Carpal Tunnel Syndrome
KEY FACTS
Terminology
Imaging
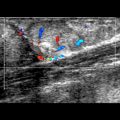
 Intraneural hyperemia
Intraneural hyperemia
 Retinacular bowing
Retinacular bowing
 Flattening ratio: Width:depth ratio > 3 of median nerve ↑ with CTS
Flattening ratio: Width:depth ratio > 3 of median nerve ↑ with CTS
 Homogeneously hypoechoic with loss of normal fascicular pattern
Homogeneously hypoechoic with loss of normal fascicular pattern
 If either CSA proximal to or distal to carpal tunnel is > 14 mm² or palmar volar bowing of flexor retinaculum at outlet > 1 mm, sensitivity, specificity & accuracy are 100%, 84%, and 93%, respectively
If either CSA proximal to or distal to carpal tunnel is > 14 mm² or palmar volar bowing of flexor retinaculum at outlet > 1 mm, sensitivity, specificity & accuracy are 100%, 84%, and 93%, respectively
IMAGING
General Features
Ultrasonographic Findings
 Swelling of median nerve either immediately proximal to, within, or immediately distal to carpal tunnel
Swelling of median nerve either immediately proximal to, within, or immediately distal to carpal tunnel
 Measure CSA by tracing around nerve perimeter
Measure CSA by tracing around nerve perimeter
 2 main measurement methods based on median nerve CSA, either of which can be used
2 main measurement methods based on median nerve CSA, either of which can be used
 Median nerve CSA measured at 4 points: Immediately proximal to tunnel inlet, at tunnel inlet, at tunnel outlet, & distal to carpal tunnel
Median nerve CSA measured at 4 points: Immediately proximal to tunnel inlet, at tunnel inlet, at tunnel outlet, & distal to carpal tunnel
 Optimal cutoff point: Median nerve CSA ≥ 14 mm²
Optimal cutoff point: Median nerve CSA ≥ 14 mm²
 Median nerve CSA ≥ 14 mm² at proximal or distal to carpal tunnel: Strong positive predictor of CTS (sensitivity/specificity/accuracy > 88%)
Median nerve CSA ≥ 14 mm² at proximal or distal to carpal tunnel: Strong positive predictor of CTS (sensitivity/specificity/accuracy > 88%)
 Median nerve CSA measured at proximal 1/3 of pronator quadratus muscle level (CSAf) & immediately proximal to tunnel inlet, at tunnel inlet, & at tunnel outlet (CSAc)
Median nerve CSA measured at proximal 1/3 of pronator quadratus muscle level (CSAf) & immediately proximal to tunnel inlet, at tunnel inlet, & at tunnel outlet (CSAc)
 Difference between pronator quadratus level measurement (CSAf) & any carpal tunnel measurement (CSAc) should not be > 4 mm²
Difference between pronator quadratus level measurement (CSAf) & any carpal tunnel measurement (CSAc) should not be > 4 mm²
 Difference between CSAc & CSAf (ΔCSA) of > 4 mm² is strong positive predictor of CTS
Difference between CSAc & CSAf (ΔCSA) of > 4 mm² is strong positive predictor of CTS





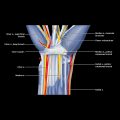
 deep to the flexor retinaculum
deep to the flexor retinaculum  & superficial to the flexor tendons. The nerve usually divides just beyond the tunnel outlet.
& superficial to the flexor tendons. The nerve usually divides just beyond the tunnel outlet.
 lies immediately below the flexor retinaculum
lies immediately below the flexor retinaculum  & superficial to the flexor digitorum tendons, which are surrounded by the ulnar bursa
& superficial to the flexor digitorum tendons, which are surrounded by the ulnar bursa  & the flexor pollicis longus, which is surrounded by the radial bursa
& the flexor pollicis longus, which is surrounded by the radial bursa  . The extrinsic ligaments
. The extrinsic ligaments  lie above the carpal bones.
lie above the carpal bones.
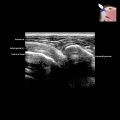
 . A nerve cross-sectional area (CSA) > 14 mm² is a positive predictor for CTS. Note also the loss of neural fascicular structure, which is an additional sign of CTS.
. A nerve cross-sectional area (CSA) > 14 mm² is a positive predictor for CTS. Note also the loss of neural fascicular structure, which is an additional sign of CTS.