CHAPTER 98 Chronic Pulmonary Embolism
Pulmonary hypertension is defined as a mean arterial pressure of greater than 25 mm Hg at rest and 30 mm Hg with exercise.1 Symptoms are often nonspecific and include dyspnea on exertion and easy fatigability. When it is severe, pulmonary hypertension can be severely debilitating and even fatal. During the past decade, advances in diagnosis and therapeutics have markedly affected the mortality of pulmonary hypertension.2 What was once a lethal condition without transplantation has become a condition that may be managed with various medications.
In 2003, an international multidisciplinary conference held in Venice, Italy, revisited the classification of pulmonary hypertension with a goal of classifying pulmonary hypertension into categories based on treatment algorithms that may be beneficial.3 The result was five main categories: pulmonary arterial hypertension, pulmonary hypertension due to left-sided heart disease, pulmonary hypertension from chronic hypoxia, pulmonary hypertension due to chronic embolic disease, and pulmonary hypertension from miscellaneous causes. Of these categories, pulmonary hypertension due to chronic embolic disease is the only one that may benefit from pulmonary thromboendarterectomy and one of the only forms of pulmonary hypertension that may be cured.4 The goal of this chapter is to highlight the imaging findings of chronic pulmonary embolism and to help delineate those patients who may benefit from surgical intervention.
CHRONIC PULMONARY EMBOLISM
Definition
Chronic pulmonary embolism is more accurately referred to as chronic thromboembolic pulmonary hypertension (CTPH) to distinguish it from chronic emboli from foreign materials, such as talc, or parasitic ova, such as schistosomiasis.3 CTPH represents cytokine-mediated scarring of the pulmonary circulation from even one episode of acute pulmonary embolism.5,6 The net effect of the scarring is decreased luminal volume for the pulmonary circulation. This decrease in arterial volume results in increased pulmonary pressures.
Prevalence and Epidemiology
In the age of cross-sectional imaging, CTPH may be more common than previously thought. Prior reports suggested that less than 0.1% of patients with an episode of acute pulmonary embolism will go on to develop CTPH and pulmonary hypertension.7 More recent studies suggest that this number is an underestimation of the true incidence and prevalence. In one prospective follow-up study of 78 patients with acute pulmonary embolism, 4 patients (5%) went on to develop definite CTPH, and in another of 223 patients with acute pulmonary embolism, 3.8% went on to develop symptomatic CTPH at 2 years.8,9 Estimations of true incidence are hindered by the large number of patients with CTPH who may not have had any history or memory of symptomatic pulmonary embolism in the past. As many as two of three patients with CTPH may not have had a documented history of acute pulmonary embolism.6
Etiology and Pathophysiology
CTPH is a cytokine-mediated condition that may follow even one episode of acute pulmonary embolism. This is important to consider so that it is not confused with recurrent acute pulmonary embolism, which represents either failure of anticoagulation or a manifestation of a hypercoagulable state.6 CTPH also does not represent failure of an acute pulmonary embolism from resolution. Instead, CTPH represents the end of a cycle of in situ thrombus, scarring, and vascular remodeling that occurs after a vascular insult, usually acute pulmonary embolism.5
Manifestations of Disease
Clinical Presentation
Like other causes of pulmonary hypertension, CTPH usually is manifested with vague symptoms and nonspecific findings.10,11 Patients tend to notice decrease in exercise tolerance, easy fatigability, and dyspnea on exertion. As the condition progresses, they may find that they develop dyspnea at rest. The mean time from onset of symptoms to diagnosis is about 3 years, highlighting the insidious, nonspecific nature of this process.6,10
Imaging Indications and Algorithm
Imaging of a patient with suspected pulmonary hypertension from CTPH is aimed at answering four main questions: (1) What is the degree of pulmonary hypertension? (2) What is the etiology of the pulmonary hypertension—is chronic pulmonary embolism the cause or is another entity more likely? (3) Are changes of chronic pulmonary embolism surgically accessible? (4) Are any new pulmonary emboli present? Imaging usually begins with a chest radiograph, which might suggest pulmonary hypertension, and quickly moves to an echocardiogram, which is used to estimate pulmonary pressures and to assess cardiac function.12 Traditionally, ventilation-perfusion scintigraphy (V/Q scan) has been used to assess for CTPH in combination with CT to exclude interstitial lung disease.6,12,13 At many institutions, however, the pulmonary embolism protocol CT has replaced both studies.14 This single study, especially when it is performed on a multidetector row CT (MDCT) scanner, allows the simultaneous assessment for CTPH and interstitial lung disease.
MR may allow a noninvasive assessment of pulmonary pressures, but its routine use for exclusion of CTPH remains somewhat experimental.15 If pulmonary hypertension is confirmed on any of the modalities, patients tend to be referred for right-sided heart catheterization so that accurate measurements of pulmonary pressures and right-sided heart hemodynamics may be performed. If CTPH is uncovered, patients may go on to pulmonary angiography to assess whether pulmonary thromboendarterectomy may be beneficial. Multiplanar postprocessing of MDCT data and thin maximum intensity projections (usually 4 to 7 mm) may provide equivalent information and avoid angiography altogether.
Imaging Techniques and Findings
Radiography
Conventional radiography may show enlargement of the right side of the heart, with increased convexity of the right border of the heart on the frontal projection and filling in of the retrosternal clear space on the lateral projection (Figs. 98-1 and 98-2). The pulmonary arteries may be enlarged. Features unique to CTPH are rarely observed.
Ultrasonography
Echocardiography will show increase in the size of the right atrium and the right ventricle as well as the main pulmonary artery. Echocardiography may be used to estimate pulmonary pressures.16 This estimate is based on calculating the peak velocity of the tricuspid regurgitation jet and calculating a pressure based on a modified Bernoulli equation [pressure = 4 × velocity2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



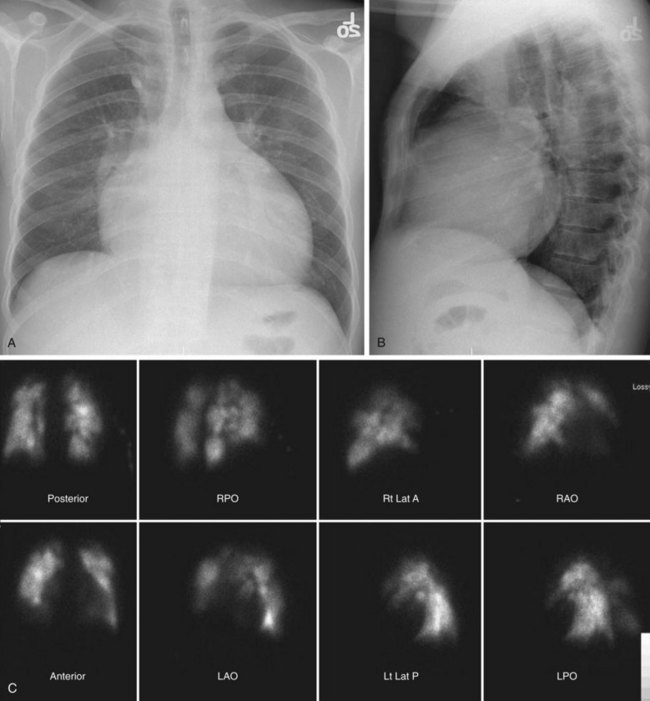
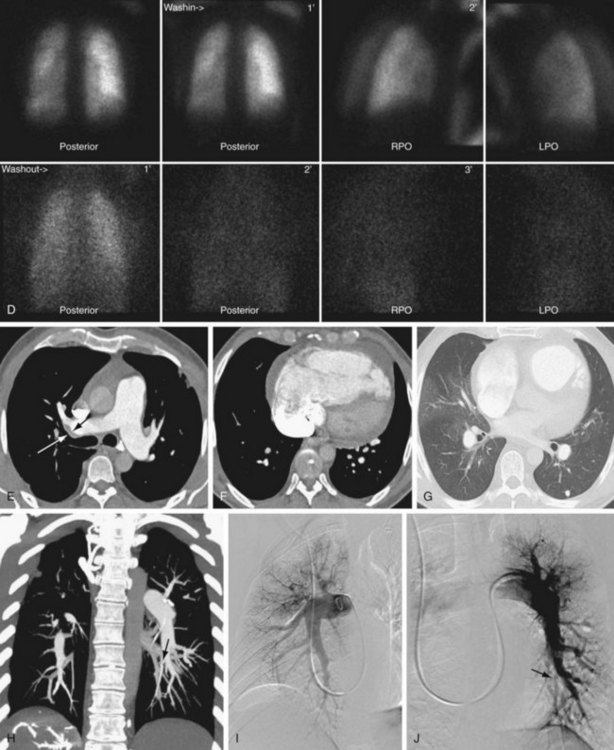
 FIGURE 98-1
FIGURE 98-1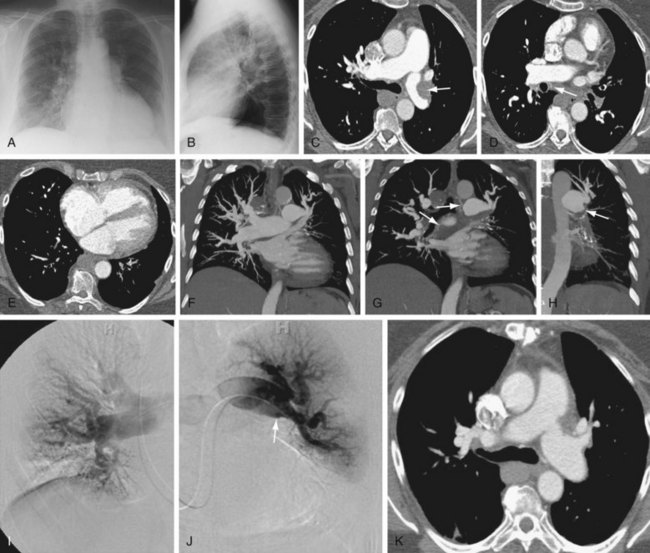
 FIGURE 98-2
FIGURE 98-2