Cervical Carcinoma
Todd M. Blodgett, MD
Alex Ryan, MD
Omar Almusa, MD
Key Facts
Imaging Findings
PET/CT: Intense FDG activity in primary cervical mass, vagina, uterus, parametria; ± lymphadenopathy, visceral metastases
Primary tumor: CEMR
Most cervical SCCA is avid on FDG → high sensitivity for sizable lesions
Evaluation of pelvic and para-aortic LN
LN detection on PET: Sensitivity 75-91%, specificity 93-100%
When PET/CT is performed with diagnostic quality CT, including IV and oral contrast, quality of the overall procedure is improved
Sensitivity and specificity for post-therapy of patients with cervical cancer: 90-93%, 91-100%
Top Differential Diagnoses
Other Female Reproductive Tract Malignancy
Ovarian Cancer
Leiomyoma
Physiologic FDG Activity in Female Reproductive Organs
Urine Contamination
Clinical Issues
Often asymptomatic
Clinical staging accurate in ˜ 60% of patients
Diagnostic Checklist
PET/CT for optimal staging
Physical exam, MR for evaluation of primary tumor
TERMINOLOGY
Abbreviations and Synonyms
Cervical cancer
Cervical carcinoma
Carcinoma of the cervix
Squamous cell carcinoma of the uterine cervix
Locally advanced cervical cancer (LACC)
Definitions
Primary cancer that arises from intraepithelial neoplasia of cervical cells
Squamous cell carcinoma (SCCA): 80%
Adenocarcinoma: 15%
Adenosquamous: 3-5%
Rare: Lymphoma and sarcoma
IMAGING FINDINGS
General Features
Best diagnostic clue
PET/CT
Intense FDG activity in primary cervical mass, vagina, uterus, parametria
± Lymphadenopathy, visceral metastases
CT/MR
Enhancing mass in expected location of cervix
± Extension into vagina, uterus, parametria
± Lymphadenopathy, visceral metastases
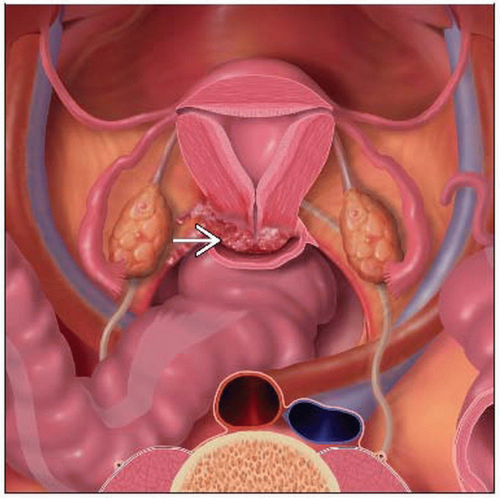
Location
Primary
Cervix
Local
Vaginal mucosa
Extension into endometrium or myometrium
Direct extension into parametrium or adjacent structures
Regional LN
Para-aortic
Common iliac
External iliac
Metastatic
Distant nodes
Organs
Size
Imaging Recommendations
Best imaging tool
Primary tumor
CEMR probably best modality for evaluating the primary lesion
Local and distant metastases
PET/CT (consider with contrast-enhanced CT)
CT reveals ˜ 1/3 para-aortic mets
MR and CT: Moderate sensitivity and specificity for detecting pelvic, para-aortic lymphadenopathy; may fail to identify small metastases
MR for detecting cervical cancer lymphadenopathy: Sensitivity 36-71%, specificity 76-100%
Combination of tumor markers and PET/CT may be highly efficient for detecting recurrence
Protocol advice
FDG excretion through urinary tract and bladder can cause false positive
Bladder voiding prior to imaging important to minimize FDG accumulation within the bladder (may cause artifact in pelvis)
However, primary tumor likely well characterized on anatomic imaging modality (MR)
Image from thighs toward head to minimize excretory FDG within the bladder
Can repeat a bed position after voiding if unclear on initial PET scan
Lasix may be useful, although not routinely used
CT Findings
Local tumor
Primary tumor arises in cervical canal
Extension into peripheral parenchyma can be evaluated with CT
Compared to normal cervical stroma, primary tumor may be hypo- or isoattenuating
Stage IB tumors frequently are isoattenuating to normal cervical tissue (50%)
May not be apparent on CT
Larger lesions will show variable diffuse enhancement pattern seen in delayed images of normal cervix
Tumor extension outside cervix is less likely when cervical margins are smooth and well defined
Enlargement of endometrial cavity with blood, serous fluid, or pus can follow obstruction of endocervical canal status post radiotherapy
Necrosis or prior biopsy of lesion may produce intratumoral gas
Poorer outcome associated with cervical enlargement > 3.5 cm and an AP size > 6 cm
Extension/metastasis
CT useful for the depiction of
Adenopathy
Pelvic side wall extension
Advanced bladder and rectal invasion
Ureteral obstruction
Extrapelvic spread of disease
Tumor extension within 3 mm of pelvic side wall fulfills criterion for invasion
Tumor extension into uterine body careful evaluation for metastic spread
Ureteral encasement may result secondary to tumor extension into parametrium
Ureteral encasement is specific for parametrial invasion
Stage IIIB disease indicated by presence of hydronephrosis
Parametrial invasion may also result in perivascular invasion and uterosacral ligament thickening
Muscular enlargement and enhancing soft tissue mass may be seen with frank invasion of piriformis and obturator internus
Direct extension to pelvic bones results in bony destruction
Tumor may encase and narrow iliac vessels
Signs of bladder or rectal involvement
Intraluminal mass
Loss of perivesical or perirectal fat plane
Asymmetric nodular thickening of bladder or rectal wall
Fistula formation with intravesical air
Cystic appearance of recurrent pelvic disease can be confused with post-surgical fluid collection
Recurrence has minimal soft tissue and generally occurs more than 6 months after surgery
Distant metastases
30% of patients have liver metastases
Appear as solid masses with variable enhancement
15% of patients have adrenal metastases
35-40% of patients with thoracic metastatic disease have this presentation
Multiple pulmonary nodules may represent thoracic metastasis
Minority of cases demonstrate cavitation
Lymph nodes
Cutoff for suspicion of malignancy is size > 1 cm in short axis
90% of metastatic retroperitoneal LNs are normalsized
Sensitivity for retroperitoneal metastases: 44%
Sensitivity for para-aortic metastases: 34%
Enhancement pattern rarely helps differentiate benign from malignant disease
Central necrosis has ˜ 100% PPV
Parametrial station is usually the first to be infiltrated by disease
Tumor spreads through 3 lymphatic pathways most commonly
Laterally along external iliacs
Hypogastric route along internal iliacs
Presacrally along uterosacral ligament
Each pathway leads to common iliac lymph nodes, then leads to para-aortic nodes
Nuclear Medicine Findings
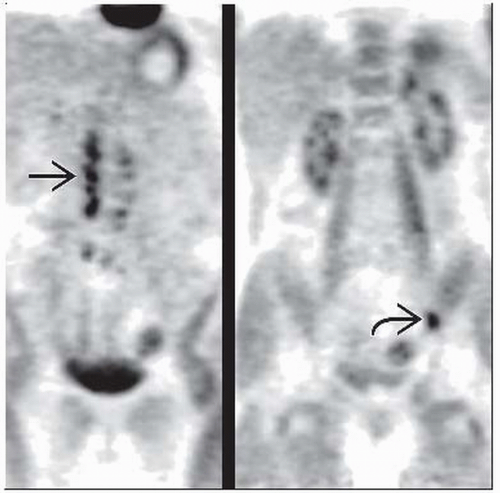
PET/CT performed with diagnostic CT
Quality of the overall procedure is improved
Much easier to identify focal abdominopelvic lesions from opacified bowel if oral contrast is used
Initial diagnosis
Evaluation of primary cervical tumor
Generally not performed to look at primary tumor
However, most cervical SCCA is FDG-avid → high sensitivity for sizable lesions
PET/CT reliable in advanced disease
May help avoid unnecessary operations
May help with radiation therapy planning
Primary tumor SUV ≥ 10 associated with significantly lower 5 year disease-free survival than tumors with lower SUV (52% vs. 71%)
Overall survival comparable whether SUV < or > 10
Staging
Evaluation of pelvic and para-aortic LN
LN detection on PET: Sensitivity 75-91%, specificity 93-100%
PET sensitivity for advanced disease 87%, specificity 100%
Low sensitivity in LN < 1 cm
Pelvic LN: Sensitivity 46%, specificity 91%
Para-aortic LN: Sensitivity 40%, specificity 99%
Presence or absence of para-aortic LN on PET correlates most significantly with disease-free survival
Knowledge of para-aortic lymph node status is crucial for treatment planning
Invasive surgery, with laparotomy or laparoscopy, has traditionally been used
Evaluation of distant metastases
In one study, ˜ 8% of patients had distant supraclavicular lymphadenopathy detected only by PET
PET/CT
Useful supplement to clinical staging procedures
Sensitivity of 75% and specificity of 87-96% for detection of nodal metastases in the pelvis
High sensitivity/specificity for newly diagnosed cervical cancer with FIGO stage IB or higher
Useful for planning treatment strategy
Histologic confirmation of results should be obtained prior to change of treatment plan
Can be used for biopsy guidance
PET/CT vs. conventional imaging for detecting metastatic lymph nodes
Sensitivity 97% vs. 40%
Specificity 94% vs. 65%
PPV 97% vs. 70%
NPV 94% vs. 34%
False positives
Inflammatory/infectious lesions
Pulmonary tuberculosis
Acute cholangitis
Physiologic uptake
Physiologic uptake in bowel, vessels, ureter
Ovarian uptake, depending on phase of cycle: Around ovulation and early luteal phase
Functional ovarian cysts, such as hemorrhagic corpus luteum cyst, may mimic lymph node metastases
Other
Post-operative changes
Benign thyroid tumor
False negatives
Low tumor volumes
Restaging
Sensitivity and specificity for post-therapy of patients with cervical cancer: 90-93%, 91-100%
DIFFERENTIAL DIAGNOSIS
Other Female Reproductive Tract Malignancy
Endometrial cancer
Ovarian cancer
Leiomyoma
Variable FDG avidity, ranging from very minimal to intense
Often distinguishable from cervical mass on CT portion of PET/CT
Physiologic FDG Activity in Female Reproductive Organs
Menstruation: FDG activity in endometrial cavity, less frequently in vagina, associated with normal menstruation
Clinical history of current menstruation important
May need ultrasound, clinical correlation if patient not currently menstruating
Ovaries: Benign and malignant etiologies
May need ultrasound to distinguish
Urine Contamination
May need ultrasound to distinguish
Incontinence can cause contamination of external genitalia
Endometrial Carcinoma
Usually spares cervix, though may spread to cervix if diagnosed late
Generally older patient population
PATHOLOGY
General Features
General path comments
Glut-1: Overexpressed in cervical carcinoma, may be correlated with tumor grade
Absence of glut-1 correlated with improved metastasis-free survival
In women with LN positive cervical carcinoma, 80% of involved LN are < 1.0 cm in greatest dimension
Etiology
Likely multifactorial
Associated with human papillomavirus (HPV) infection (strains 16, 18, 31, 33, 45)
Other risk factors
Multiple sexual partners
Sex before age 18
Tobacco use
Diethylstilbestrol
Epidemiology
In USA: ˜ 10,000 cases per year
˜ 1/3 die of disease
HPV vaccination programs widely instituted with goal of eradicating cervical cancer
However, cervical cancer remains an important public health problem
Worldwide:
> 300,000 cases diagnosed per year
2nd most frequently diagnosed gynecologic malignancy in women
50% mortality rate
5 year recurrence: 28%
5 year overall mortality: 27.8%
Staging, Grading, or Classification Criteria
In contrast to other gynecologic malignancies, cervical cancer is staged clinically
FIGO staging
Allows only the following diagnostic tests to be used in determining the stage
Palpation, inspection, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, and intravenous urography
X-ray examination of the lungs and skeleton, and cervical conization
Most important limitation: Does not provide any information about retroperitoneal lymph node status
Especially para-aortic nodal metastases
Discrepancies between FIGO staging and surgical/histopathologic findings
Occurs in about 30% of patients with locally advanced cervical cancer
Clinical staging accurate in ˜ 60% of patients
Undiagnosed lymphadenopathy is a major problem
American Joint Committee on Cancer (AJCC) staging
Stage 0
Carcinoma in situ
Stage I
Confined to uterus
Stage II
Beyond uterus, but not to pelvic side wall, lower third of vagina
Stage IIIA
Extends to pelvic wall, lower third of vagina
Causes hydronephrosis/nonfunctioning kidney
Negative lymph nodes (LN)
Stage IIIB
Extends to pelvic wall, lower third of vagina
Causes hydronephrosis/nonfunctioning kidney
Positive LN
Stage IVA
Beyond true pelvis, bladder mucosa, rectal mucosa
Positive LN
Stage IVB
Distant metastases
Pre-treatment surgical staging issues
Risks of laparotomy for nodal staging include
Bowel obstruction
Infection
Vascular damage
Ureteral injury
Fistula formation
Lymphocyst/lymphedema
Thrombophlebitis
Surgical staging results in treatment modification in 18-44% of patients
Negative sentinal lymph node biopsy accurately predicts negative status of retroperitoneal lymph nodes in early cervical cancer
NPV: 92-97%
Sentinal node biopsy has limited value in locally advanced disease due to high false negative rate
Many centers defer surgical staging due to high morbidity
CLINICAL ISSUES
Presentation
Demographics
Age: Primarily affects younger women, although can be seen at any age
Natural History & Prognosis
5 year survival
No lymphadenopathy: 57%
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree