html xmlns=”http://www.w3.org/1999/xhtml”>
Chapter 25 Child abuse and the law I: general issues for the radiologist
Introduction
Child abuse is one of those unique realms where medicine and law are strange, but routine, bed fellows. Thus, it is incumbent upon physicians involved in the detection of child abuse and neglect to have some familiarity with the law. Physicians involved in child abuse cases often encounter a variety of issues that entail legal questions – patient consent, appropriate documentation, reporting child abuse, potential liability, privilege, and confidentiality. Despite questions about the law and the need for legal understanding, doctors often greet lawyers with a sense of anxiety, if not resentment. And, with concurrent dismay, attorneys sometimes resent what they perceive as a medical lack of cooperation with the legal process. However, the test of time has borne out that the sensitive management of family violence cases requires both professional spouses to not only communicate, but to get along (1).
It is not uncommon, if not the norm now, for hospitals and communities to have multidisciplinary child abuse-assessment teams who specialize in the assessment of suspected victims of abuse (2). Common participants of multidisciplinary child abuse-assessment teams include pediatricians, radiologists, ophthalmologists, surgeons, social workers, and mental health providers. Additionally, hospitals are not the only institutions that become involved. The thorough multidisciplinary management of child abuse cases includes police departments, district attorneys’ offices, courts, and protective service agencies. Although child abuse laws are sometimes vague and poorly defined, there are three basic issues for the medical professional to consider:
Beginning with the issues of consent and record keeping, this chapter covers the principal legal requirements in the area of child abuse, with an emphasis on those materials relevant to radiologists. General information is also provided to help the radiologist understand customary practices and procedures in dealing with suspected abuse and neglect. It is important to remember, however, that the law in this area varies from state to state. For some questions of practice, it may be helpful to consult with a Child Abuse Pediatrician (CAP), or, in certain circumstances, necessary to consult with a lawyer knowledgeable about child protection.
Legal consent
The legal doctrine of informed consent is well-established in American law, and is based upon the premise that “every human being of adult years and sound mind has a right to determine what shall be done with his own body”(4). There are limitations to the doctrine of informed consent, and physicians do not have a duty to disclose every remote risk associated with a medical procedure or treatment. The ability to provide informed consent presumes mental competence of a patient. As with other scenarios where the mental competence of a patient is in question (e.g., the unconscious patient), the law assumes that a minor child lacks the legal capacity and authority to provide informed consent for medical treatment. Instead, the child’s parents or legal guardians retain and grant this authority. As such, for children, the doctrine of informed consent is more aptly interpreted as one of informed permission (5). Although children cannot usually provide legal consent for medical care or treatment, in most states, there are exceptions to this general rule:
In the emancipation process, a minor petitions a court (typically a juvenile or family court) for emancipation. Most states have minimum age requirements (typically 16 years of age) before such a petition can be made (7). The minor must prove to the court his or her age, affirm residency in the state, and declare why he or she is seeking emancipation. In considering a minor’s petition for emancipation, courts assess a multitude of factors – whether the minor is or has been married, has children, is a member of the armed forces, or is financially independent and living separate and apart from the parents. Ultimately, however, a determination of emancipation is based upon what is in “the best interest of the child” (8).
Although a minor may demonstrate characteristics of emancipation, or even declare himself or herself to be so, a physician should never assume emancipation unless provided clear court documentation affirming so. When adjudicated as “emancipated,” the minor child is legally congruent to an adult for medical care and treatment purposes. Accordingly, the emancipated minor may provide (or refuse) informed consent to medical intervention as an adult would. It is notable that pregnancy and parenthood are not typically statutory criteria for emancipation. This can occasionally lead to the legally interesting and ironic situation of a minor child being able to provide consent for her child’s care, but not for her own.
As the determination of “maturity” is case-specific, the doctrine lacks concrete principles that can be easily applied to future scenarios, and inherently has resulted in variable decisions. Some states have recognized a distinction between a minor’s ability to consent for health-promoting treatment and a minor’s ability to refuse health-or life-sustaining treatment. Additionally, recent national and international cases have highlighted the ethical complexities of these cases when minors have sought to refuse medical treatment (even life-sustaining treatment) based upon their religious beliefs (10). Finally, as with emancipation, although a minor child may exhibit characteristics of a “mature minor,” or even declare himself or herself to be so, a physician should never assume mature minor status applies unless he or she is provided clear court documentation affirming so.
In addition to these exceptions, there are other scenarios where a minor may consent for medical care or treatment:
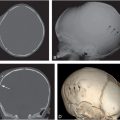
In “an emergency” (e.g., when a child with subdural hematomas is brought to the hospital by ambulance), physicians may take whatever medical steps are necessary to diagnose and treat the child, although, if time permits, staff should make every reasonable effort to contact those able to consent.
When a minor child obtains medical care and treatment for one of these state-sanctified conditions, physicians and hospitals may not bill the parents or release the child’s medical information without the written approval of the minor patient. All physicians, especially those routinely involved in the care of maltreated children, should be knowledgeable of their state-specific conditions.
Aside from the specific exceptions discussed above, the general rule is that parental informed permission is necessary prior to medical intervention on a minor child. However, the consent of only one parent or guardian is required, not both. If there is conflict or disagreement between parents or guardians, it is probably wise to consult a hospital lawyer or administrator. If a child is in the legal custody of a state protective agency or resides with foster parents, the agency or foster parents, rather than the minor’s biologic parents, will have the authority to make medical decisions, and should provide appropriate documentation demonstrating that authority. If the parent or legal guardian refuses to consent to evaluation or treatment that the physician thinks is necessary, the physician or others (e.g., state protective services) may petition a court to intervene or to compel parental compliance.
Documentation and medical records
The United States is a litigious society – some would say too litigious. This fact, and the inherent adversarial nature of child maltreatment case litigation, makes complete, accurate, and objective medical documentation a healthcare imperative. In child maltreatment cases, many different audiences may have access to medical records – patients, parents and legal guardians, child protective agencies, law enforcement, attorneys, and the courts. Take care, therefore, in deciding what is recorded and when and how reports are dictated and transcribed. The following guidelines will assist the radiologist in diminishing medico-legal risk in documentation.
Do:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree