The chest wall is a complex anatomic structure composed of muscles, bones, joints, and soft tissues that make up the area of the body between the neck and the abdomen. Pathologic processes that may involve the chest wall include congenital and developmental anomalies, trauma, inflammatory and infectious diseases, and soft tissue and bone tumors. Because the clinical presentation of patients with chest wall disorders is diverse and nonspecific, imaging plays a key role in establishing the diagnosis. Diseases that affect the chest wall are difficult to evaluate with radiography. The introduction of cross-sectional imaging techniques, including computed tomography (CT) and magnetic resonance imaging (MRI), has enabled precise localization of chest wall lesions and, in some cases, definitive diagnosis. 18 F-fluorodeoxyglucose (FDG)–positron emission tomography (PET)-CT provides information regarding the metabolic status of chest wall masses but adds only limited additional diagnostic information.
- •
It is formed by bones, joints, and soft tissues located between the neck and the abdomen.
- •
It is involved in developmental anomalies, trauma, inflammatory diseases, and neoplasms.
- •
Chest wall tumors may originate in the skeleton or soft tissues.
Normal Variants, Congenital Diseases, and Chest Wall Deformities
Congenital rib anomalies may be found on 1% to 2% of chest radiographs. Most of these anomalies are isolated findings that occur sporadically and lack clinical significance. Representative examples include, among others, cervical rib, bifid or forked rib, fused ribs, hypoplastic rib, pseudoarthrosis of the first rib, and intrathoracic rib.
A cervical rib is a supernumerary rib that usually arises from the seventh cervical vertebra ( Fig. 79.1 ). It is present in about 0.5% of the general population and is bilateral and often asymmetric in 45% to 70% of cases. When unilateral, it is generally on the right. Most cervical ribs are detected incidentally, may articulate with the superior aspect of the first rib, and are asymptomatic. In less than 10% of patients, cervical ribs may result in thoracic outlet syndrome, which consists of symptoms resulting from pressure on nerves and vessels at the thoracic inlet, including paresthesias, pain, muscular atrophy, and claudication in the ipsilateral limb. Other anatomic causes of thoracic outlet syndrome include an abnormal scalene muscle, congenital fibromuscular bands, and an elongated transverse process of the seventh cervical vertebra.

Rib notching usually affects the lower margin of one or more ribs. The most common and important cause is coarctation of the thoracic aorta. The notches result from rib erosion by dilated intercostal arteries taking part in collateral arterial flow. These arteries may become extremely tortuous and may extend to and erode the superior aspects of contiguous ribs. Rib notching secondary to coarctation of the aorta seldom is seen in patients before age 6 to 7 years and usually is not well developed until the early teens. Focal rib notching also may be due to an intercostal nerve tumor ( Fig. 79.2 ).
- •
Clinical signs: pain in the neck and shoulder area, paresthesias, and weakness in the arm
- •
Pathogenesis: compression of nerves (90%) and/or vessels at the superior thoracic aperture
- •
Causes: trauma, postural distortions, and congenital conditions (cervical rib, scalene triangle, congenital fibromuscular bands)
- •
Differential diagnosis: carpal tunnel syndrome, spinal disorders with nerve root compression, cord tumors, brachial plexopathy, and neuromuscular disorders
- •
Magnetic resonance angiography: useful, noninvasive, and safe method for evaluating the subclavian vessels if vascular compression is suspected

Poland Syndrome
Poland syndrome is a rare autosomal-recessive condition classically consisting of the combination of unilateral partial or complete absence of the pectoralis major muscle and an ipsilateral hypoplastic hand with simple syndactyly and short fingers. The incidence has been estimated at between 1 : 30,000 and 1 : 80,000 of live births. Bilateral involvement is rare. It is three times more common in boys than in girls and involves the right side in 75% of patients. Associated conditions include osseous dysostoses affecting the ipsilateral hand (brachymesophalangy with syndactyly, biphalangy, ectrodactyly), pectus excavatum, anomalies of the upper limb, and other anomalies of the anterior chest wall (absence of the pectoralis minor muscle, hypoplasia of latissimus dorsi and serratus anterior, hypoplasia or aplasia of nipple and breast, lung herniation, and hypoplasia of hemithorax and ribs). Increased incidences of leukemia, non-Hodgkin lymphoma, lung cancer, and breast cancer have been reported in these patients.
Chest radiography usually shows unilateral hyperlucency with absence of the normal axillary fold on the affected side. Rib deformities are found occasionally ( Fig. 79.3 ). The diagnosis usually can be established on CT or MRI, both of which show absence or hypoplasia of pectoral girdle musculature (see Fig. 79.3 ). With these techniques, absence of the sternocostal head of the pectoralis major muscle is always noted, and associated chest wall defects are best depicted.

