, Leonid Tiutin2 and Thomas Schwarz3
(1)
Russian Research Center for Radiology and Surgery, St. Petersburg, Russia
(2)
Department of Radiology and Nuclear Medicine, Russian Research Center for Radiology, St. Petersburg, Russia
(3)
Department of Nuclear Medicine Division of Radiology, Medical University Graz, Graz, Austria
Abstract
Prostate cancer is one of the most frequent neoplasms in middle-aged and elderly men. In a number of countries this tumor is the second or third most frequent in incidence among all oncological diseases. Mortality from prostate cancer occupies the second place after lung cancer among all oncological diseases.
Prostate cancer is one of the most frequent neoplasms in middle-aged and elderly men. In a number of countries this tumor is the second or third most frequent in incidence among all oncological diseases. Mortality from prostate cancer occupies the second place after lung cancer among all oncological diseases.
Presently some risk factors for this disease are known, such as age, race, genetic factors, nutrition characteristics, hypodynamia, etc. The probability of developing prostate cancer increases after the age of 50 and more than 70% of cases of prostate cancer are detected in males over 65. Up to 40% of males at the age of 60–70 have microscopic cancer of the prostate. Due to some characteristics of clinical course the disease may not have any impact on the patient’s well-being for many years. Only in 10% of cases the latent form of prostate cancer passes to its symptomatic form. It has been established that the risk of developing the disease grows when an excessive amount of animal fats is consumed. Some substances, for example vitamins of the B group, vitamins D and E and the mineral selenium, decrease the risk of developing prostate cancer. Hereditary predisposition to the disease should be taken into account.
Histological studies on prostate cancer have permitted to establish specific injuries preceding the occurrence of the disease. The direct predecessor of invasive adenocarcinoma is prostatic intraepithelial neoplasia (PIN), which can be detected only by way of biopsy. Unlike prostate cancer, in the stage of PIN the basal cell membrane remains intact, surrounding tissues are not affected and the level of prostate-specific antigen (PSA) remains normal.
Prostate cancer is a hormone-dependent tumor, whose growth is conditioned by the influence of androgens, first of all dihydrotestosterone (DHT), a functionally active form of testosterone.
14.1 Pathologic Anatomy and Way of Metastases
Prostate tumors are morphologically divided into epithelial and nonepithelial tumors. The vast majority of prostate tumors (more than 99%) are epithelial; epithelial tumors, in their turn are in 98% of cases represented by adenocarcinoma. Adenocarcinoma is microscopically inhomogeneous. There are acinic cell, small cell (scirrhous), clear cell, ductal and mucinous histological forms of adenocarcinoma of the prostate. Most histological classifications are based on signs of differentiation of prostate cancer. Three tumor gradations are distinguished: highly differentiated, moderately differentiated and lowly differentiated adenocarcinomas. Prostate cancer almost always has an inhomogeneous structure. This is the basis of Gleason’s histological classification, which has received universal recognition. According to the Gleason scale, a grade 1 tumor is characterized by the presence of practically normal glands. As the Gleason scale increases, glandular structures become inhomogeneous, their size and configuration become irregular and tumor boundaries become indistinct. At grade 5, glands are practically absent and the tumor has a solid texture. The sum of grades according to the Gleason scale is composed of the dominant and the second in frequency types of glands; for example, 3 + 5 = 8. The obtained number is an important prognostic criterion permitting conjecture on the degree of dissemination, presence of metastases and to make prognosis of the disease.
Prostate cancer spreads by ways of local invasion, lymphogenic and hematogenic metastases. Local invasion often precedes the emergence of metastases. Tumor most often spreads to the prostatic capsule and affects the base of the urinary bladder and seminal vesicles. Spread of prostate cancer to the urethra is possible. Denonvilliers’ fascia serves as a barrier between the prostate and the rectum; therefore invasion to the rectum is far less frequent. Lymphogenic metastases most often affect obturator lymph nodes. The next frequent localization of metastases is in the internal iliac, presacral and external iliac lymph nodes. There are two ways of hematogenic spread of prostate cancer: arterial and venous. The hematogenic arterial way characterizes prostate cancer metastases to the lungs, liver, brain and bones. The exception is only the bones of the pelvic girdle, whose specific lesion occurs in the venous way. Metastases most often affect the bones. Bone metastases are observed in 80% of patients who die from prostate cancer. In most cases they have an osteoblastic character, even though lytic and mixed lesions are observed as well. The most frequent localizations of bone lesions are the spine, femoral bones and pelvic bones.
