Outline
Topic 5, Figure 159
- 1.
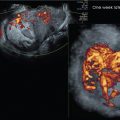
Fig. 159 . Topic: Normal Endoanal 3D Image of the Distal Internal (IAS) and External Anal Sphincter (EAS)

Fig. 159
At this axial level, the hyperechoic EAS envelops the hypoechoic IAS. Because of the biplane endoanal transducer placement in the rectum, the central mucosa is circumferentially displaced peripherally. Both the IAS and the EAS are intact.
Case 75, Figure 160
- 2.
Fig. 160 demonstrates transperineal 3D imaging of the pelvic floor using a 5–9 MHz endovaginal (EV) transducer. The curvilinear transducer can be seen directly above the urethral and vaginal orifices at screen top (gold arrows). Which of the following structures are indicated by the gold numbers?
- a.
Anterior vaginal wall
- b.
Posterior vaginal wall
- c.
Proximal urethra
- d.
Mid-urethra
- e.
Distal urethra
- f.
Pubovisceralis muscle complex
- g.
Internal anal sphincter
- h.
External anal sphincter
- i.
Anal sphincter central mucosa

Fig. 160
- a.
Case 76, Figures 161 and 162
- 3.
Fig. 161 is a transperineal 3D volume set of the pelvic floor using a 5–9 MHz EVtransducer. The three intersecting orthogonal A, B, C planes (at right angles to each other) are labelled at the center of the four quadrants (white arrow). A 90-degree cut at the A plane center reference point (CRP; yellow line) creates the B plane image, and the horizontal cut through the A plane from the side through the CRP (blue line) creates the coronal C plane. The various ultrasound systems will indicate on the screen where the intersecting orthogonal planes are (red and light blue side arrows). The yellow and blue lines are placed here for emphasis of those indicators.

Fig. 161
Answer the following as related to the anatomic cuts (not the planes of the body):
- a.
On what structure is the CRP placed on all three planes? _____
- b.
What cut is the original sweep plane (A plane)? _____
- c.
What cut is the B plane? _____
- d.
What cut is the C plane? _____
- a.
- 4.
The C plane can be isolated and then rotated upright on the Z-axis as is seen on Fig. 162 . Number the following structures below in order from anterior to posterior:
- a.
Puborectalis muscle complex _____
- b.
Urethra _____
- c.
Anal sphincter central mucosa ______
- d.
Vagina _____
- e.
Internal anal sphincter _____

Fig. 162
- a.
Case 77, Figure 163
- 5.
Fig. 163 . Compare the transperineal pelvic floor images of two patients. Like all patient populations, a large group of individuals is surprisingly varied, and imaging operator skill level and interpretation skill is crucial to optimize the assessment. The level of transducer frequency is paramount for resolution and is also operator dependent. For example, the transducer frequency of the left image is clearly a higher frequency than the right.

Fig. 163
Poor technique may contribute to normal anatomy appearing abnormal in appearance or abnormal anatomy being perceived as normal. When interpreting transperineal pelvic floor exams, assess the images from global to specific. Of course, in the presence of an abnormality, detailed imaging at the area of interest will be necessary. Comparing the two cases, answer the following, for both the left image and right image:
- a.
Is the pelvic floor image symmetric? ______________ ______________
- b.
Is the urethra normal in contour?______________ ______________
- c.
Is there evidence of urethral diverticula? ______________ ______________
- d.
Does the vagina appear as a normal smooth-bordered squared off appearance? ____________ ____________
- e.
Is there any evidence of avulsion? ____________ _____________
- f.
Is the pubovisceralis muscle complex demonstrated? ______________ ____________
- a.
Case 78, Figure 164
- 6.
Fig. 164 is a 2D transperineal image, using a 5–9 Hz EV transducer, of a 46-year-old patient with a history of mesh placement. Answer the following:
- a.
Is the pelvic floor anatomy symmetric? ______________
- b.
Is the urethra normal in contour?______________
- c.
Is there evidence of urethral diverticula? ______________
- d.
Does the thickened mesh have a normal bilateral smooth-bordered appearance? ______________
- e.
Is there any evidence of avulsion? ______________
- f.
Is the entire pubovisceral muscle (PVM) complex demonstrated? ______________
- g.
Is the IAS symmetric in appearance? ______________
- h.
Is the central mucosa (CM) displaced? ______________