Differential diagnosis of a diffuse hyperlucent hemithorax on chest radiograph includes radiographic artifact, patient rotation, extrapulmonary conditions (Poland syndrome, previous mastectomy, contralateral pleural effusion, and contralateral soft tissue thickening), pneumothorax, and pulmonary conditions (Swyer-James-MacLeod syndrome, overinflation, and unilateral diminished pulmonary blood flow owing to vascular abnormality or partial bronchial obstruction).
Autosomal-recessive disorder characterized by:
- •
Unilateral partial or complete absence of pectoralis major muscle.
- •
Common association with other anomalies of chest wall or ipsilateral upper limb.
- •
Increased radiolucency of one hemithorax on posteroanterior chest radiography.
- •
Computed tomography and magnetic resonance imaging evaluation may help reconstructive surgical planning.
- •
Pectus Excavatum
Pectus excavatum, also known as funnel chest, consists of depression of the anterior chest wall of variable severity that may be mild, moderate, or severe. It is the most common chest wall deformity, occurring in approximately 1 in 1000 live births with a strong male predominance (3–5 : 1). Approximately 90% of patients with developmental chest wall disorders have pectus excavatum. A family history is known in about 35% to 45% of cases. Pectus excavatum is generally present at birth, or it arises shortly thereafter. It is often progressive, and the depth of sternal depression increases as the patient grows, especially during puberty. Pectus excavatum can be associated with other congenital abnormalities, including scoliosis (15%), osteogenesis imperfecta, Ehlers-Danlos syndrome, diaphragmatic abnormalities, and mitral valve prolapse (20%–60%). In 2% of patients it is associated with congenital cardiac anomalies. Approximately 2% of patients with this condition have Marfan syndrome; these patients typically have the most severe forms of pectus excavatum.
Patients with pectus excavatum are usually asymptomatic or present with chest or back pain, frequently exacerbated by exercise. Physical examination reveals sternal depression so that ribs protrude more anteriorly than the sternum.
On posteroanterior chest radiography, pectus excavatum causes obscuration of the right heart border. The heart is displaced to the left and rotated, and a spurious cardiomegaly may be noted. On lateral chest radiography a depression and deformity of the lower portion of the sternum may be noted ( Fig. 79.4 ). The severity of the defect can be best quantified with CT or MRI. A “pectus or Haller index” (transverse thoracic diameter/anteroposterior thoracic diameter) higher than 3.25 usually requires surgical correction.

The differential diagnosis of obscuration of the right heart border on posteroanterior chest radiography includes right middle lobe atelectasis, right middle lobe pneumonia, large mediastinal fat pad, and Morgagni hernia. In all these conditions the lateral radiograph shows a normal sternum.
Pectus Carinatum
Pectus carinatum, also known as pigeon breast, is a protrusion deformity of the anterior chest wall consisting of anterior displacement of the sternum. It may involve the body of the sternum or, more rarely, the manubrium (chondromanubrial prominence). Pectus carinatum is less frequent than pectus excavatum (1 : 5) and accounts for 5% to 7% of all chest wall deformities. It occurs more frequently in men than women (4 : 1); a family history of chest wall deformities is present in about 25% of cases.
Patients with pectus carinatum are usually asymptomatic. Exertional dyspnea or cardiac arrhythmias may occur. The diagnosis is established on the basis of physical examination. Lateral chest radiography shows anterior prominence of the sternum.
Kyphoscoliosis
Kyphoscoliosis is an abnormal posterior (kyphosis) and lateral (scoliosis) curvature of the thoracic spine. Approximately 80% of cases are idiopathic. Congenital causes include, among others, type 1 neurofibromatosis, hemivertebra, Friedreich ataxia, muscular dystrophy, Morquio syndrome, and Marfan syndrome. The paralytic group includes spinal deformities secondary to poliomyelitis, muscular dystrophy, or cerebral palsy.
Severe forms of kyphoscoliosis cause decreased compliance of the lung and chest wall and result in restrictive lung disease with hypoventilation, hypoxic vasoconstriction, and eventually pulmonary hypertension, cor pulmonale, and respiratory failure. In cases of severe kyphoscoliosis the chest radiograph is difficult to evaluate because of rotation of the thorax and heart. The scoliotic curvature is usually convex to the right. About 60% of patients with type 1 neurofibromatosis have kyphoscoliosis, usually involving a short segment of the lower thoracic spine.
Blunt Chest Trauma
Blunt chest trauma most commonly results from high-energy mechanisms, such as motor vehicle accidents, motorcycle collisions, and falls. Motor vehicle collisions are responsible for 80% of cases of blunt chest trauma and are associated with a wide range of injuries, many of which are life threatening ( Fig. 79.5 ). Rib fracture is the most common thoracic injury, present in 10% of all blunt chest traumas and almost 40% of patients who sustain severe nonpenetrating trauma. Posteroanterior chest radiography should be the initial, and often the only, imaging study in patients with suspected rib fracture after minor trauma. In the workup of patients with high-mechanism blunt trauma, CT is more sensitive than radiography and may demonstrate traumatic injuries in patients with “normal” chest radiographs. Blunt chest trauma is discussed in further detail in Chapter 67 .

Inflammatory and Infectious Diseases
There are a wide variety of inflammatory and infectious diseases that can affect the chest wall. These lesions range from inflammatory conditions of uncertain etiology to acute or chronic infections involving bone, joints, or soft tissues. Infections include pyogenic, tuberculous, fungal, and some other unusual infections. The most common infections are those that follow median sternotomy. Infections and hematomas may affect the presternal (cellulitis, sinus tracts, abscess), sternal (osteomyelitis), or retrosternal (mediastinitis, abscess) compartments. Although radiography remains the first imaging method in suspected cases of chest wall infection, ultrasound, CT, and MRI are all useful and complementary; bone destruction is more accurately detected with CT, whereas soft tissue involvement is better visualized with ultrasound and MRI. Infections in the presternal or retrosternal compartments manifest as stranding, sinus tracts, soft tissue thickening with gas bubbles, or fluid collections with peripheral enhancement (abscess). Sternal osteomyelitis must be suspected when soft tissue anomalies are associated with bone destruction, dehiscence, or severe demineralization ( Fig. 79.6 ).

Primary chest wall soft tissue infections are rare and can occur either by direct inoculation (puncture) or by contiguous spread from other areas and occasionally by hematogenous spread of infection. Soft tissue infections may be classified as necrotizing fasciitis, when they involve the subcutaneous fat and superficial fascia, and pyomyositis, if they involve the muscles alone.
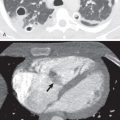
Necrotizing fasciitis is a rapidly spreading infection of the subcutaneous tissue characterized by spontaneous necrosis and gas formation. CT scans provide superior information about the true extent of disease and associated fluid collections, thus facilitating correct diagnosis and treatment ( Fig. 79.7 ).

Empyema necessitatis results from leakage of empyema through the parietal pleura with discharge of its contents into the subcutaneous tissues of the chest wall ( Fig. 79.8 ). Although tuberculosis is the most commonly reported etiology, other pathogens, such as Actinomyces spp. , Staphylococcus aureus, Mycobacterium avium-intracellulare, and Aspergillus fumigatus, have also been described .

SAPHO Syndrome
SAPHO syndrome (synovitis, acne, palmoplantar pustulosis, hyperostosis, and osteitis) is a rare chronic autoimmune disease with hidradenitis suppurativa and severe acne that is sometimes associated with unusual noninfectious skeletal conditions. SAPHO syndrome occurs with equal frequency in men and women and has been reported in patients of all ages but mainly affects young and middle-aged adults. The clinical manifestations of SAPHO syndrome vary. Osteoarticular lesions cause pain and soft tissue swelling and can occur without associated skin lesions.
The most common site of the lesions is the sternocostoclavicular region, involved in 70% to 90% of patients. Imaging manifestations typically include hyperostosis and osteosclerosis with narrowing or ankylosis of the joint space ( Fig. 79.9 ). Destructive changes, including osteolytic areas and erosions, may also be noted. Less frequently, involvement of spine, sacroiliac joint, or long tubular bones may be noted. Differential diagnosis includes osteomyelitis, spondylitis, osteosarcoma, Ewing sarcoma, Paget disease, metastasis, and avascular necrosis of bone.
Synovitis, acne, pustulosis, hyperostosis, and osteitis:
- •
Unknown etiology.
- •
Hyperostosis and osteosclerosis involving sternocostoclavicular region.
- •
Spine and appendicular skeleton may also be involved.
- •
Skin lesions may be absent, precede, or follow bone lesions.
- •

Paget Disease
Paget disease (PD), or osteitis deformans, is a chronic benign metabolic bone disease of unknown etiology that affects approximately 3% to 4% of the population older than 40 years. PD exhibits a predilection for the axial skeleton, but any bone may be affected. It may affect a single bone (monostotic disease) or many bones (polyostotic forms). Monostotic PD disease is usually an incidental finding on radiographs obtained for unrelated purposes. The spine is the second most common site of involvement with PD (29%–57% of cases), after the pelvis (30%–75%). Involvement of the ribs (1%–4%), scapula, or clavicle is uncommon. Sarcomatous degeneration of PD disease of the spine or the rib into osteosarcoma has been reported.
Radiographs in PD disease are frequently sufficiently characteristic for diagnosis. It manifests as areas of enlargement of the bone with a thickened, coarsened trabecular pattern ( Fig. 79.10 ). Technetium-99m–labeled bisphosphonate tracer is more sensitive than radiography for the identification of PD lesions. The differential diagnosis of a sclerotic rib includes chronic osteomyelitis, SAPHO syndrome, Paget disease, osteochondroma, fibrous dysplasia, and sclerotic metastases.

Chest Wall Tumors
Chest wall tumors are uncommon lesions that represent approximately 5% of all thoracic malignancies. They may arise from any of the chest wall tissues—bone, cartilage, muscle, fat, fibrous connective tissue, nerves, and vessels (blood or lymphatic). It is often difficult to make an accurate presurgical diagnosis and differentiate benign from malignant tumors. Although more than 20% of lesions are visible on chest radiography, cross-sectional techniques, such as multidetector CT and MRI, are the imaging modalities of choice in the management of chest wall tumors. A combination of clinical, radiologic, and histopathologic information is often necessary to establish the correct diagnosis. In adults the most common benign chest wall tumors are lipoma and osteochondroma, and the most common malignant chest wall tumor is undifferentiated pleomorphic sarcoma (formerly malignant fibrous histiocytoma). In children the most common primary chest wall malignancies are small round-cell tumors, including peripheral neuroectodermal tumors (PNETs) and rhabdomyosarcoma.
Benign Bone Tumors
Benign bone tumors of the chest wall are uncommon lesions less frequently encountered than malignant neoplasms. They originate from blood vessels, nerves, bone, cartilage, or fat. Some of these tumors have characteristic radiographic features that allow a preoperative diagnosis. In other cases imaging plays a major role in tumor management, including staging, biopsy planning, and follow-up evaluation. Fibrous dysplasia and osteochondroma are the most common benign bone lesions of the chest wall. More unusual lesions include enchondroma, chondromyxoid fibroma, osteoid osteoma, aneurysmal bone cyst, and giant-cell tumor ( Fig. 79.11 ).

Fibrous Dysplasia
Fibrous dysplasia is a nonhereditary skeletal anomaly in which the medullary bone is replaced by fibrous tissue during the period of skeletal growth. Fibrous dysplasia is the most common primary bone tumor of the chest wall, accounting for approximately 30% of all benign chest wall osseous lesions. Virtually any bone in the body can be affected. There are two forms of the disease: monostotic (80% of cases) and polyostotic (20% of cases). Polyostotic involvement may be a part of McCune-Albright syndrome (fibrous dysplasia, patchy cutaneous pigmentation, and precocious puberty) or Mazabraud syndrome (fibrous dysplastic lesions in close proximity to soft tissue myxomas).
Monostotic fibrous dysplasia occurs most frequently in the ribs (28%), femur (23%), tibia, or craniofacial bones (10%–25%). Pathologic fractures and bone deformities are common complications.
The usual radiologic appearance of fibrous dysplasia includes an osteolytic lesion in the medullary cavity of bone, with endosteal scalloping and possible bone expansion ( Fig. 79.12 ). Periosteal reaction is typically absent. The lesion may be surrounded by a layer of thick sclerotic reactive bone (rind sign). Usually, the matrix of the lesion is smooth and relatively homogeneous; classically, this finding is described as a ground-glass appearance. Irregular areas of sclerosis may be present with or without calcification. CT and MRI enable more accurate assessment of lesion morphology, location, and extent.

Osteochondroma
Cartilage-forming tumors are the most common primary bone tumors. Osteochondroma is a cartilage-capped osseous growth that projects from the surface of the affected bone and accounts for 10% to 15% of all bone tumors. Its central core of bone marrow is continuous with the marrow of the underlying bone and is surrounded by a cortex and periosteum that are continuous with those of the affected bone. Most osteochondromas are seen in the metaphyseal regions of the long bones. Patients are commonly in the second decade of life at diagnosis.
Osteochondroma is the second most common benign rib lesion after fibrous dysplasia. Solitary osteochondromas of the chest wall are uncommon lesions. In cases of multiple familial exostoses, nearly half of patients have a costal or scapular osteochondroma, however. Osteochondromas appear on the chest radiograph as a deformity or expansion of the rib with calcification of the cartilaginous cap. CT is particularly useful in the assessment of osteochondromas in the spine, ribs, or shoulder ( Fig. 79.13 ). Unusual complications secondary to osteochondromas of the ribs include spontaneous hemothorax, empyema, extradural spinal cord compression, Horner syndrome, and malignant transformation.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree