Cardiac neoplasms are a diagnostic challenge on many levels. They are rare, their clinical presentation may mimic other much more common cardiac diseases, and they are at an uncommon intersection of oncologic and cardiac imaging. The pathology of primary cardiac neoplasms explains their varied imaging features, for example, calcification in primary cardiac osteosarcomas and T2 hyperintensity in myxomas. Integrating the imaging and pathologic features of cardiac tumors furthers our understanding of the spectrum of appearances of these neoplasms and improves the clinical imager’s ability to confidently make a diagnosis.
Key points
- •
Primary cardiac neoplasms are rare, and their clinical presentation may mimic more common nonneoplastic cardiac diseases.
- •
The varied imaging appearances of primary cardiac neoplasms can be explained by their underlying pathology.
- •
Primary considerations for the imaging diagnosis of primary cardiac neoplasms are location, tissue characterization, and clinical features such as age and associated syndromes.
Introduction
Cardiac neoplasms are a diagnostic challenge on many levels. They are rare, their clinical presentation may mimic other much more common cardiac diseases, and they are at an uncommon intersection of oncologic and cardiac imaging. Despite these obstacles, it is often possible to arrive at a favored diagnosis using advanced imaging techniques and knowledge of the pathologic basis of cardiac neoplasms. As with imaging tumors elsewhere in the thorax, a foundation in the pathology of cardiac neoplasms explains an entire spectrum of imaging appearances. Furthermore, knowledge of cardiac tumors ranging from imaging appearances to epidemiology informs the diagnostic approach to these lesions and ultimately their management. This work will explore the imaging approach to cardiac neoplasms with emphasis on the most common, clinically significant tumors and the relationship between their pathology and imaging manifestations.
An epidemiologic context is the first step to arriving at a clinically relevant diagnosis or a short differential diagnosis. Primary cardiac neoplasms are rare in both autopsy series and clinical practice, with metastatic disease being 40 to 100 times more common. This difference between the incidence of primary tumors and metastatic disease may be inconsistent with the clinical experience of cardiac imagers who frequently evaluate cardiac neoplasms. However, it should be noted that most epidemiologic data are derived from autopsy series or large clinical databases in which cardiac spread may be detected in the larger context of metastatic disease but not undergo further diagnostic evaluation.
Primary cardiac neoplasms occur at an incidence of 30 per 100,000 people per year. , Approximately 80% of primary cardiac tumors are benign. The World Health Organization has classified neoplasms of the heart into either benign tumors and tumorlike lesions such as myxoma, malignant lesions such as angiosarcoma, and pericardial tumors such as solitary fibrous tumors. In patients older than 16 years, the most common primary cardiac neoplasms are myxomas, lipomatous tumors, and papillary fibroelastomas. In patients younger than 16 years, the most common tumors are rhabdomyomas, teratomas, fibromas, and myxomas.
The most common presenting symptom of a cardiac tumor is dyspnea, but the manifestations of a neoplasm will depend on the location of the lesion and size. Even benign cardiac tumors may cause obstruction of blood flow, decreased cardiac output, arrhythmia, or heart failure, which can be fatal. , In addition, systemic manifestations such as fatigue, anorexia, and fever may also be seen.
Myxoma
Clinical Considerations
Cardiac myxoma is the most common benign primary cardiac neoplasm, accounting for up to 80% of all cases, but only represent 10% of benign primary cardiac tumors in children. Approximately 3% to 10% of cardiac myxomas are associated with Carney complex, an autosomal dominant disorder characterized by pigmented lesions of the skin and mucosae, cardiac myxomas, cutaneous tumors, and multiple other endocrine and nonendocrine neoplasms. In this disorder, pituitary neoplasms lead to acromegaly and adrenocortical tumors lead to Cushing syndrome. In this disorder, cardiac myxomas are responsible for 50% of the related mortality and are often found in multiple locations, in younger patients, and have a higher risk of recurrence. ,
Symptoms are variable and include shortness of breath and chest pain as well as constitutional symptoms such as fever and weight loss. , Embolism may be a presenting sign of a myxoma in up to 30% of patients. Myxomas within the left heart have been shown to present earlier with worse shortness of breath when compared with right heart tumors.
Although they can be located in any chamber, most myxomas are located within the left atrium and originate at the interatrial septum. These lesions may have an irregular border, a pedunculated morphology, and be mobile. , The size of the tumor is related to the degree of mobility and the potential that the lesion can obstruct the atrioventricular valve.
Pathologic Features
At gross inspection, most myxomas are soft, gelatinous, or friable lesions, ranging from 2 to 11 cm in size. The contour of the tumor is most often lobular and smooth but can be villiform in appearance, which is thought to be associated to thromboembolism. ,
Histologically, myxomas demonstrate myxoma cells in a myxoid stroma with possible calcification and hemorrhage. These lesions may demonstrate heterotopic elements such as bone, glands, and giant cells. In addition, the use of the immunohistochemical test of PRKAR1A, a cAMP-dependent protein kinase type 1α regulatory subunit, can be used as a screening tool to evaluate for Carney complex in the setting of myxomas.
Imaging Features
Transthoracic echocardiography is the initial imaging modality of choice for the evaluation of cardiac myxomas, although findings are nonspecific. On echocardiography, a myxoma may be heterogenous or homogeneous and may have calcification. Although computed tomography (CT) is not the preferred method to characterize the tumor, typical findings on a contrast-enhanced CT include a spherical or ovoid mass that is lower in attenuation than surrounding myocardium. Characteristic features of a myxoma on MR imaging is T2-weighted hyperintensity, hypoperfusion on first-pass perfusion following the administration of intravenous gadolinium, and a heterogeneous appearance on delayed enhancement when compared with the myocardium ( Figs. 1 and 2 ). , Gradient echo imaging may demonstrate susceptibility artifact due to hemosiderin. Parametric techniques can also be applied to characterize the mass with T1 mapping demonstrating T1 times between 1285 and 1356 msec and T2 mapping demonstrating T2 times between 76 and 270 msec at 1.5 T.


Management
Surgical resection is the treatment of choice and is associated with excellent outcomes. In one series of 95 patients, there was only a single recurrence over 5 years following excision. Patients are regularly followed with transthoracic echocardiography 1 year following excision and then at 5 years.
Rhabdomyoma
Clinical Considerations
Rhabdomyoma is the most common primary cardiac tumor of infancy and childhood representing 60% of pediatric primary cardiac neoplasms. These lesions are most often diagnosed during the first year of life or prenatally. Cardiac rhabdomyomas are associated with tuberous sclerosis in 30% to 50% of cases but also occur sporadically and rarely in association with congenital heart disease. , Tuberous sclerosis is characterized by cortical tubers and subependymal nodules within the brain, multiple retinal hamartomas, adenoma sebaceum of the skin, and periungual fibromas. Rhabdomyomas may precede other sequelae of tuberous sclerosis such as skin abnormalities and neuroimaging findings by months or years. Symptoms of cardiac rhabdomyomas vary and are based on the size and location of the tumor. They may be asymptomatic or result in congestive heart failure from obstruction. Arrhythmias have also been reported.
Rhabdomyomas are most commonly located within the ventricles attached to the myocardium but are less commonly located in the atrioventricular groove. , They are multiple in 60% of cases, typically in the setting of tuberous sclerosis.
Pathologic Features
At gross inspection, rhabdomyomas are lobulated masses with a glistening cut surface. Sporadic tumors tend to be larger in size than those associated with tuberous sclerosis. At histology, these neoplasms tend to have large cells in relation to the myocardium with abundant glycogen. “Spider cells” are present in all tumors that have a centrally located mass of granular cytoplasm with elongated projection of myofibrils extending peripherally from the nucleus to the cell membrane. , These lesions demonstrate positive immunohistochemical staining for desmin, actin, and myoglobin.
Imaging Features
On transthoracic echocardiography, rhabdomyomas are uniformly hyperechoic in appearance ( Fig. 3 ). On contrast-enhanced CT, they are most often hypodense masses with little contrast enhancement. On MR imaging, these tumors are homogenous in appearance, isointense to slightly hyperintense to myocardium on T1-weighted imaging, mildly hyperintense in relation to the myocardium on T2-weighted imaging, hypoenhancing on first pass perfusion, and isointense to myocardium on myocardial delayed enhancement. ,

Management
Most rhabdomyomas spontaneously regress. When there is outflow obstruction leading to heart failure or arrhythmias, surgical resection may be performed. In addition, everolimus, a mammalian target of rapamycin inhibitor, may be used as therapy.
Fibroma
Clinical Considerations
Cardiac fibroma is the second most common primary cardiac neoplasm of infancy and childhood after rhabdomyoma. Although cases do occur in adults, greater than 80% of cardiac fibromas are in children. These tumors occur more frequently in nevoid basal cell carcinoma (Gorlin) syndrome, a phakomatosis characterized by multiple basal cell carcinomas; odontogenic cysts; ocular pathology such as congenital cataracts, microphthalmia, and coloboma of the iris; and other tumors such as medulloblastoma. Two percentage of patients younger than 45 years with basal cell carcinomas have this syndrome.
Patients with cardiac fibromas may be asymptomatic but may also present with arrhythmias, congestive heart failure, and sudden death believed to be secondary to distortion of the conducting system of the heart rather than infiltration. The most common locations of a cardiac fibroma are the left ventricular free wall, interventricular septum, and right ventricular free wall.
Pathologic Features
At gross inspection, cardiac fibromas tend to be solitary well-demarcated white tumors ranging from 3 to 8 cm in diameter. Cut surfaces are either white, gray, or tan ( Fig. 4 ). At histology, the tumor contains prominent spindle-shaped fibroblasts with a collagen matrix. The collagen matrix increases with age and the amount of cellularity decreases with age. Cells express alpha smooth muscle actin and do not express desmin, CD 34, or S100 protein. Calcification is seen but this is more likely in older patients.

Imaging Features
Chest radiographs may show calcification in cardiac fibromas. Transthoracic echocardiography is successful in identification of the mass and demonstrates mixed echogenicity. On contrast-enhanced CT, fibromas tend to enhance either homogenously or heterogeneously. On MR imaging, the lesion may have a thin rim of myocardium with a heterogeneous signal intensity on both T1- and T2-weighted images. Following the administration of intravenous gadolinium, the mass demonstrates avid hyperenhancement on delayed imaging with or without decreased enhancement centrally.
Management
Surgical resection is the treatment of choice for cardiac fibromas with excellent early and late-term outcomes. If a tumor is difficult to resect due to location, subtotal resection has also been shown to result in excellent long-term survival.
Hemangioma
Clinical Considerations
Hemangiomas account for 5% to 10% of all benign cardiac neoplasms and can occur in any age group. Although patients are often asymptomatic, the most common symptom is dyspnea on exertion. Rarely patients may develop Kasabach-Merritt syndrome manifesting as recurrent thrombocytopenia and consumptive coagulopathy. These tumors can occur in any chamber of the heart but are most common in the ventricles.
