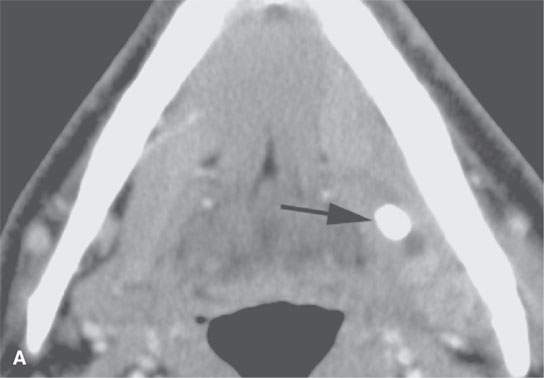

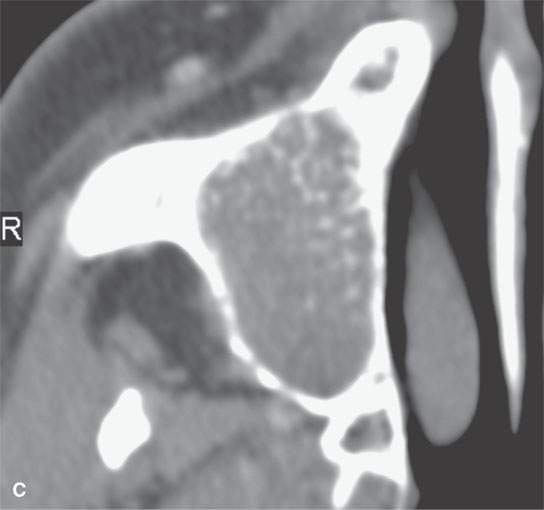
FIGURE 12.3. Examples where magnetic resonance would likely not make as good a diagnosis based on recognizing calcification and mineralization as computed tomography (CT) and where this information is critical to proper diagnosis. A: Contrast-enhanced CT of low-grade sialoadenitis presenting as a submandibular mass—the stone (arrow) and ductal dilatation is obvious on CT and might be more difficult to detect with magnetic resonance imaging (MRI) or ultrasound. B, C: CT makes the specific diagnosis of chondrosarcoma of the nasal septum (B) and chondroblastoma or at least a chondroid matrix lesion (C) that is unlikely to have been as apparent a diagnosis on MRI.
THINGS THAT MAY LOOK CALCIFIC BUT ARE NOT
The range of CT density that might appear on images as calcific is wide. Sometimes, dense keratin debris in lymph nodes, densely desiccated secretions, or metals other than calcium manifest a similar density, signal intensity, or pattern of echogenicity— things that may look like calcifications but are not that at all (Figs. 12.4A,B). Small metallic foreign bodies and even wood can mimic calcific density (Fig. 12.5) on CT.1 Focal areas of contrast enhancement and even normal vessels may mimic or mask calcification from accurate observation. Acute or subacute blood products can be mistaken for calcification (Fig. 12.5B). Sometimes, the foreign bodies are actually calcified even though they originate extrinsically; this appearance may evolve over time (Fig. 12.6). It is particularly difficult to recognize foreign bodies on magnetic resonance imaging (MRI) compared to CT; however, MRI may provide clues to their nature. The variations that such findings can create on MRI can be even more confusing (Fig. 12.7).

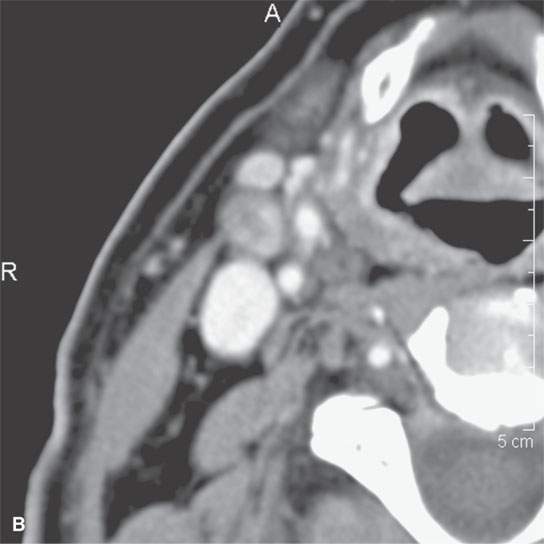
FIGURE 12.4. Examples of keratin and other “debris” mimicking calcification. A: Contrast-enhanced computed tomography (CECT) of normal variant of impacted high-density foci of material in tonsillar crypts. B: CECT of nodes surgically proven to contain high-density keratin debris and no calcification following radiotherapy.
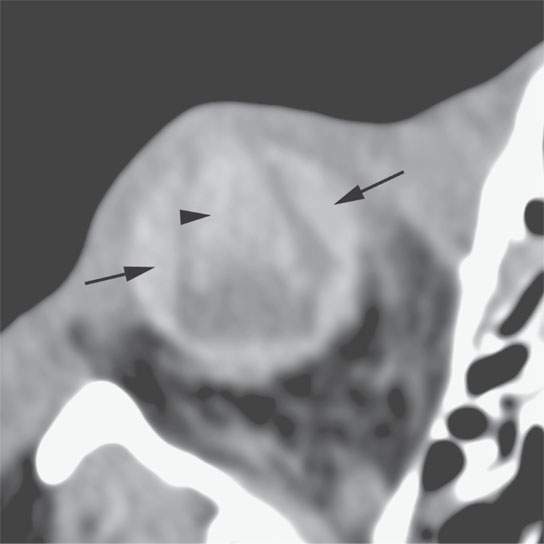
FIGURE 12.5. Computed tomography of choroidal hemorrhage (arrows) as well as anterior and posterior chamber and vitreous hemorrhage that could be a calcification or otherwise mineralized foreign body (arrowhead). Compare this figure with Figure 12.16.
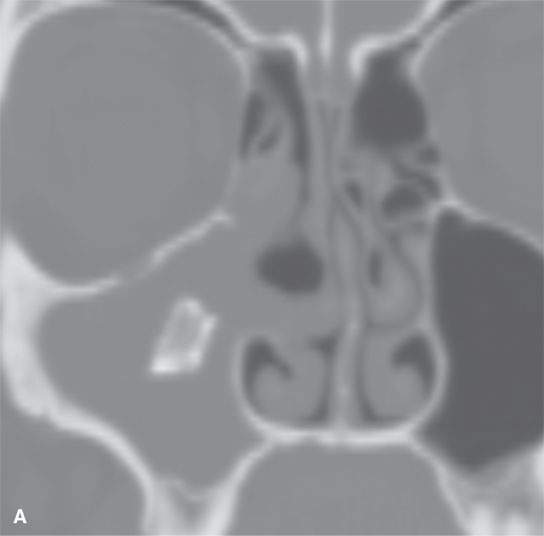


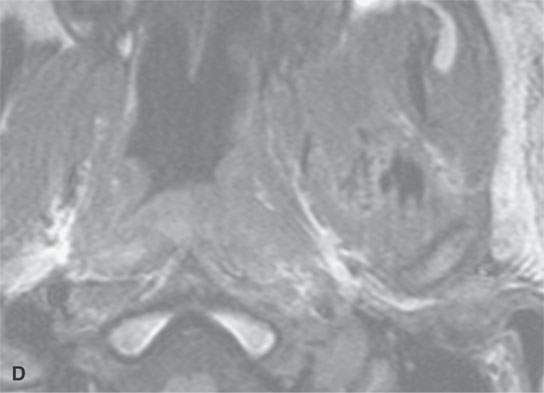
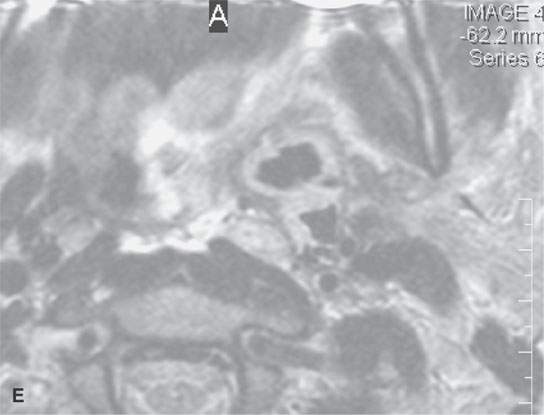
FIGURE 12.6. Calcified foreign bodies. A: Computed tomography (CT) of calcified surgical material that incited this chronic sinusitis left after an endoscopic sinus surgery procedure. B–E: Non–contrast-enhanced CT and magnetic resonance imaging (MRI) of a patient who had a piece of a fence post penetrate from the orbit to the deep facial soft tissues. In (B), the air pattern shows the wood. Weeks later in (C), the foreign body has mineralized. In (D) and (E), the MRI does not really provide as definitive overall evaluation of the situation, but is does nicely demonstrate the surrounding soft tissue response.
