Clinical Correlation
The most common disease affecting the carotid arteries is atherosclerosis. Other less common, but clinically important conditions include dissection, trauma, and carotid body tumors.
The carotid bifurcation is a common location for the development of atherosclerotic plaque. Although usually asymptomatic, atherosclerosis of the carotid bifurcation may become unstable and cause monocular blindness, transient cerebral ischemia, or stroke.
Monocular blindness may be temporary (also known as amaurosis fugax ) or permanent. It is due to embolization of atheromatous debris to the retinal artery. Symptoms are ipsilateral to the arterial source of the emboli. Typically, the patient reports complete blindness in part or all of the visual field of one eye. The blindness is often described as a shade coming across part of the visual field of the eye and may involve a quadrant, half, or all of the visual field. Temporary blindness typically resolves over seconds to a few minutes, with complete resolution. A cholesterol crystal (Hollenhorst’s plaque) may be seen on funduscopic examination.
In terms of the carotid arteries, a stroke is defined as a focal, cerebral hemispheric deficit persisting for longer than 24 hours. A transient ischemic attack (TIA) is a focal, cerebral hemispheric deficit persisting less than 24 hours, typically resolving in minutes to a few hours. Symptoms include unilateral motor weakness, unilateral sensory changes (numbness or paresthesia), dysarthria (slurred speech), or language deficit (most typically an expressive dysphasia or aphasia). Motor and sensory deficits occur on the side of the body contralateral to the etiologic carotid artery. Language deficits are due to ischemia of the dominant hemisphere. Dysarthrias may be due to ischemia of either cerebral hemisphere.
Dissection of the carotid artery may occur spontaneously or may be due to trauma, iatrogenic injury, or as a component of aortic dissection. Clinical presentation may include unilateral neck or head pain, Horner’s syndrome (decreased diameter of the pupil, drooping of the eyelid, decreased sweating on the side of the face), and/or ipsilateral TIA or stroke.
Penetrating, blunt, or iatrogenic trauma to the neck may cause carotid disruption with hemorrhage and hematoma, carotid occlusion, or carotid dissection. These injuries may present with bleeding, neck fullness, pain, TIA or stroke, or may be asymptomatic.
Carotid body tumors (paragangliomas, glomus tumors, chemodectomas) characteristically present as a painless mass or fullness in the neck. Larger tumors may cause compressive symptoms such as pain, difficulty or pain with swallowing, hoarseness, or stridor.
Normal Anatomy
The right common carotid arises from the brachiocephalic artery. The left common carotid artery arises as the second branch of the aortic arch. The common carotid arteries bifurcate in the midneck into the internal and external carotid arteries. The internal carotid artery has no branches in the neck. Its terminal branches in the cranial cavity include the ophthalmic, anterior cerebral, middle cerebral, and posterior communicating arteries. The branches of the external carotid artery are the superior thyroid, lingual, facial, occipital, posterior auricular, ascending pharyngeal, superior temporal, and maxillary arteries.
The internal jugular vein lies superficial and posterolateral to the carotid arteries. The vagus nerve is typically deep to and between the carotid arteries and the jugular vein. The hypoglossal nerve crosses the internal and external carotid arteries from posterolateral to anteromedial. The carotid body lies in the crotch of the internal and external carotid arteries.
Imaging
Carotid artery evaluation requires high-resolution B-mode imaging and pulsed Doppler with spectral analysis. A linear array scan head with transducer frequencies of 5 to 12 MHz is most commonly used. The patient is positioned supine, with the head turned away from the examiner and the neck extended. The examiner is seated at the head of the bed.
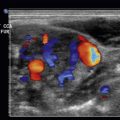
The carotid arteries are evaluated in transverse and longitudinal axes with B-mode imaging. Pulse Doppler is performed in the longitudinal axis. Doppler angles should be 60 degrees or less. The sample volume should be moved throughout the long axis of the arteries, particularly at the common carotid bifurcation and in the proximal internal carotid artery, to identify regions of maximal stenosis. Color Doppler may be useful to localize areas for more specific assessment with pulse Doppler.
The internal carotid artery typically has low resistance to flow, with the spectral waveform showing a brisk upstroke and antegrade flow throughout diastole ( Fig. 6.1 ). The external carotid artery has a smaller diameter than the internal carotid artery at the carotid bulb but a similar diameter more distally ( Fig. 6.2 ). The external carotid artery has flow characteristics similar to most peripheral arteries, with a triphasic spectral waveform: brisk forward upstroke, retrograde flow in early diastole, and antegrade flow in late diastole ( Fig. 6.3 ). The waveform in the external carotid artery may show lower resistance if the external carotid artery has developed collateral flow to the intracranial circulation, making it more difficult to tell whether the artery is the internal or external carotid. In this case, a temporal tap may be used to confirm that the external carotid artery is being evaluated ( Fig. 6.4 ). While monitoring the waveform in the artery, the ipsilateral superficial temporal artery (anterior to the ear) is rapidly compressed with the examiner’s finger; oscillations will be visible on the spectral waveform if the artery being evaluated is the external carotid. The common carotid artery supplies flow to both the internal and external carotid arteries; therefore its waveform will be a hybrid between a low-resistance and high-resistance pattern ( Fig. 6.5 ). However, as the internal carotid artery carries much more volume than the external carotid artery, the common carotid artery typically has a relatively low-resistance pattern.





Pathology
Carotid Stenosis
The diagnosis of carotid stenosis is primary based on spectral analysis for measuring flow velocities. Although B-mode imaging will identify plaque, ultrasound imaging alone is not accurate for measuring carotid stenosis.
A stenosis in the internal carotid artery will lead to turbulent flow patterns. At a moderate degree of stenosis, the peak systolic velocity will be elevated ( Fig. 6.6 ). A more severe stenosis will elevate the end diastolic velocity ( Fig. 6.7 ). The ratio between the peak systolic velocity in the internal carotid artery and the peak systolic velocity in the common carotid artery is also useful. Various criteria have been proposed to define the degree of stenosis in the internal carotid artery; the two most commonly used criteria are presented in Tables 6.1 and 6.2 . When the internal carotid artery is occluded, the waveforms in the common carotid artery will assume a pattern similar to that in the external carotid artery ( Fig. 6.8 ). There are no validated criteria to define the degree of stenosis in the common or external carotid arteries. However, a stenosis in these arteries may be inferred by a focal increase in the peak systolic velocity and turbulent flow.