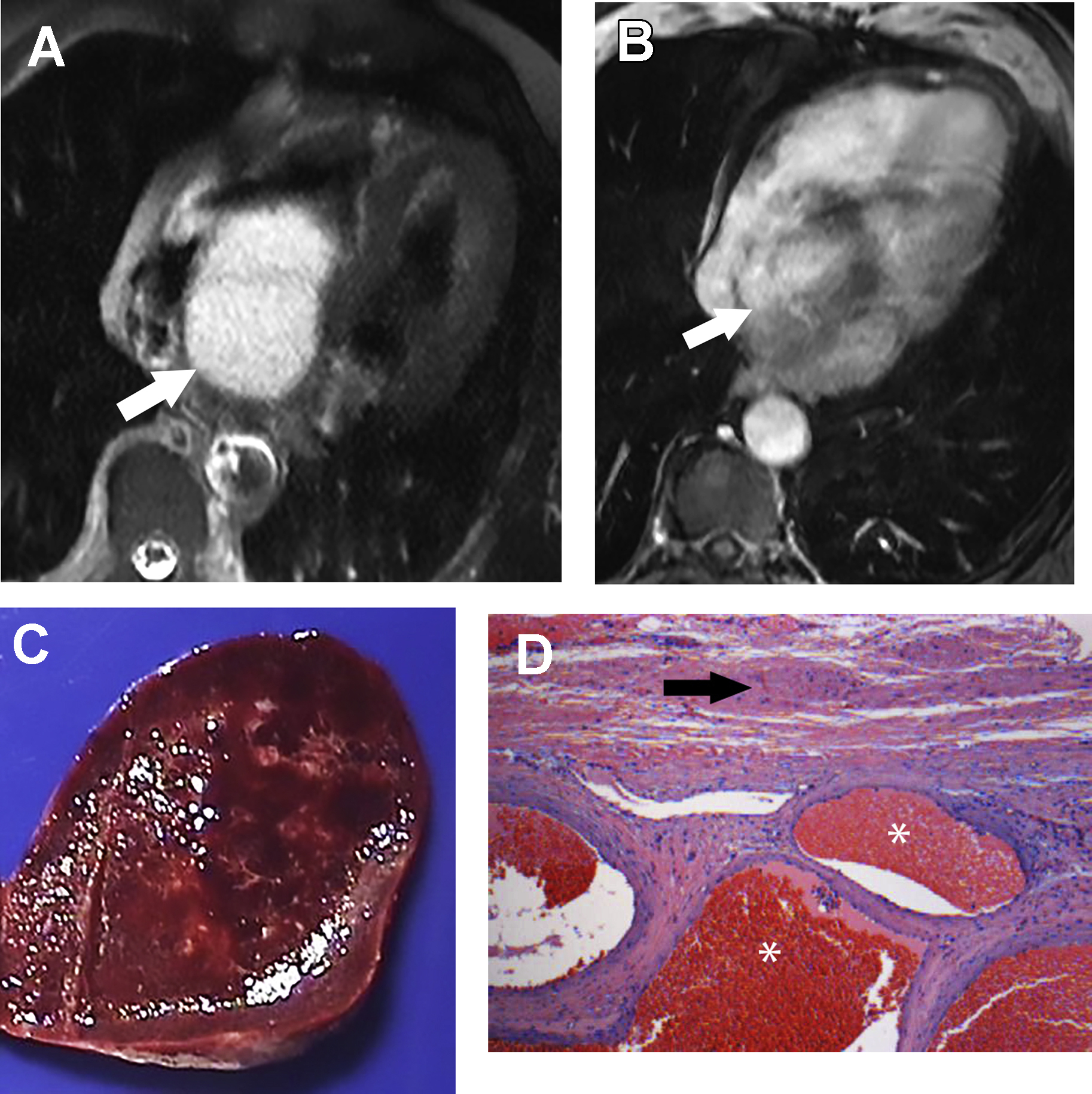
Pathologic Features
At gross inspection, hemangiomas are red and hemorrhagic. On histology, there are 3 variants capillary, cavernous, and arteriovenous. The lesions are composed of a dilated mixture of mature vessels supported by fibrous connective tissue.
Imaging Features
Transthoracic echocardiography of a hemangioma reveals a solid vascular mass. On contrast-enhanced CT, hemangiomas are heterogeneous masses that may contain calcifications and avidly enhance. On MR imaging, hemangiomas are heterogeneous and hyperintense to myocardium on T2-weighted imaging and isointense to hypointense to myocardium on T1-weighted imaging ( Fig. 5 ). They enhance on first pass perfusion but may have variable enhancement on myocardial delayed imaging. Differentiation of hemangiomas from other vascular tumors, even malignant neoplasms such as angiosarcoma, can be difficult on MR imaging.