Fig. 164
- a.
- 7.
The operator/interpreter of the transperineal urogyn ultrasound examination should be able to look at any out-of-context isolated anal sphincter complex (ASC) transverse cut image and be able to tell:
- •
at what level the image was made
- •
whether the sphincter at that level is intact and, if not,
- •
at what location is it disrupted
- •
whether or not there is elevation of the CM toward the defect
- •
if, at the midlevel, the PVM complex is symmetric.
- •
Normally, the CM is centrally situated unless there is a deviation of the surrounding IAS, which allows the mucosa to shift toward the defect. This is one of the advantages of the transperineal approach as opposed to the endoanal approach, wherein the transducer is placed into the anal canal and circumferentially compresses the CM equally by the transducer.
Which of the following is the most common plane utilized to assess the ASC?
- a.
Coronal
- b.
Sagittal
- c.
Axial
Case 79, Figures 165–174
Consider the following questions for Figs. 165–174 , all of which are of separate patients:
- a.
At what level is the ASC cut (proximal, mid, or distal)? The proximal level appears isolated with no visualization of the PVM complex. The midlevel has distinct PVM complex inferior and lateral to the hypoechoic IAS, and the distal level hyperechoic EAS symmetrically surrounds the relatively hypoechoic IAS. The CM is seen centrally at all levels.
- b.
Is it intact? The IAS or EAS is circumferentially symmetric in the normal appearance. If not, at what level in terms of a clock is the disruption? Describe the disruption as if comparing to hands of a clock. Report, for example, that a “Disruption is noted from 10-2 OC.”
- c.
Is there elevation of the CM toward the defect? Because the transducer is at the perineum and not in the rectum, this adds a secondary finding in the event of IAS or EAS disruption as the mucosa is shifted toward the defect. Contrarily, the CM is circumferentially displaced by the transducer when placing a rectal transducer.
- d.
Are the IAS and/or EAS four quadrants (12-3, 3-6, 6-9, 9-12) symmetric? The normal IAS or EAS appears subjectively symmetric; however, measurements are comparatively the same.
- e.
Does the PVM complex appear symmetric (if at appropriate level)? The convex appearance should be bilaterally symmetric. Accomplishing this is operator dependent, not only for the 2D transperineal approach but also when creating a 3D volume set. A normal ASC can appear quite abnormally asymmetric if improperly performed.
- f.
Is there evidence of a rectal/vaginal fistula? Though this is rare, it should be assessed as part of all exams, and would be seen as a triangularly shaped extension off the IAS extending partially or all the way to the posterior vaginal wall.
- a.
- 8.
Fig. 165 . This is a transperineal ASC image.
- a.
At what level is the ASC cut (proximal, mid, or distal)? _____
- b.
Is it intact? _____
- c.
If not, at what level in terms of a clock is the disruption? _____
- d.
Is there elevation of the CM toward the defect? _____
- e.
Are the IAS and/or EAS four quadrants subjectively symmetric? _____
- f.
Does the PVM complex appear symmetric? _____
- g.
Is there evidence of a rectal/vaginal fistula? _____

Fig. 165
- a.
- 9.
Fig. 166 . This is a transperineal ASC image.
- a.
At what level is the ASC cut (proximal, mid, or distal)? _____
- b.
Is it intact? _____
- c.
If not, at what level in terms of a clock is the disruption? _____
- d.
Is there elevation of the CM toward the defect? _____
- e.
Are the IAS and/or EAS four quadrants subjectively symmetric? _____
- f.
Does the PVM complex appear symmetric? _____
- g.
Is there evidence of a rectal/vaginal fistula? _____

Fig. 166
- a.
- 10.
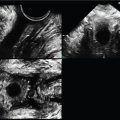
Fig. 167 . This is a transperineal ASC image.
- a.
At what level is the ASC cut (proximal, mid, or distal)? _____
- b.
Is it intact? _____
- c.
If not, at what level in terms of a clock is the disruption? _____
- d.
Is there elevation of the CM toward the defect? _____
- e.
Are the IAS and/or EAS four quadrants subjectively symmetric? _____
- f.
Does the PVM complex appear symmetric? _____
- g.
Is there evidence of a rectal/vaginal fistula? _____
- h.
Comment on the Color Power Doppler vascularity. _____
- a.