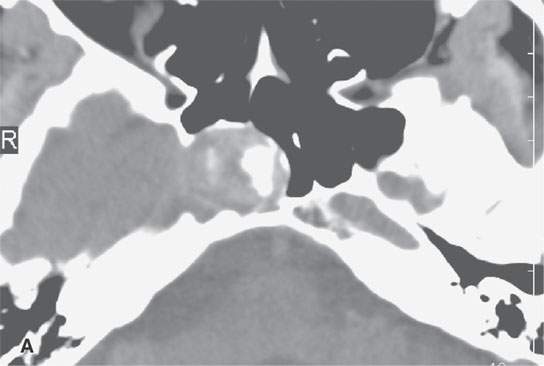
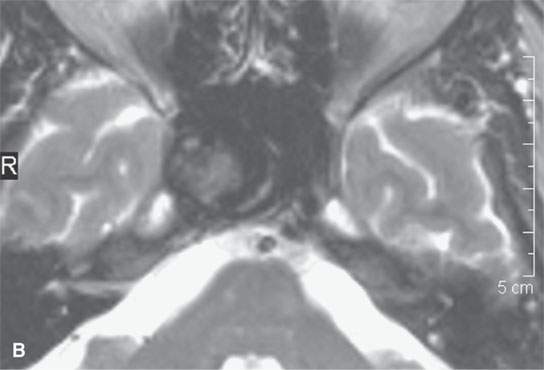
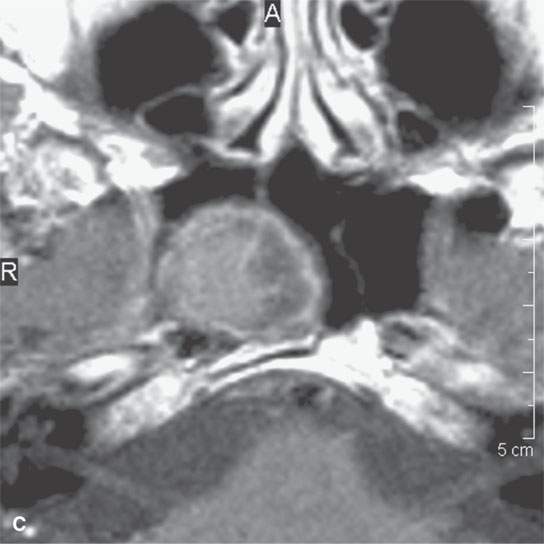
FIGURE 12.7. Cavernous segment aneurysm. The calcification suggesting wall and mural thrombus calcification is obvious on computed tomography. On the magnetic resonance imaging in (B) and (C), the findings are more ambiguous.
CALCIFICATION AS SEEN ON COMPUTED TOMOGRAPHY AND MAGNETIC RESONANCE IMAGING
Calcification and ossification are often very difficult to recognize on MR studies as such, but calcification can be anticipated in certain situations. A focal or diffuse area of markedly diminished signal intensity or signal void on all pulse sequences suggests calcification, ossification, fibrosis, or very chronic blood products (Fig. 12.8). Other possible explanations for such decreased signal include flow void, air, surgical clip, foreign body (Figs. 12.6 and 12.9), or other very proton poor substance or at least something lacking enough mobile protons to create a signal (Fig. 12.10). Small foci of calcification or ossification (several millimeters) are very likely to go unnoticed on standard spin echo (SE) sequences depending on the nature of the surrounding tissues. Gradient echo techniques can improve the rate of detection, or at least suspicion, of calcifications since these sequences are highly sensitive to the local field distortions produced by calcium-related susceptibility effects (Fig. 12.11 and Chapter 2). Gradient echo and susceptibility-weighted sequences are useful in the brain for this purpose, but their value is sometimes limited in the extracranial head and neck because these sequences are more prone to magnetic susceptibility artifacts that variably degrades image quality outside the brain depending on the adjacent anatomy and its vulnerability to susceptibility artifacts such as a mandible full of metal due to dental appliances.
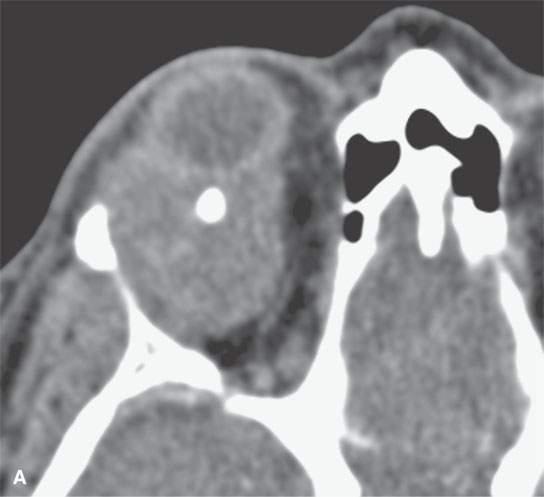
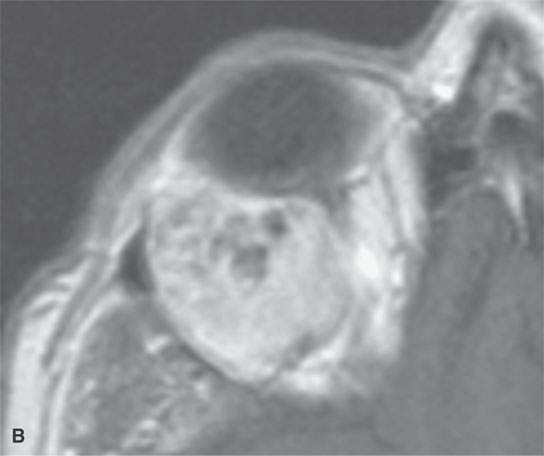
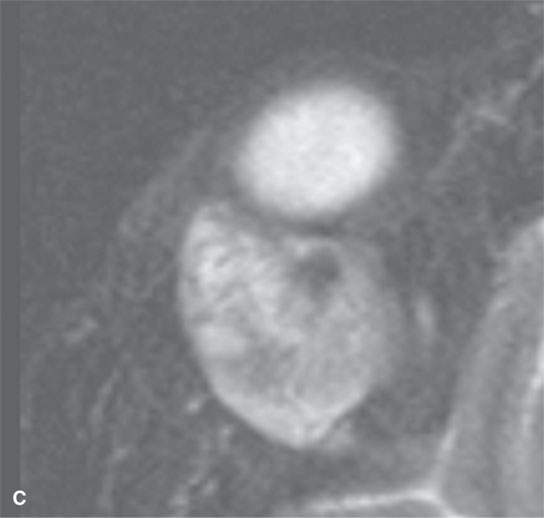
FIGURE 12.8. Adenoid cystic carcinoma of the lacrimal gland with possible calcification in impacted mucoid material or dystrophic calcification. The nature of the signal void is less clear on the contrast-enhanced T1-weighted magnetic resonance imaging (MRI) in (B) and the T2-weighted MRI in (C). In this case, the presence of a calcification adds nothing to the diagnostic process.
