Chapter 23 Chest and thoracic contents
• Suspected pulmonary embolism
• Suspected pericarditis/pericardial effusion, myocarditis, heart failure
• Suspected heart valve disease
Despite the reduction in referrals resulting from efforts to cut the numbers of unnecessary medical irradiations,2,3 it can be seen that there is still a wide range of referral reasons that are considered valid. Plain radiography of the chest was used more extensively in the 20th century than today and is no longer justified in the following cases:
• Non-cardiac related chest pain
• Preoperative assessment (‘routine’, in patients who are not considered at risk from administration of anaesthetic)
• Screening medicals (with exception of high risk immigrants and those who need employment-specific imaging; RCR guidelines give an example of this as ‘deep sea divers’)
Although anecdotal evidence shows that chest radiography has certainly been discontinued from the non-recommended list above, an internet search during the writing of this text did show that there is evidence that some hospital protocols still include recommendation for ‘routine’ chest radiography in some cases.4
The PA chest projection and comments on its implementation
Erect
1 Undertaking the projection in the erect position allows for demonstration of unnaturally located fluid, which finds its natural level within the thoracic cavity and is well demonstrated as more dense in appearance than the air-filled lung tissue. In the supine position this pleural fluid will lie posteriorly in a layer which will show as an increased density over the hemithorax in which it lies; this density may overlie other pathology.5 Wherever possible radiographers should undertake chest radiography erect; in the case of the infirm patient an erect sitting projection is a suitable alternative and this can be achieved using a stool or, preferably, a commercially built chair designed for stability and versatility. These chairs have wheels for manoeuvrability, wheel locks for stability, and removable back and arms for versatility. A PA erect chest can therefore be undertaken with the chair back removed but chair arms in place (Fig. 23.1A,B,C,D). For patients who must remain in a wheelchair, on a trolley or bed, an erect anteroposterior (AP) projection can be undertaken.
2 Inspiratory effort is more effective when the thorax is in the erect position.
PA
1 The PA projection allows forward tilt of the thorax to elevate the lung apices above the clavicles. Tuberculosis (TB) frequently manifests itself in the lung apex, thereby indicating the importance of clearing this area from the image of the clavicles (although a lordotic projection will clear the clavicles entirely above the apices, allowing visualisation of the lung apex without superimposition of the clavicles over the lower apical portion). Numbers of reported cases of TB in the 21st century are relatively insignificant in the UK compared to the 17th, 18th and 19th centuries and the first half of the 20th century, but it is by no means non-existent; after a period of increase the incidence rate per thousand (global population) levelled off in the period around 2005, but actual numbers increased because of population increase.6 In the UK, numbers of recorded TB cases fell to their lowest level in 1987, reaching the low plateau of 5000–6000 cases per year for some years afterwards; the first signs of a very slight increase were noted around 1997,7 increasing until 2009 but then falling again in 2010.8
In addition to revealing the lung apices, forward tilt also avoids a lordotic appearance of the image; lordosis affects the accuracy of cardiothoracic ratio (CT ratio) assessment for cardiomegaly.
2 The chin can be supported clear of the apices by its position resting upon the upper border of the image receptor (IR).
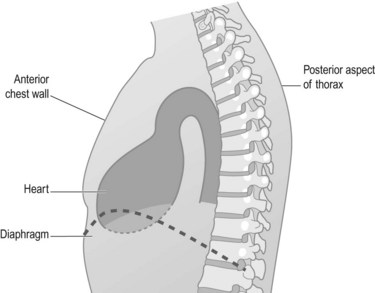
3 As the heart lies anteriorly within the thorax (Fig. 23.2) the degree of magnification of this organ is minimised in the PA position; again, in assessment of the CT ratio, minimal magnification is preferred.
4 In an adult woman, compression of breast tissue against the IR will reduce body thickness and ensure the lowest exposure factor settings can be used.
5 It is acknowledged that the use of PA projections reduces the dose to anteriorly positioned radiosensitive organs, owing to the higher average beam energy after travelling through the posterior portions of the chest (thereby producing less absorption in these anterior organs). The sternum and female breasts lie within the field of primary radiation and will also benefit from reduction of dose in the PA position.
6 Obliquity of the X-ray beam at the periphery of the thorax will assist projection of the scapulae away from the area of the lung fields. The angle of this obliquity is likely to vary, as the distance of the scapulae from the central ray will differ according to the width of the chest, but it is likely that this angle will be quite small, even in the patient who has a wide chest. Examples of such angles of obliquity of the beam at 2 m focus receptor distance (FRD), at different points around the beam centre (when using a central ray at 90° to the IR) and using geometric calculations, are given as approximate figures in the following table (figures are given to the nearest decimal point).
| Distance from centring point (cm) | Angle of oblique rays at this point (2 m FRD) |
|---|---|
| 12 | 3.4° |
| 17 | 4.8° |
| 21.5 | 6.2° |
Comments on exposure technique selection
In order to image the lung tissue adequately in contrast to air within the thorax, for the most part of the 20th century exposure factors with a fairly low kVp were traditionally selected for chest radiography. These were usually in the range of 60–75 kVp and accompanied by values of 6–12 mAs. However, structures overlying dense areas such as the heart failed to be demonstrated owing to the low penetration of the beam. EC guidelines in 1996 not only stressed the importance of using a high-energy beam in order to penetrate such areas, but also emphasised the reduction of absorbed dose by using high kVp techniques, namely 125 kVp.9 These high kVp techniques may well require the use of an antiscatter grid or bucky, and use of automatic exposure devices (AEDs) is recommended in the 1996 EC guidelines, selecting the right chamber.
Positioning choices for the PA projection
Direction of central ray
It appears that, internationally, beam angulation is not in widespread use and the UK appears to be the area most likely to use it.10 Caudal angulation has been suggested as inappropriate as the (minimal) obliquity of the beam used is actually likely to reduce the amount of posterior inferior lung tissue demonstrated above the diaphragm on the image (this is despite the common belief that its use ‘opens out the lung fields’ or maximises the amount of lung tissue seen above the diaphragm).11 The effectiveness of small angles has also been challenged.12 In addition, caudal angulation takes the beam direction towards the abdomen, thereby potentially increasing radiation dose to this region. To summarise, the use of caudal angulation does not offer improvements in image quality, may reduce the amount of lung tissue seen above the diaphragm, and potentially adds to the radiation burden for abdomen and gonads; it is can therefore be considered pointless.
Centring point
As indicated, suggestions for centring have varied from T4 to T7,13–16 with the middle of the IR, chest or thorax also mentioned in some texts.15–17 In some cases more than one suggestion is given. So which is most appropriate? An additional question is: do texts specifying a vertebral level mean the body or the spinous process of that which is indicated? This is an important point when it is remembered that the body of a thoracic vertebra lies level with the spinous process of the one above it. It is also important that a suggested centring point be located as a palpable surface marking, so in this chapter spinous process will be referred to.
One suggestion for accurate assessment of the centring point involves using a ruler to measure the radiographer’s hand span in order to help locate a centring point (given in centimetres and inches from T1) for use on the ‘average’ male and ‘average’ female,18 but how can this be standardised or accurate when the assessment (and opinion) of ‘average’ is likely to vary from radiographer to radiographer, and any set measurement in centimetres or inches varies in its distance down each individual spine from a given point?
Centring points are most effective when simply in the centre of the area of interest, whether or not tube angle is used, and this should similarly apply to the chest region. Considering the issue of using a sensible centring point for the chest, the previous edition of this book suggested a move from traditional centring points as high as T6 (which lies only one-third of the distance from apices to costophrenic angles) after research showed that this point almost never lies in the middle of the area of interest: indeed, study of PA chest images has shown that the vertebral body that most frequently lies level with the midpoint of the lungs is the body of T8 (spinous process of T7).19
In support of the question regarding the ability to accurately select a centring point at 2 m, it has been found that radiographers frequently believe that they use a specific centring point for PA projection of the chest but in reality ensure that the area of interest lies centrally over the IR. They then centre to the middle of the IR and the area of interest.20 This provides a well-centred image and suggests that radiographers are accurate at centring appropriately at 2 m, but not at selecting the point they believe they use. For this reason the description of technique and centring point in this book reflects a combination of this second method and selection of a specific centring point.
PA chest projection (Fig. 23.3A,B,C)
Positioning
• A lead rubber apron is applied to the patient’s waist
• The anterior aspect of the chest is placed in contact with the IR
• The height of the IR is adjusted until the whole of the thorax is included in its perimeter. The beam is collimated to the patient’s thorax
• The patient’s feet are separated slightly, for stability
• The patient leans forward and the chin is raised slightly and rests against the IR, or upon its upper border if a cassette type IR is used
• The median sagittal plane (MSP) is perpendicular to the IR; this is checked by ensuring the sternoclavicular joints are equidistant from the IR. The MSP is coincident with the long axis of the IR
• The elbows are flexed and the backs of the hands are placed on the sides of the waist, resting on the lateral aspects of the iliac crests. The elbows are then gently pressed forward towards the IR, to clear the scapulae from the lung fields on the image. Ensure that the hands are actually on the lateral aspect of the waist, as this maximises forward movement of the shoulders; positioning of the hands on the posterior aspect significantly reduces the range of forward movement
• A PA marker is most frequently used, on the relevant upper corner of the radiation field
Collimation
First thoracic vertebra, first rib, lateral margins of ribs 2–10, costophrenic angles
Criteria for assessing image quality
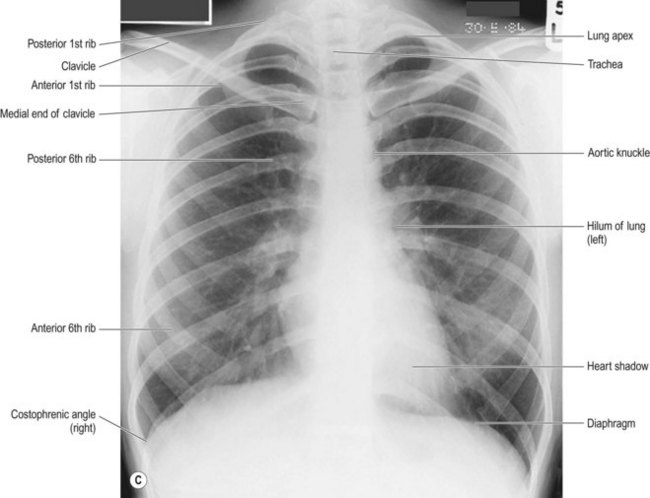
• First thoracic vertebra and first rib, lateral rib margins and costophrenic angles are demonstrated. The costophrenic angles must be demonstrated above the collimated field
• 3–5 cm of apical tissue is projected above the clavicles
• Posterior aspects of the ribs are slightly inclined from the thoracic spine down towards their lateral borders
• Anterior aspects of the ribs are inclined more steeply than the posterior aspects, from their lateral borders down towards the midline
• Medial ends of the clavicles are equidistant from the midline of the thoracic vertebrae
• Scapulae are cleared from the lung fields
• Six anterior or nine posterior ribs are demonstrated above the diaphragms
• Sharp image demonstrating the vascular pattern of the lungs to the periphery in contrast with the air-filled lung tissue and dense structures of the hila and mediastinum (heart, aorta). Trachea and proximal bronchi should be visible, as should the retrocardiac lung and mediastinum. The thoracic vertebrae (intervertebral disc spaces) should be evident through the cardiac image. Diaphragms and costophrenic angles should be clearly seen. These exposure factor criteria relate to high kVp technique as outlined by EC 96 regulations.3 For images produced with kVp lower than 85–90, penetration is assessed by checking that the spinous process of T4 is adequately seen in the midline as in Figure 23.3C. (Note that the patient positioning in Fig. 23.3C is superior to that in Fig. 23.3B.)
Adherence to quality standards outlined above is particularly important in the PA chest radiograph:
• Poor inspiratory effort, lordosis and rotation will all affect the accuracy of CT ratio assessment. Rotation will also cause hilar markings to appear more prominent on one side of the thorax and potentially mimic the suggestion of pathology. Density in each lung will appear to be different in the rotated patient. A rotated position will also cause the mediastinum to appear widened and the trachea to appear shifted laterally.5,21
• It is vital to include all the outline of the whole of the costophrenic angle on each side, as a significant volume of 100 mL of pleural effusion may be present before blunting of the costophrenic angle will be demonstrated.5 This is related to the fact that the diaphragm level sits lower on the posterior aspect of the thorax in relation to its anterior portion. Pleural fluid can collect in this lower posterior portion before it is actually demonstrated in the anterior portion and on the PA erect chest radiograph, when it is seen to cause blunting of the costophrenic angle as its earliest appearance.21 Although the lateral radiograph is more sensitive than the PA when demonstrating pleural effusions, most often a good-quality PA is the first indication that the lateral will be necessary.21 It is therefore essential that the PA image includes the whole costophrenic angle to ensure that the earliest radiographic signs of pleural effusion can be noted as soon as possible.
| Common errors | Possible reasons |
|---|---|
| Medially positioned soft tissue shadow, between and/or overlying the apices | Chin not raised adequately |
| Apices inadequately cleared above the clavicles; posterior and anterior aspects of the ribs flattened | Patient is lordotic, i.e. not leaning forward towards the IR |
| Medial ends of the clavicles not seen at an equal distance from the thoracic vertebrae | Patient is rotated. The medial end of the clavicle furthest from the vertebrae corresponds to the side rotated away from the IR. Any evidence of scoliosis? If the patient has scoliosis, it may not be possible to ensure the clavicles lie equidistant from the midline22 |
| Scapulae overlying upper, lateral aspects of lung fields | Elbows and shoulders not pushed forward adequately, or patient has relaxed their arm position Patients with limited shoulder movement may not find it possible to fully comply with the required action; try extending the patient’s arms in forward abduction, with internal rotation at the shoulder |
| Fewer than six anterior ribs or nine posterior ribs are demonstrated above the diaphragms | Miscounted ribs; check again. The first and second ribs cross over superiorly on the image and can sometimes be erroneously counted as one, rather than two. A tip when checking rib numbers is to assume that the posterior aspects of the first and second ribs appear to cross over, like a kiss on a birthday card – so always ‘count the kiss’ first and remember that the kiss = ribs one and two. Counting the thoracic vertebrae is another method that can be used to identify posterior ribs and confirm rib number |
| Poor inspiratory effort. Obese patients or patients with dyspnoea may find improvement difficult | |
| Any evidence or history suggestive of infective or cardiac disease, lobar collapse, lobectomy, subphrenic abscess, phrenic nerve paralysis or upper abdominal mass? These are likely to affect diaphragm height and improvement may not be possible |
AP erect chest (Figs 23.4, 23.5)
The AP erect chest is undertaken when a patient is too ill or frail to stand or sit PA erect.
Positioning
• A patient who can sit on a chair sits with their back to the IR (Fig. 23.4)
• For a patient who presents on a trolley or bed the IR is (a) brought to the back of the patient (digital plate technique), (b) placed in the erect holder or (c) supported by a large 45° pad which rests on the raised back of a trolley or bed (Fig. 23.5)
• The posterior aspect of the chest is placed in contact with the IR
• The height of the IR is adjusted until the whole of the thorax is included in its perimeter. Ensuring that the first thoracic vertebra is below the upper border of the receptor will ensure that the lung apices are included at the top of the image
• The patient sits, supported with their back against the IR
• A lead rubber apron is applied to the patient’s waist
• The beam is collimated to the patient’s thorax and its upper border positioned level with the upper border of T1
• A small radiolucent pad is placed behind the shoulders to reproduce the slight elevation of the lung apices above the clavicles achieved in the PA position. The chin is raised slightly and the MSP is coincident with the long axis of the IR
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree