Carcinoma of Unknown Primary
Todd M. Blodgett, MD
Alex Ryan, MD
Hesham Amr, MD
Key Facts
Terminology
Metastatic cancer without known site of origin; histology inconsistent with known tumors from organ biopsied
Imaging Findings
Most common site: Upper aerodigestive tract, specifically lung
Gastrointestinal and urogenital tract also common
Squamous cell: Primary most often in tonsils, nasopharynx
Adenocarcinoma: Primary most often in thorax, GI tract, urogenital tract
Likelihood of primary detection with PET/CT: 25-40%; CT: 25%
FDG PET provides whole-body survey
PET may commonly reveal “missed primary” rather than unknown primary in true sense, i.e., following complete work-up
Small study showed PET/CT more sensitive than PET alone, with 53% detection rate for occult cancers missed by other techniques
Top Differential Diagnoses
Physiologic Activity
Inflammation
Infection
Diagnostic Checklist
In patient with CUP, perform conventional laboratory workup and combination of imaging studies, with consideration of PET/CT
TERMINOLOGY
Abbreviations and Synonyms
Carcinoma of unknown primary (CUP)
Includes undifferentiated carcinomas in addition to adenocarcinoma
Definitions
Metastatic cancer without known site of origin
Histology inconsistent with known tumors from organ biopsied
Also defined as presence of metastatic disease for which site of primary lesion remains unidentified
Remains unknown despite review of
Medical history
Physical exam
Lab work (CBC, kidney/liver/pancreas function tests, PSA, U/A)
Imaging evaluation usually includes CXR, abdominopelvic CT, mammography
After common imaging investigation, 20-27% of primaries remain unidentified
IMAGING FINDINGS
General Features
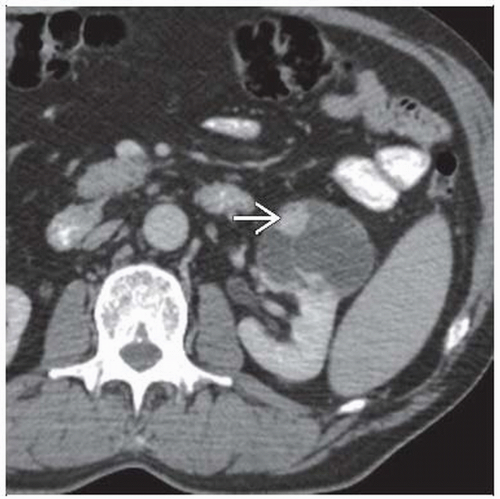
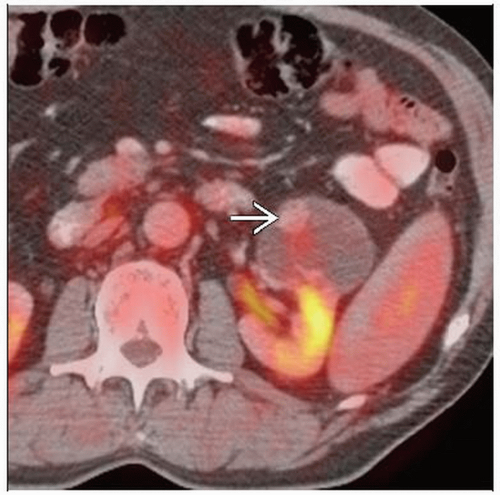
Best diagnostic clue: Detection of focal intense FDG activity in potential primary organ or site in patient with biopsy-proven carcinoma of unknown primary
Location
Most common site: Upper aerodigestive tract, specifically lung
May also have abnormal mediastinal nodes
Consider accessible areas for subsequent confirmatory biopsy
Gastrointestinal and urogenital tract also common
Appear as focal areas of intense FDG activity in bowel rather than linear areas of physiologic activity
Look carefully at kidneys as a small renal cell carcinoma may be missed or obscured by physiologic excretory FDG activity
Frequency of metastases by location
Involvement of supraclavicular and low cervical lymph nodes may be suspicious for primary in chest or abdomen
Associated with poorer prognosis than metastases of upper neck levels
Squamous cell
Primary most often in tonsils &/or nasopharynx
Look for asymmetrical focal intense FDG activity on PET and PET/CT
Adenocarcinoma
Primary most often in thorax, GI tract, or urogenital tract
Size: Varies from small (< 1 cm) to several centimeters
Morphology: Range of morphologies, including no obvious findings on CT to a several centimeter mass
Imaging Recommendations
Best imaging tool
Likelihood of primary detection with PET/CT: 25-40%; CT: 25%
FDG PET provides whole-body survey
Patients with head/neck mets of non-SCCA histology should not be limited to imaging of head/neck area only
Whole-body imaging has been proven beneficial
Typical workup for patients with SCCA lymph node mets
Thorough physical exam including transnasal fibre-endoscopy of nasal cavity, nasopharynx, oropharynx, hypopharynx, larynx
CECT or CEMR of neck and PA/Lat CXR
Panendoscopy includes rigid esophagoscopy, tracheobronchoscopy, hypopharyngoscopy, laryngoscopy
Inspection/palpation of oropharynx and oral cavity, with biopsies taken from suspicious mucosal areas
Ipsilateral tonsillectomy if no primary detected during panendoscopic random biopsies
FDG PET often used when all of the above approaches have failed; may also direct biopsies
Non-SCCA histology has similar workup, with CT of chest and abdomen along with pelvic/prostate examinations
Mammography very low yield; rarely do patients with CUP have primary mass in breast
Protocol advice
Consider PET/CT evaluation, although currently not routinely used for CUP
Contrast-enhanced CT may provide additional benefit
Better characterization of focal areas of FDG activity
Differentiation of potential bowel lesion from those adjacent to bowel
CT Findings
CT typically used to help identify primary
Low sensitivity (˜ 25%)
CT scanning is the imaging modality of choice in terms of availability, cost effectiveness, quickness, and patient compliance
Especially for evaluation of cervical lymphadenopathy and identification of occult primary lesions
Newer technology and methods of acquisition
Better image quality and resolution
Better reconstructive capabilities
Quicker scans
Decreased artifact
Quicker scans also allow dynamic maneuvers to be used
Puffed cheek and modified Valsalva techniques can help open opposed mucosal surfaces in the oral cavity, oropharynx, and hypopharynx
May allow easier detection of unknown mucosal primaries
Nonetheless, critical evaluation of the CT scan helps direct biopsies during panendoscopy in the workup of the unknown primary tumor
For evaluation of cervical lymphadenopathy, a CT scan of the neck is helpful to assess the involvement of vital structures
Also provides the clinician with useful data regarding surgical resectability
CT scan can also be used to evaluate clinically negative cervical lymph node zones
Radiographic criteria of potential pathological lymph nodes
Rounding of the lymph node
Size > 1.5 cm in the jugulodigastric region or > 1 cm in other regions
Hypodense fluid center of the lymph node that signifies necrosis
Mass effect
Nuclear Medicine Findings
PET
FDG PET shown to identify lesion in ˜ 25-40% of patients with negative conventional imaging investigations
PET may commonly reveal “missed primary”
Rather than unknown primary in true sense, i.e., following complete workup
False negative may result from
Low tumor uptake (e.g., carcinoid) or high background uptake (e.g., liver, high serum glucose level)
PET has high specificity for tumors in lung, breast, and pancreas
Possibly low clinical impact of FDG PET in patients who have already undergone extensive workup with panendoscopy
Small study showed PET/CT more sensitive than PET alone, with 53% detection rate for occult cancers missed by other techniques
Criteria for malignancy on FDG PET or PET/CT
FDG hypermetabolism at site of pathological changes on CT
Marked focal hypermetabolism at sites suggestive of malignancy (liver parenchyma, bone marrow)
Despite absence of signs of pathology at those sites on CT
Identification of primary is more complex than identification of metastatic lesions
Patient’s history is often helpful
Distribution of pathological lesion may be helpful
Knowledge of the pattern of spread of different tumors
More difficult in cases of generalized disease with many foci in different organs
If unable to identify a lesion as the site of primary, may conclude that CUP syndrome was generalized
Rate of detection of malignancy in general will be higher than that of primary
DIFFERENTIAL DIAGNOSIS
Physiologic Activity
Following structures commonly have increased physiologic activity that may mimic that of malignancy
Colon: Can be focal, short segment, or linear
Cardiac: Usually left ventricular, though all chambers may have increased wall activity in pathologic states
Thymus: Seen in younger patients, usually linear if physiologic
Glands: Look for symmetry to differentiate physiologic from pathologic activity
Lymphoid tissue: May be asymmetrical or symmetrical
Muscle: Often linear, helping to establish as physiologic; when focal can look like malignancy; correlate with CT
Brown fat: CT showing fat attenuation is diagnostic
PET/CT helps facilitate differentiation of pathologic from physiologic FDG activity
Inflammation
Several inflammatory or granulomatous conditions, such as sarcoidosis, may cause focal FDG activity and mimic malignancy
Infection
Infectious processes such as underlying fungal infection or TB may cause focal activity
Dental abscesses may cause focal intense FDG activity, mimicking head and neck cancer
Benign Lesion
Colonic adenomas and thyroid adenomas may have focal FDG activity
Benign osseous lesions include fibrous cortical defect, osteoradionecrosis, and Paget
Iatrogenic
Post-operative changes or catheters and ostomies may appear as focal areas of FDG activity, mimicking malignancy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree