, Leonid Tiutin2 and Thomas Schwarz3
(1)
Russian Research Center for Radiology and Surgery, St. Petersburg, Russia
(2)
Department of Radiology and Nuclear Medicine, Russian Research Center for Radiology, St. Petersburg, Russia
(3)
Department of Nuclear Medicine Division of Radiology, Medical University Graz, Graz, Austria
Abstract
Currently, cervical cancer is one of the widest-spread forms of malignant neoplasms. This disease occupies seventh place in incidence among all malignant neoplasms and third place in women (after mammary and colorectal cancers). Recently, a considerable increase in frequency of diagnosing different forms of cervical cancer in young women (up to 40 years old) has been observed.
Currently, cervical cancer is one of the widest-spread forms of malignant neoplasms. This disease occupies seventh place in incidence among all malignant neoplasms and third place in women (after mammary and colorectal cancers). Recently, a considerable increase in frequency of diagnosing different forms of cervical cancer in young women (up to 40 years old) has been observed.
Possible etiologic factors for developing cervical cancer include the early start of sex life, viral (human papilloma virus, HIV and genital herpes virus) and Chlamydia infections, a large number of sexual partners, traumas of the uterine cervix at childbirth and hereditary predisposition.
The main factors determining prognosis in patients with cervical cancer comprise the morphological texture of the tumor and the character and degree of tumor dissemination. It is accepted to distinguish two histological types of cancer of the uterine cervix: planocellular cancer accounts for 95–97% of all malignant neoplasms here, while 4.5% are adenocarcinomas. Undifferentiated cancer, melanoma, lymphoma and sarcoma are observed very seldomly (less than 1% of cases). It has been established that invasive planocellular cancer of the uterine cervix develops from the normal epithelium, passing through all the stages of precancerous dysplasia. Cancer in situ or preinvasive cancer is characterized by minimum signs of atypia and by absence of tumor dissemination beyond the basal membrane of the epithelium of the uterine cervix.
Cancer of the uterine cervix disseminates in three directions: to the vagina, to the uterine body and to the parametrium. In late stages the tumor may infiltrate the pouch of Douglas and urinary bladder. Lymphogenic metastasis occurs through lymph collectors of the parametrium to pelvic, iliac and, in still later stages, to paragastric lymph nodes. Hematogenic metastases of cervical cancer are most often observed in the lungs, liver and bones. In case of exophytic forms, as well as in the presence of mixed and endophytic tumor growth, a high frequency of lymphogenic metastasis is observed, while the vaginal variant of spreading is characterized by a lower metastasis rate. Adenocarcinoma is characterized by early metastasis and relapse (up to 12 months), while for planocellular cancer generalization is possible over 36 months.
The classification of cancer of the uterine cervix is presented in Table 13.1.
Table 13.1
TNM and FIGO classifications for cervical cancer
TNM | FIGO | Surgical-pathologic findings |
|---|---|---|
Categories | Stages | |
TX | Primary tumor cannot be assessed | |
T0 | No evidence of primary tumor | |
Tis | Carcinoma in situ (preinvasive carcinoma) | |
T1 | I | Cervical carcinoma confined to the cervix (disregard extension to the corpus) |
T1a | IA | Invasive carcinoma diagnosed only by microscopy; stromal invasion with a maximum depth of 5.0 mm measured from the base of the epithelium and a horizontal spread of 7.0 mm or less; vascular space involvement, venous or lymphatic, does not affect classification |
T1a1 | IA1 | Measured stromal invasion ≤3.0 mm in depth and ≤7.0 mm in horizontal spread |
T1a2 | IA2 | Measured stromal invasion >3.0 mm and ≤5.0 mm with a horizontal spread ≤7.0 mm |
T1b | IB | Clinically visible lesion confined to the cervix or microscopic lesion greater than T1a/IA2 |
T1b1 | IB1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
T1b2 | IB2 | Clinically visible lesion >4.0 cm in greatest dimension |
T2 | II | Cervical carcinoma invades beyond uterus but not to pelvic wall or to lower third of vagina |
T2a | IIA | Tumor without parametrial invasion |
T2a1 | IIA1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
T2a2 | IIA2 | Clinically visible lesion >4.0 cm in greatest dimension |
T2b | IIB | Tumor with parametrial invasion |
T3 | III | Tumor extends to pelvic wall and/or involves lower third of vagina and/or causes hydronephrosis or nonfunctional kidney |
T3a | IIIA | Tumor involves lower third of vagina, no extension to pelvic wall |
T3b | IIIB | Tumor extends to pelvic wall and/or causes hydronephrosis or nonfunctional kidney |
T4 | IV | Tumor invades mucosa of bladder or rectum and/or extends beyond true pelvis (bullous edema is not sufficient to classify a tumor as T4) |
T4a | IVA | Tumor invades mucosa of bladder or rectum (bullous edema is not sufficient to classify a tumor as T4) |
T4b | IVB | Tumor extends beyond true pelvis |
Regional lymph nodes (N) | ||
NX | Regional lymph nodes cannot be assessed | |
N0 | No regional lymph node metastasis | |
N1 | Regional lymph node metastasis | |
Distant metastasis (M) | ||
M0 | No distant metastasis | |
M1 | Distant metastasis (including peritoneal spread; involvement of supraclavicular, mediastinal, or para-aortic lymph nodes; and lung, liver, or bone) | |
Cancer of the uterine cervix for long time has no clinical manifestations. Sometimes patients complain of abundant bloody or serous discharge from the vagina and hemorrhages. In case of small size of tumor there may be contact hemorrhages, which occur immediately after coitus. Later, pain syndrome appears. Pains are localized in the lumbar area, above the pubes and in the crotch. Pain syndrome usually intensifies when the tumor infiltrates the adjacent organs: the urethra, intestine, and urinary bladder.
13.1 Methods of Diagnosis
Diagnosis of cancer of the uterine cervix is rather simple and is based on the data of gynecologic examination, colposcopy, cytological and histological studies. Schiller’s test with Lugol’s iodine solution, which is done during colposcopy, permits the detection of Lugol-negative areas, suspected of cervical cancer. The pathophysiological basis of the test is a sharp decrease in glycogen content in pathologically changed layers of the integumentary epithelium of the uterine cervix. Oncocytological study consists of examining smears from the vaginal portion of the uterine cervix and cervical canal. Diagnosing is based on dividing smears into five classes according to the Papanicolaou classification:
Class 1 – absence of atypical cells
Class 2 – cells with signs of atypia in small amount
Class 3 – cells with marked signs of atypia
Class 4 – suspicion of malignant process
Class 5 – convincing signs of malignancy
Due to the possibility of false-positive results of oncocytological examination, final diagnosis is made on the basis of data of the histological analysis of biopsy material obtained under colposcopy control.
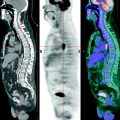
The radiologic diagnosis of cervical tumors is based mainly on the data of ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI). US enables the detection of tumor localization, its size, form, structure and relation to other organs of the small pelvis. Use of intravaginal and intrauterine sensors significantly increases the information value of the method. CT is a poorly informative method of diagnosing in the early stages of the disease. However, in the late stages CT permits diagnosis of the primary tumor, determination of its spread to adjacent organs and the detection remote metastases.
MRI is an informative method of diagnosing cancer of the uterine cervix; it permits not only the detection of the malignant tumor but also the visualization of regional and remote metastases.
However, the main shortcomings of the indicated radiologic methods are based on the difficulty in differentially diagnosing the detected solid masses as well as in assessing the real size of the formation, particularly during treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree