CHAPTER 89 Carotid Artery Disease
The ancient Greeks believed that compression of the carotid artery caused sudden sleep (karoo, “to stupefy”). Ambroise Paré later named these arteries “the right and left carotides or sleepy vessels” in the 16th century.1 In 1914, J. Ramsay Hunt noted that partial or complete occlusion of the carotid artery could be responsible for “cerebral intermittent claudication.”1 In 1935, Aring clarified the differences between brain hemorrhages and infarctions in autopsy cases. The notion that carotid artery occlusive disease can produce a dementia state was proposed soon thereafter.1 It was postulated that restoration of blood supply could reverse the condition. This inspired the first carotid reconstruction (1951) by Carrea, Molins, and Murphy in Argentina.1 They performed an anastomosis of the distal internal carotid artery to the external carotid artery after partial resection of a stenosed internal carotid artery. Although DeBakey is credited with performing the first carotid endarterectomy (CEA), the report in 1954 by Eastcott, Pickering, and Rob of a successful carotid reconstruction in a woman after acute stroke provided a major impetus for operative intervention in carotid occlusive disease and introduced CEA as an important procedure in the management of stroke.1 In the ensuing decades, atherosclerotic carotid occlusive disease has been recognized as, by far, the most common disorder affecting the extracranial carotid artery and has become one of the most intensively studied of vascular diseases. Treatment decisions are appropriately guided by several randomized trials and additional well-designed large cohort studies.
CAROTID ARTERY STENOSIS
Prevalence and Epidemiology
Stroke is the third leading cause of death in the United States. Each year, 600,000 patients suffer a new stroke, and 170,000 deaths per year are attributable to cerebrovascular disease.2 Stroke is also the leading cause of disability among elderly Americans. Although there has been a 50% reduction in mortality during the last two decades, 21% of survivors will still have a second stroke and 7% a third stroke. Forty percent will require special nursing home care; 10% will require institutionalization involving an expenditure of billions of dollars of the health care budget.2
About one third of strokes are thromboembolic in etiology, and atherosclerotic carotid occlusive disease is the most common single cause. The extent to which carotid stenosis or occlusion can be attributed to stroke has been difficult to determine from population studies. Between 1993 and 1997, the Northern Manhattan Study identified cerebral infarction attributable to carotid stenosis in 17 (95% CI, 8 to 26) per 100,000 blacks, 9 (5 to 13) per 100,000 Hispanics, and 5 per 100,000 (2 to 8) whites.3 Approximately 7% of all first ischemic strokes occurred in the presence of extracranial carotid artery stenosis of 60% or more. Between 1985 and 1989, in the Mayo Clinic study conducted among the population of Rochester, Minnesota, 18% of all first ischemic strokes occurred in the presence of significant extracranial or intracranial carotid artery stenosis.4
A variety of risk factors contribute to an increased risk of stroke. The Framingham study5 confirmed that there was no difference in incidence related to gender. However, increasing age, systolic and diastolic blood pressure, diabetes, smoking, and cardiovascular diseases were associated with an increased risk for stroke. The age-adjusted relative risk for stroke among hypertensive patients (>160/95 mm Hg) in contrast to normotensive persons (<140/90 mm Hg) is 3.0 in men and 2.9 in women. Smokers may have a 50% increase in risk of atheroembolic stroke compared with nonsmokers.
Etiology and Pathophysiology
The unique hemodynamics at the carotid bifurcation predisposes this area to atherosclerosis. Along the inner wall of the carotid bulb, blood flow remains laminar, with high velocity and high shear stress. Conversely, along the outer wall, there are areas of flow separation, stasis, turbulent flow, and a complex oscillating shear stress pattern that predisposes to atherosclerotic plaque deposition.6 Although neurologic events have been attributed to progressive stenosis and decreased blood flow from enlarging atherosclerotic plaques, most such events are usually secondary to plaque disruption and atheroembolization from the lesion. Loss of the fibrous cap with exposure of atherosclerotic debris to the flow lumen appears to be responsible for these embolic complications. Additional factors, such as adequacy of collateralization, plaque ulceration or hemorrhage, hypotension, and low cardiac output, also play a contributory role.
Histologic evaluation of atherosclerotic plaques has demonstrated that they originate from fatty streaks that, over time, accumulate into a lipid core.7 The fatty streak becomes a fibroatheroma as fibrous tissue accumulates over the core and forms a fibrous cap (Fig. 89-1). Through unknown mechanisms, some plaques become unstable, resulting in an enlarging lipid core, intraplaque hemorrhage, plaque enlargement, fibrous cap rupture, ulceration, and luminal thrombosis. These histomorphologic features have been associated with the production of atheroemboli and neurologic symptoms. Specifically, large lipid cores located close to the flow lumen, intraplaque hemorrhage, and fibrous cap disruption with ulceration have frequently been observed in CEA specimens obtained from patients with symptomatic plaques (Fig. 89-2A).8 Conversely, small lipid cores located deep within the plaque with a thick fibrous cap have been observed in CEA specimens from patients with asymptomatic carotid stenosis (see Fig. 89-2B).8
Manifestations of Disease
Clinical Presentation
Because one of the major goals in the management of carotid stenosis is to prevent stroke, the identification of individuals with asymptomatic stenosis becomes an important objective. The incidence of asymptomatic carotid stenosis in the general population is difficult to estimate. In one study of 2000 asymptomatic patients screened by duplex ultrasonography, significant carotid stenosis was found in 32.8% of patients with peripheral vascular disease, 6.8% of patients with coronary artery disease, and 5.9% of patients with significant risk factors.9 Perhaps the most frequent reason for suspecting a carotid stenosis is a cervical bruit in a high-risk patient. However, bruit is nonspecific and is associated with significant stenosis in only 47% of patients. Conversely, only 60% of significant carotid stenoses will be manifested as a bruit.10 Although auscultation of a bruit is not a sensitive or specific predictor of carotid stenosis, it remains an important clinical sign in an otherwise asymptomatic patient and must prompt a duplex ultrasound evaluation. Of additional interest is the association of cervical bruit with coronary artery disease. Its presence should also prompt a clinical evaluation for coronary artery disease because the bruit may actually be a more accurate predictor of myocardial infarction than stroke.10
Alternatively, patients may first present with a variety of symptoms related to atheroembolic ischemic events. Eye symptoms can result from embolization to the retinal, ophthalmic, or cerebral circulation and include one or more of the following: amaurosis fugax (blurring or loss of vision in the ipsilateral eye, typically described as a curtain or shade falling over the eye), homonymous hemianopia (resulting from emboli to optic radiation), intermittent retinal blindness (loss of vision on exposure to bright light), neovascularization of iris (resulting from ophthalmic artery ischemia), and, rarely, complete blindness (resulting from ischemic optic neuropathy). More commonly, atheroemboli travel to the intracranial circulation and result in lateralizing deficits that may follow several patterns. A transient ischemic attack tends to be a stereotypic and temporary loss of sensory, motor, or visual function that usually lasts for less than 15 minutes. Per definition, patients always return to baseline within 24 hours. Alternatively, patients may have recurring attacks of deficits similar to a transient ischemic attack without an interval allowing complete recovery. The deficit is often the same with each attack, and there is no deterioration in function. These symptoms are associated with a worse outcome and are referred to as crescendo transient ischemic attacks. Patients may also present with recurring attacks of focal neurologic deficits with progressive deterioration in neurologic function. This is termed a stroke in evolution and generally lasts longer than 24 hours. Finally, a completed stroke occurs when a deficit has stabilized beyond 24 hours. The definitions of transient ischemic attack and stroke are evolving. Studies of patients with diffusion-weighted MRI demonstrate that many patients with transient ischemic attacks lasting only hours will actually be shown to have sustained cerebral infarction.11
All patients with suspected or confirmed carotid stenosis must undergo a complete neurologic examination to identify potential neurologic deficits and to establish a clinical baseline with which to compare outcomes of future therapeutics. No single outcome measure can describe or predict all dimensions of recovery and disability after acute stroke. Several scales have proved reliability and validity in stroke trials, including the National Institutes of Health Stroke Scale (NIHSS), the modified Rankin Scale, the Barthel Index, the Glasgow Outcome Scale, and the Stroke Impact Scale. The NIHSS comprises 15 items that enable standardized application and measurement of a simple neurologic examination.12 The scale assesses the level of consciousness, extraocular movements, visual fields, facial muscle function, extremity strength, sensory function, coordination, language, speech, and hemi-inattention. It has undergone extensive validation and is the preferred method of quantification of neurologic deficits in a clinical trial setting.13–16
Imaging Indications and Algorithm
A clinically detected carotid bruit, or neurologic symptoms attributable to the carotid artery territory as outlined before, should prompt a noninvasive assessment of the carotid arteries. The most commonly performed study is an ultrasonographic evaluation. Alternative approaches include evaluation with a CT scan or MRI, which have the advantage of being able to incorporate intracranial views to assess for infarctions. However, these studies are more expensive, and the yield for intracranial disease is low. Noninvasive studies typically yield information about the lesion that is reliable enough to plan further management.17 In cases in which the stenosis is determined to be borderline significant, a second noninvasive study provides complementary information. Exceptional circumstances, such as the inability to differentiate between an occluded and a very tight stenosis, warrant an invasive study such as angiography.
Imaging Techniques and Findings
Angiography
The degree of carotid stenosis generally correlates with risk of stroke in symptomatic extracranial carotid occlusive disease. Cerebral angiography (Fig. 89-3) was the first definitive investigative tool used to visualize and to quantify carotid stenosis. Multiplanar angiography still remains the gold standard for preoperative delineation of extracranial carotid occlusive disease. Complete details of diagnostic procedures have been included in other chapters in this book. The definition of a significant carotid stenosis has been conventionally accepted as a 50% decrease in the luminal diameter, which translates into a 75% reduction in cross-sectional area. On cerebral angiography, the maximal stenosis is determined on the anteroposterior, lateral, or oblique view. Two methods to estimate the percentage of diameter reduction are in common use (Fig. 89-4). The first (North American) method compares the least transverse diameter at the stenosis with the luminal diameter of the distal internal carotid artery once its walls become parallel. This technique has been used by the majority of carotid atherosclerosis trials.13–15 The second method compares it with the presumed normal luminal diameter at the stenosis and has been used in Europe.18 The percentage stenosis measured by the North American method will be lower than the European measurement; for example, North American measurements of 30%, 40%, 50%, 60%, 70%, 80%, and 90% stenosis will correspond to 65%, 70%, 75%, 80%, 85%, 91%, and 97% stenosis, respectively, in Europe. It is therefore important to specify the method used for estimation of percentage stenosis for purposes of comparison with published data.

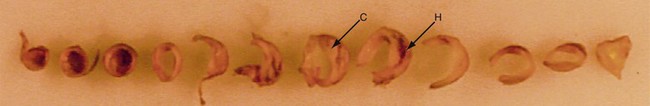
 FIGURE 89-1
FIGURE 89-1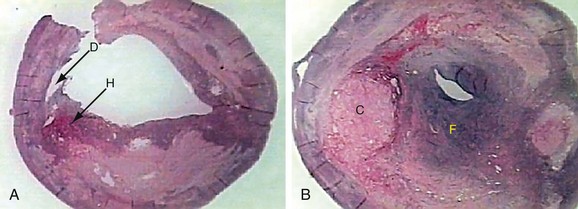
 FIGURE 89-2
FIGURE 89-2
 FIGURE 89-3
FIGURE 89-3