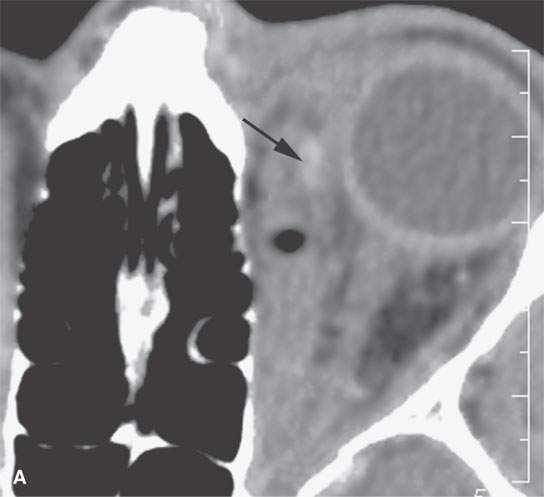

FIGURE 12.9. Penetrating orbital trauma. A:The wood fragment (arrow) is the same density as expected from calcification seen in the non–contrast-enhanced CT. Note the gas. B: In the T2-weighted magnetic resonance imaging, both the foreign body (arrow) and gas show as signal voids an obviously more ambiguous and less helpful scenario than with CT.
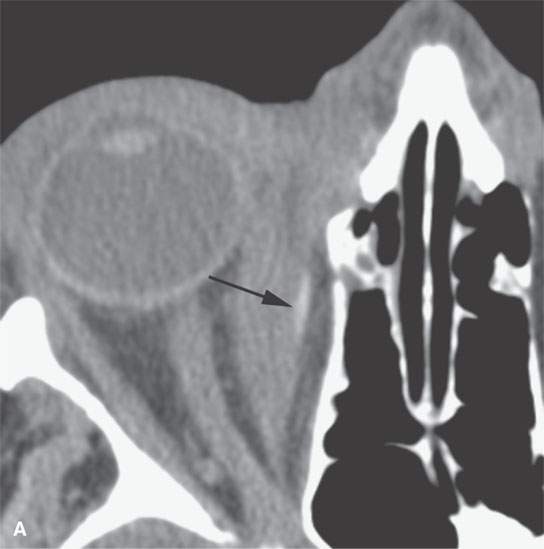
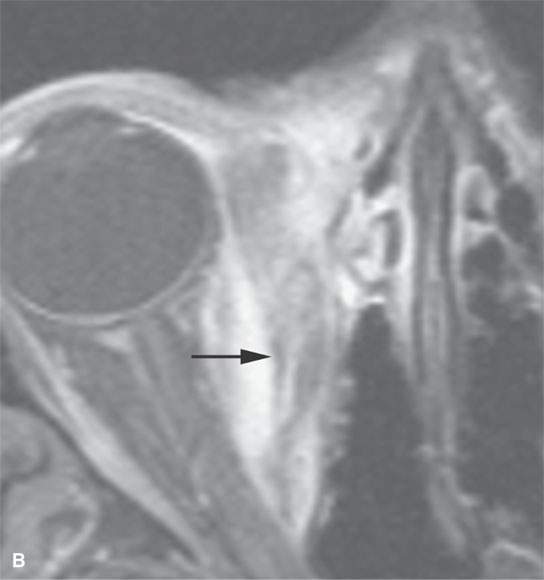
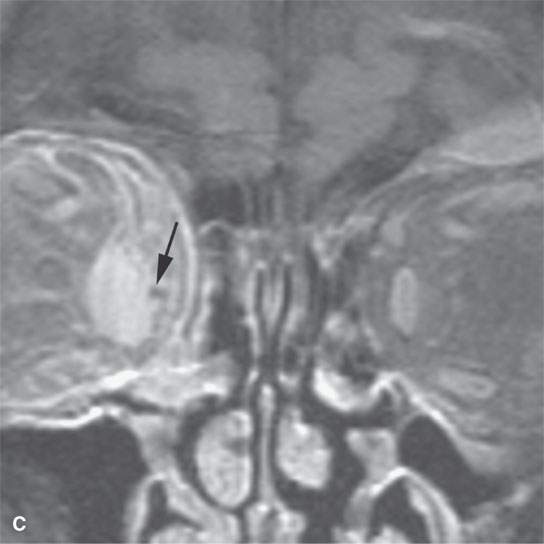
FIGURE 12.10. Penetrating plant material mimics a calcified foreign body on the computed tomography in (A). It is not really visible (arrow) on the fat-suppressed T1-weighted magnetic resonance imaging in (B), but it can be seen (arrow) as a void on the coronal T2-weighted image in (C).
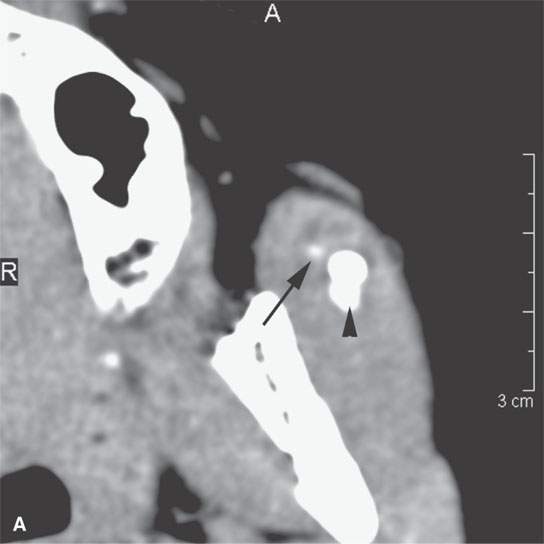
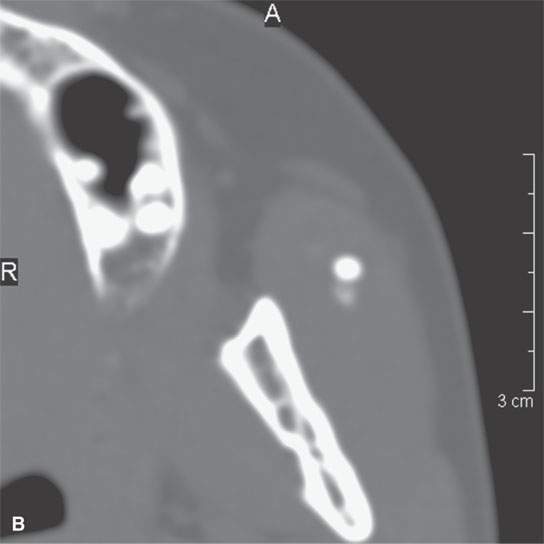
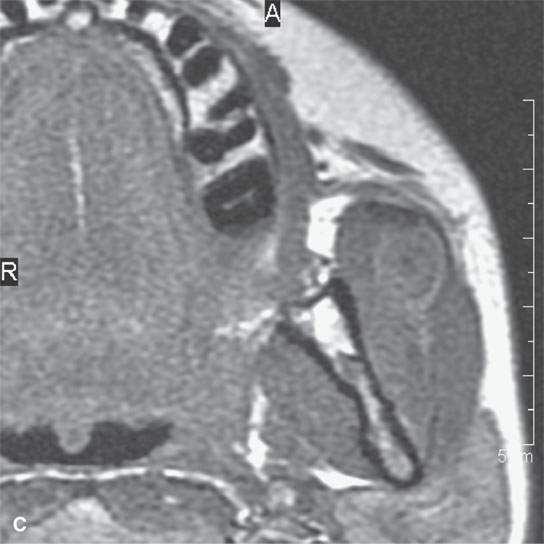
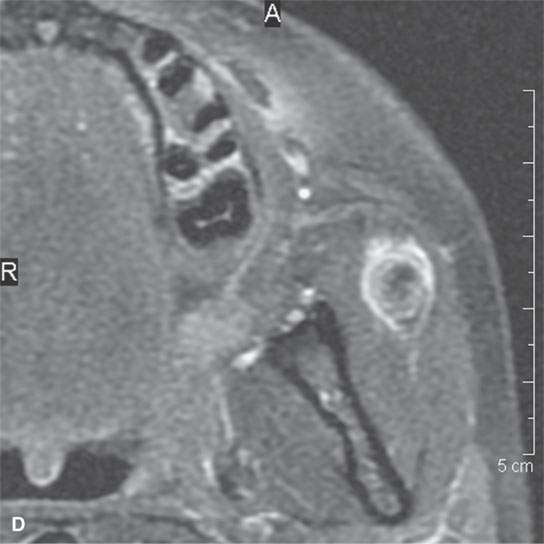
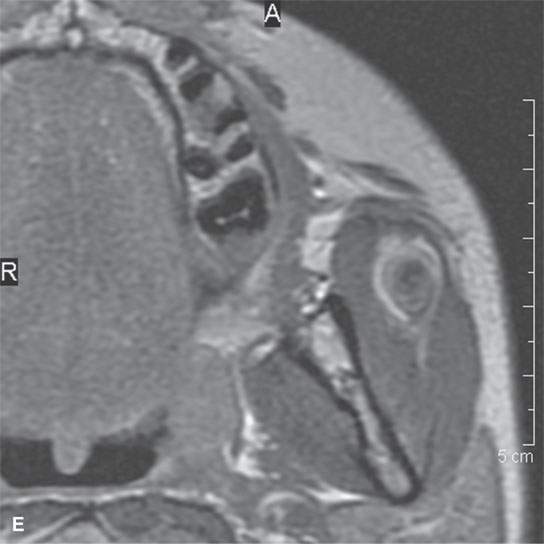

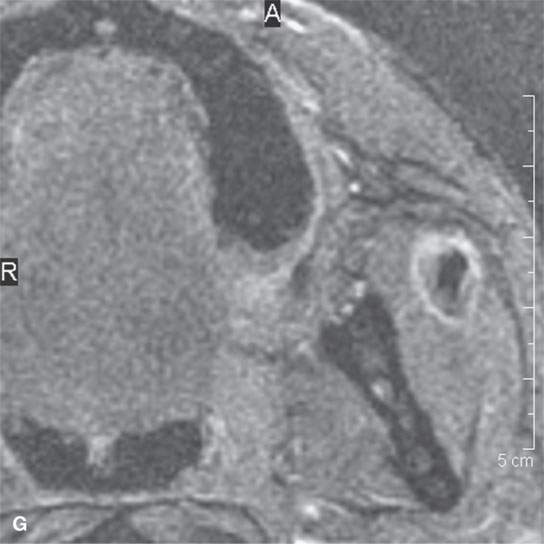
FIGURE 12.11. Appearance of calcification on computed tomography (CT) and magnetic resonance imaging (MRI) in a small vascular malformation presenting as a cheek mass. The recognition of the calcification is useful in the differential diagnosis. Contrast-enhanced CT (A) shows enhancement (arrow) and the calcification (B). MRI including non–contrast-enhanced T1 weighted (C), contrast-enhanced fat-suppressed T1 weighted (D), contrast-enhanced T1 weighted (E), T2 weighted (F), and gradient echo (G), all showing the calcifications as some degree of a signal void with some recognizable field distortion in the calcification in (F) as a clue to is “metallic” nature.