In the initial stages prostate cancer does not manifest itself clinically. It is usually detected accidentally during morphological study of material obtained by transurethral resection or prostate biopsy in patients with elevated PSA indices.
The development of symptoms is associated with enlargement of the organ and emergence of regional and distant metastases. The increase in volume of the prostate leads to the development of symptoms of obstruction of the urinary bladder: frequent and difficult urination, feeble stream, etc. The intensity of obstruction symptoms is directly associated with the degree of tumor compression of the urethra. Symptoms of obstruction of the urinary tracts are usually accompanied by a number of other disease manifestations. For example, if the tumor invades into the prostatic urethra, hematuria and painful urination occur. If the sphincter muscle of the urethra is tumor-affected, urinary incontinence develops. Locally spread prostate cancer may compress and spread to the distal section of the rectum. In such cases the disease manifests itself with constipations, tenesmus, hemorrhages, and excretion of mucus from the rectum.
In some patients, clinical manifestations of the disease are determined by metastases to lymph nodes. However, the main motif that brings the patient to take medical advice is pain syndrome caused by bone metastases. Localization of pain sensations usually corresponds to the location of metastases. Metastases to the spine may lead to paralyses and pareses.
14.2 Methods of Diagnosis
The standard diagnosis of prostate cancer is based on the results of digital rectal examination, level of PSA in blood serum and transrectal US. On the basis of these data, transrectal multifocal biopsy of the prostate with ultrasound aiming is administered.
Digital examination of the rectum is the simplest, cheapest and safest method of diagnosing prostate cancer. The characteristic features of this disease are enlargement, changed consistence, presence of dense nodes, asymmetry and disturbance of mobility.
One of the main methods of early detection of prostate cancer is PSA blood test, which should be done annually in all males over 50. If prostate cancer has been detected in relatives, such tests should be implemented starting from 40 years. However, in a quarter of cases prostate cancer can be detected also in case of normal PSA levels in blood serum. This is accounted by particular characteristics of the tumor. Also, increase in PSA level in blood is not always associated with a malignant prostate neoplasm. This index may rise in such diseases as benign hyperplasia of the prostate (adenoma), acute and chronic prostatitis as well as after digital rectal examination of the prostate, coitus, etc. It should be remembered that lowly differentiated prostate adenocarcinoma produces much less PSA than highly differentiated forms of cancer do, which makes interpretation of results of a single test difficult.
US of the prostate not only helps detect the tumor but also may be of aid in performing biopsy of a suspicious area. For screening diagnosis of prostate cancer, the transabdominal method of examining the prostate is widely used. However, the capacities of this method of diagnosis are limited. The indicated methodology permits determination of the size and symmetry of the gland, assessment of the state of the capsule, the volume of residual urine and detection of gross changes in the pelvic organs. At the same time, the detection of subtile changes in the internal structure of the prostate and assessment of the character of pathologic changes are possible only by means of transrectal US examination. The simplicity of performing transrectal US and its high information have significantly extended the possibility of early diagnosis of prostate diseases. A valuable advantage of transrectal US is its ability to provide data on the size of the prostate and on its topographic-anatomic relation with adjacent organs and tissues, the state of its capsule and internal structure. And yet US examination has serious limitations in determining the stage of the tumor process. The information value of transrectal US is confined to a small field. The sensitivity and specificity of a standard transrectal US examination, according to different authors, range from 38% to 58% and from 42% to 60%, respectively (Kattan et al. 1998; Rifkin et al. 1990; Smith et al. 1997).
A new method that has appeared recently, that of US angiography, provides the unique possibility to quickly obtain in a noninvasive way reliable diagnostic information on vessels, and to study the hemodynamics and perfusion of the prostate, which improves the possibilities of diagnosing prostate cancer.
CT is considered to be lowly informative in case of small size of the tumor focus (less than 2 cm) located within the organ, because of small difference in density between tumor tissue and normal tissue. The diagnostic accuracy of CT in detecting a tumor spreading beyond the prostate gland is 24%, while if seminal vesicles are tumor-affected, it is 69% (Hricak et al. 1987). However, in late stages of the disease, spiral CT permits assessment of the dissemination of the pathologic process, in particular presence or absence of tumor tissue infiltration of the urinary bladder and rectum, as well as those of regional and distant metastases.
MRI of the prostate has a number of advantages over CT and transrectal echography. In particular, this method of visualization, due to the possibility of obtaining images in three planes, reflects with high accuracy the size of the prostate, its contours, the topographic-anatomic relations of the prostate with periprostatic organs and tissues. The information value of the examination significantly increases when a rectal coil is used. Endorectal MRI may be a valuable supplement to transrectal US. Images obtained in endorectal examination are characterized by a more distinct differentiation of the zonal structure and capsule, which is particularly important in cases when routine MRI does not permit to precisely determine the boundaries of the tumor node. MRI can diagnose with high accuracy tumor spreading into the perineural tissue, which is of importance for choosing the volume of surgical intervention. The sensitivity of the method is 50%, its specificity being 95%. The accuracy of endorectal MRI makes up approximately 80% (Yu and Hricak 2000). The sensitivity of MRI in detecting lymphogenic prostate cancer metastases, according to some authors, is 51–89%, using special lymphotropic contrast agents the sensitivity increases up to 90% (Bartolozzi et al. 1996; Tempany et al. 1994; Harisinghani et al. 2003). False-negative MRI results in diagnosing lymphogenic metastases of prostate cancer are usually due to unchanged sizes of affected lymph nodes.
Table 14.1 summarizes the efficacy of traditional methods in diagnosing a local relapse of prostate cancer. The most effective in diagnosing local relapses of prostate cancer is MRI and, consequently, preference should be given to this radiological technique.
Table 14.1
Comparison of conventional methods of diagnosis of prostate cancer local recurrence (Schoder and Larson 2004)
Method | Sensitivity (%) | Specificity (%) |
|---|---|---|
DRE | 44 | 91 |
TRUS | 75 | 67 |
CT | 36 | − |
MRI | 95 | 100 |
Radionuclide methods of examination for diagnosing primary tumor lesion in prostate cancer cases have not become widespread. However, there is a radiopharmaceutical (RP), ProstaScint, which is a 111In-labeled mouse monoclonal antibody, 7E11-C5.3, that is directed toward a glycoprotein expressed by prostate epithelium known as prostatic-specific membrane antigen (PSMA).
By means of scintigraphy it is possible to detect not only the primary lesion but also metastatic lesion of regional lymph nodes as well as distant bone metastases. Due to high specificity of examination with monoclonal antibodies, the information value of this method in diagnosing metastatic lesions of the bone tissue is much higher than that of 99mTc-pyrophosphate scintigraphy. Unfortunately, ProstaScint has not become widespread in Russia due to the expensiveness of the RP.
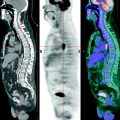
Until recently 99mTc-pyrophosphate scintigraphy of the skeleton was obligatory in the staging of prostate cancer. Scintigraphy of the skeleton is a highly sensitive method of diagnosing metastases to the bones, considerably superior to rentgenography, clinical examination and indices of alkaline phosphatase. False-positive results are observed in patients with bone fractures and degenerative dystrophic diseases of the locomotor system. The frequency of false-negative results does not exceed 1%. The probability of presence of bone metastases in the case of a PSA level lower than 10 ng/mL is virtually equal to zero. In most clinics, if the PSA blood content is less than 10 ng/mL, routine examination of the osseous system is no longer implemented. Nevertheless, implementing radionuclide scanning is obligatory in prostate cancer patients with PSA blood content levels higher than 10 ng/mL, pain in the bones or high readings of alkaline phosphatase.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree