Your children have finally learned to get their own cereal in the morning. But yikes, what is that stuff on the kitchen floor? You start to reach for a paper towel. Actually, that stuff looks kind of sharp. You’re going to need a broom and dustpan. Analyzing calcifications can be like deciding how to deal with a dirty kitchen floor. Do you use a paper towel because the debris is just stuff, or do you go to the closet to get the dustpan because the detritus is sharp like pieces of glass? A good way to approach calcifications is to think about the sharpness of the edges. The sharper the calcifications, the more worried you should be. So … when you look at calcifications, would you go for the paper towel or the dustpan?
As radiologists, we have an opportunity to detect and diagnose curable breast cancer. This is especially true for ductal carcinoma in situ (DCIS); the 10-year survival rate is 98%. Once invasion occurs, the prognosis is less sure. Calcifications are the earliest sign of breast cancer, and their accurate assessment is potentially lifesaving.
Calcifications Versus Artifact
The first step in evaluating suspected calcifications is to make sure that they represent true calcifications rather than artifact. Deodorant is radiopaque because it contains aluminum compounds. It has a characteristic appearance and is typically present in the axilla. Zinc oxide in ointments and talc can mimic calcifications, especially when collected in moles and other skin lesions ( Fig. 6-1 ). Sand on the skin, tattoo pigment, and metallic artifacts from gunshot wounds or prior surgical procedures ( Fig. 6-2 ) can also resemble calcifications, as can pick-off artifact or dust on screens in film-screen mammography.


Describing Calcifications
Calcifications are described by distribution, morphology, laterality, and location. The key to evaluating calcifications is to accurately define their distribution and morphology. Careful analysis of these features and comparison with prior studies allows us to estimate the level of suspicion of calcifications and determine how they should be managed. Remember that assessment of calcifications is only as good as the quality of the magnification views.
Distribution
The BI-RADS lexicon defines distribution modifiers ( Fig. 6-3 ) that range from the least suspicious (diffuse/scattered) to the most suspicious (segmental).

A ductal system in the breast resembles the branches of the tree. Ductal systems vary greatly in size and can extend over quite a large region.
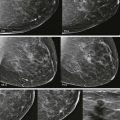
The large majority of breast cancers develop within a single ductal system. Therefore, calcifications of almost any morphologic type that are judged to be in one ductal system are suspicious for DCIS, especially if their distribution is segmental or linear ( Fig. 6-4 ). If widely separated calcifications of suspicious morphologic appearance are visualized, particularly within dense tissue, they may still be malignant. Because they are sparse, the initial impression may be that they are scattered; however, calcifications that appear scattered within a segment may still be suspicious. If you connect the dots and the resulting distribution is linear or segmental, biopsy should be considered ( Fig. 6-5 ).


On the other end of the spectrum, the lowest suspicion distribution is bilateral scattered calcifications. Benign processes producing calcifications in the breast frequently involve more than one duct system, often in both breasts. This most commonly occurs with round & punctate calcifications that develop within lobules; when scattered and bilateral, these calcifications are typically benign ( Fig. 6-6 ).

Morphology
The BI-RADS lexicon divides calcifications by morphology into two categories based on their risk of malignancy: (1) typically benign and (2) suspicious ( Table 6-1 ).
| LIKELIHOOD OF MALIGNANCY | MORPHOLOGY |
|---|---|
| Typically benign |
|
| Suspicious |
|
Typically Benign Calcifications
Typically benign calcifications are classified by their etiology (e.g., suture, dermal) except for round & punctate. These are nearly always recognized as benign on screening mammography, although occasionally, recall for magnification or tangential views may be needed to confirm their benign status.
Dermal Calcifications
Benign dermal calcifications occur in folds where women sweat—in the inframammary fold, cleavage, and axilla ( Fig. 6-7 ). Because dermal calcifications are fixed in the skin, they retain the same relationship to each other in each view; this is called the “tattoo sign” ( Fig. 6-8 ). Dermal calcifications are also common in scar tissue. A tangential view may be needed to confirm that calcifications have a dermal location.


Vascular Calcifications
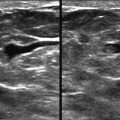
Arterial calcifications usually produce parallel tracks of linear calcifications that follow the course of a vessel and can almost always be dismissed as benign. Occasionally, when early, they may mimic fine pleomorphic calcifications that are in a linear distribution ( Fig. 6-9 ).

Coarse Popcorn-like Calcifications
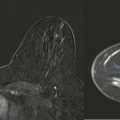
Coarse, popcorn-like calcifications are due to degenerating fibroadenomas. Although this late stage is usually obviously benign, the earlier appearance of coarse heterogeneous calcifications is less specific. Calcifications often develop first at the periphery of a fibroadenoma and become increasingly coarse and coalescent over time ( Fig. 6-10 ; see Fig. 6-20 ).

Large Rod-like (Secretory) Calcifications
Large rod-like calcifications are ductal in origin. They are typically large (≥1 mm in diameter), well-defined linear calcifications oriented toward the nipple ( Fig. 6-11 ). They are often bilateral and symmetric but may be few in number and affect a single ductal system early in their development. They are usually intraluminal with a rod shape but may also be periductal, in which case they are cigar-shaped with a lucent center. Think of secretory calcifications as dashes with no dots. They are due to involution of the duct, so they are usually seen 10 to 20 years after menopause. If you identify what you think are secretory calcifications in a young woman who has not undergone early menopause, think twice!

Eggshell or Rim Calcifications
These calcifications are easy to recognize and are nearly always due to fat necrosis. Injury to a fat lobule results in healing by liquefaction necrosis, which causes an inflammatory response at the margin. Calcifications form at this inflamed margin, and can disappear after a number of years.
Injury can affect a single fat lobule, resulting in small fat necrosis calcifications ( Fig. 6-12 ). For those of you who learned Latin prior to medical school, this is also called liponecrosis microcystica. These calcifications are typically due to incidental trauma, such as an encounter with a soccer ball when playing with your kids. Larger areas of fat necrosis can also occur (liponecrosis macrocystica) (see Fig. 6-12 ). This type is often due to recallable trauma, like a motor vehicle collision or an encounter with a surgeon.

Recognition of the central lucency within calcifications is important in establishing them as benign. Although other types of calcifications may also have lucent centers, they are most accurately described by their specific type (e.g., dermal or large rod-like), rather than as lucent centered.
Dystrophic Calcifications
These benign calcifications are typically seen after surgery, trauma, or radiation. They are often irregular in shape but too large to be considered suspicious for malignancy ( Fig. 6-13 ). They frequently have lucent centers ( Box 6-1 ).

- •
Dermal
- •
Large rod-like (secretory)
- •
Rim or eggshell
- •
Dystrophic
Milk of Calcium
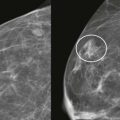
Milk of calcium is one type of benign calcification due to fibrocystic change (FCC). When the fluid-filled lobule is enlarged and calcium forms within it, the calcium can form layer in the dependent part of the lobule ( Fig. 6-14 ). On the CC view, this is like looking down on sugar that has settled to the bottom of a glass of iced tea. The calcifications are powdery and spread out. They may even be difficult to identify. No linear particles should be present on the CC view. On the ML view, this is like looking at the sugar from the side of the iced tea glass. The calcifications layer and form a line that may have a curved bottom (“tea-cupped” appearance). The mediolateral oblique (MLO) view is in between the CC and ML views, so the calcifications may also layer on this view. When patients are recalled from screening, magnification views should be obtained in the CC and ML projections. Although change in morphologic appearance between the CC and ML magnification views is the first clue, layering of most if not all of the calcifications on the ML view is the key to diagnosis.

Suture Calcifications
These calcifications are due to foreign body reaction to suture material after a surgical procedure. They are most common in the radiated breast. The typical appearance is regular lines or circles of calcifications; calcified knots are frequently seen as well. Suture calcifications are most often seen with catgut suture material. With the increased use of silk sutures, they are less frequently encountered than in the past.
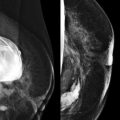
Round & Punctate Calcifications
Round calcifications are typically uniform in size (≥0.5 mm) and very round—like peas in a pod ( Fig. 6-15 ). Punctate calcifications are similar but smaller (<0.5 mm). Round & punctate calcifications usually develop within lobules (see Fig. 6-15 ). The differential diagnosis of lobular calcifications is broad; they are most commonly due to FCC. FCC results in an increase in fluid and sometimes debris within the lobules. Debris can then calcify.