If the diagnosis is already known, then the MR depiction of the process may be adequate or yield more information than the CT. However, whenever such suggestive areas of consistently diminished signal are present and the nature of the low-intensity area is important for treatment or diagnostic purposes, a CT should be done to clarify the situation (Fig. 12.12).

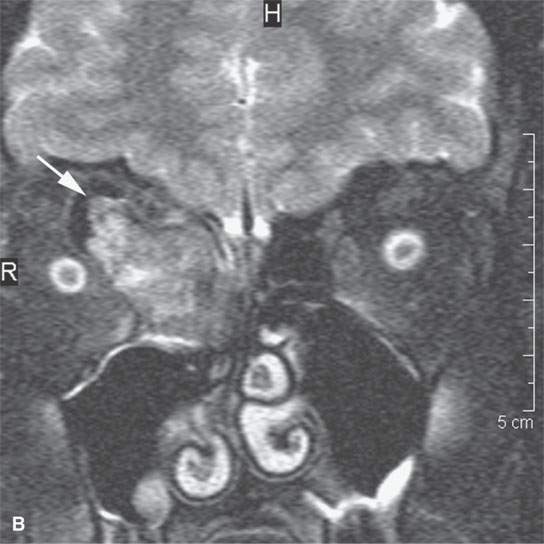
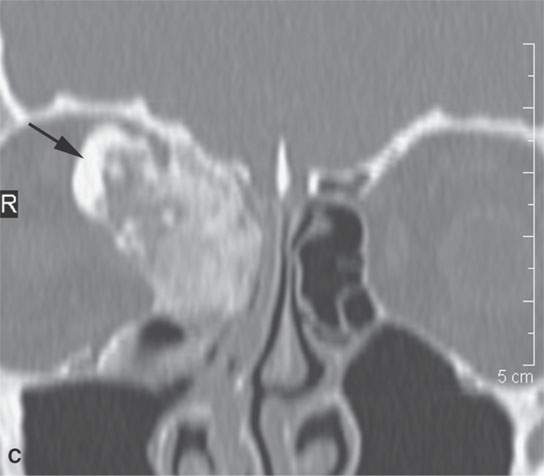

FIGURE 12.12. The obvious area of signal void is seen on the magnetic resonance images (T1-weighted non–contrast enhanced in A and T2 weighted in B by the arrows), but the nature of the remaining matrix and true nature of the signal void area is not clear (arrow) until viewing the non–contrast-enhanced computed tomography in (C) and (D). This was diagnosed pathologically as an osteoma with elements of osteoblastoma.
Calcium may also be the cause of areas of increased signal intensity on T1-weighted images. This has been observed in patients with neurofibromatosis as areas of increased signal intensity in the basal ganglia (Fig. 12.13).2 One group2has demonstrated that the effect is probably related to the physical state of the calcium in these regional areas of disordered brain maturation and thus altered MR signal. A similar situation may exist in calcium in solution in a fluid collection.
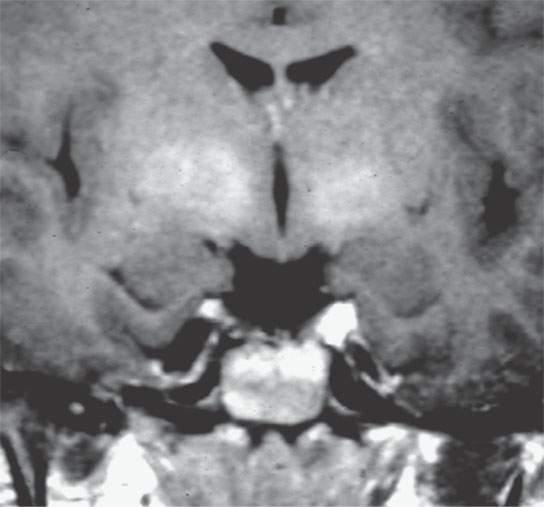
FIGURE 12.13. TI-weighted magnetic resonance showing high-attenuation areas in the globus pallidus in a patient with neurofibromatosis type I.
In general, the calcifications and areas of ossification on CT and plain films are very easily recognized as areas of discreet increased density with a morphology conforming to the source of their origin (Figs. 12.14 and 12.15). Occasionally, they may be confused with retained noncalcific foreign bodies, acute blood products, desiccated impacted secretions, or focal contrast enhancement (Fig. 12.16 compared to 12.5). If important to diagnosis, pre- and postcontrast CT images may be necessary. Currently, this is not a routine in any CT protocol except the initial evaluation of a potential retinoblastoma.
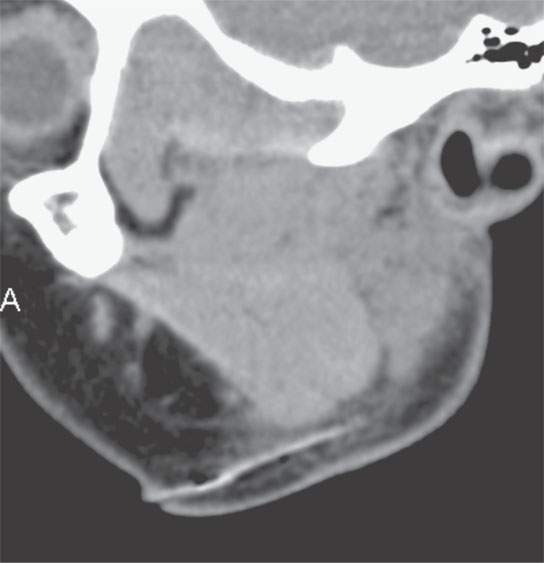
FIGURE 12.14. Contrast-enhanced computed tomography that shows a penetrating pine needle that likely would not have been visible on magnetic resonance imaging. The morphology is the clue to the nature of the material; in this situation, its density is not helpful.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








