Chapter 9
Cholangiocarcinoma
Ersan Altun1, Mohamed El-Azzazi1,2,3,4, Richard C. Semelka1, and Miguel Ramalho1,5
1The University of North Carolina at Chapel Hill, Department of Radiology, Chapel Hill, NC, USA
2University of Dammam, Department of Radiology, Dammam, Saudi Arabia
3King Fahd Hospital of the University, Department of Radiology, Khobar, Saudi Arabia
4University of Al Azhar, Department of Radiology, Cairo, Egypt
5Hospital Garcia de Orta, Department of Radiology, Almada, Portugal
- Cholangiocarcinoma is the second most common primary liver malignancy and accounts for 10–20% of primary tumors.
- More common in areas with endemic fluke infestation (O. Viverini and C. Sinensis). Hepatolithiasis developing secondary to recurrent pyogenic cholangitis is another risk factor.
- Other risk factors include congenital biliopancreatic anomalies, cirrhosis, primary sclerosing cholangitis, hepatitis B or C virus infection, and heavy alcohol consumption.
- Classified into three types:
- Mass-forming cholangiocarcinoma
- Periductal infiltrative cholangiocarcinoma
- Intraductal cholangiocarcinoma
- More common in areas with endemic fluke infestation (O. Viverini and C. Sinensis). Hepatolithiasis developing secondary to recurrent pyogenic cholangitis is another risk factor.
- Mass-forming intrahepatic cholangiocarcinoma
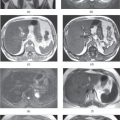
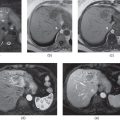
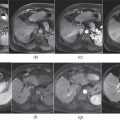
- Usually presents as a solitary intrahepatic heterogeneous mass with irregular well-defined margins. They are usually hypovascular (Figures 9.1–9.3) although hypervascular cholangiocarcinomas (Figure 9.4) may also be seen occasionally.
- May show biliary dilatation at the periphery of the lesion (Figures 9.2 and 9.5), when the tumor is more central in location.
- Vascular compression (especially portal vein) is common (Figure 14.8). Development of intravascular thrombosis is rare and is a distinguishing feature from HCC.
- Capsular retraction (Figures 9.1 and 9.3), central necrosis, and satellite nodules may be seen. Capsular retraction overlying the tumor is considered a hallmark of this tumor, but is seen only occasionally.
- Atrophy of the involved segment may be detected (Figure 9.1).
- Microscopy:
- Tumors with glandular configurations surrounded by abundant, dense fibrous stroma.
- On CT:
- Hypoattenuating mass with irregular and undulating but moderately defined margins (Figure 9.6).
- Mild to moderate irregular peripheral enhancement with gradual centripedal enhancement and pooling of contrast material on delayed images due to its abundant fibrotic stroma.
- Hypoattenuating mass with irregular and undulating but moderately defined margins (Figure 9.6).
- On MRI:
- Usually demonstrate mild to moderate high signal intensity on T2-WIs. Higher T2 signal compared to HCCs. They usually have irregular and undulating contours (Figures 9.2 and 9.3).
- Moderately low signal intensity on T1-WIs.
- Mild to moderate early irregular peripheral contrast enhancement with progressive enhancement on delayed images (Figures 9.2, 9.3, and 9.5). Note that in hypovascular tumors, the peripheral tumor border zone enhancement may simulate ring enhancement of metastases, but subtle diffuse heterogeneous enhancement may be seen on arterial phase images. Note that tumors show progressive enhancement and do not show wash-out and late capsule enhancement as seen with HCC.
- Although they are generally hypovascular, hypervascular tumors showing homogeneous or heterogeneous prominent enhancement, usually without central necrosis, on the hepatic arterial dominant phase may be seen.
- Usually demonstrate mild to moderate high signal intensity on T2-WIs. Higher T2 signal compared to HCCs. They usually have irregular and undulating contours (Figures 9.2 and 9.3).
- Differential Diagnosis
- Hepatocellular carcinoma (HCC) with sclerosis and HCC-cholangiocarcinoma may demonstrate similar imaging features to cholangiocarcinoma.
- Metastases
- Gallbladder carcinoma (Figure 9.7).
- Abscesses, hepatic tuberculosis, and inflammatory myofibroblastic tumor may mimic cholangiocarcinomas.
- Periductal infiltrating cholangiocarcinoma

Stay updated, free articles. Join our Telegram channel
- Periductal infiltrating cholangiocarcinoma

Full access? Get Clinical Tree