Presentation and Presenting Images
A 39-year-old female presents for baseline high-risk screening mammography.
46.2 Key Images
46.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
46.2.2 Imaging Findings
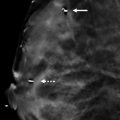
In the posterior depth of the left breast at the 2 o’clock location, there is an oval circumscribed mass. This is demonstrated on both conventional mammography ( ▶ Fig. 46.1 and ▶ Fig. 46.2) and tomosynthesis ( ▶ Fig. 46.3 and ▶ Fig. 46.4). The location would be classic for a lymph node; however, no defining features are seen to identify this as a lymph node.
46.3 BI-RADS Classification and Action
Category 0: Mammography: Incomplete. Need additional imaging evaluation and/or prior mammograms for comparison.
46.4 Diagnostic Images
( ▶ Fig. 46.5, ▶ Fig. 46.6, ▶ Fig. 46.7, ▶ Fig. 46.8)
46.4.1 Imaging Findings
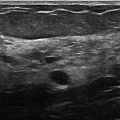
The diagnostic imaging demonstrates the oval circumscribed mass to be at the 2 o’clock location in the posterior depth ( ▶ Fig. 46.5, ▶ Fig. 46.6, and ▶ Fig. 46.7). However, these images do not provide any additional information about the nature of the mass. An ultrasound was performed that confirms a 0.9 × 0.5 × 1.0 cm oval hypoechoic mass with a central echogenic hilum located 9 cm from the nipple ( ▶ Fig. 46.8). Normal vascularity was seen in the hilum.
46.5 BI-RADS Classification and Action
Category 2: Benign
46.6 Differential Diagnosis
Lymph node: The location of this mass suggests that a lymph node is a likely diagnosis. However, it does not have the classic features of a fatty hilum on conventional mammography or tomosynthesis. The patient also has no prior imaging for comparison. Additional imaging is warranted. In this case, ultrasound, which demonstrated the mass to be a lymph node, was the most helpful.
Fibroadenoma: Fibroadenomas can occur anywhere in the breast and are very common in patients this age. Additional imaging is warranted. The ultrasound in this case does not support this diagnosis.
Breast cancer: Triple-negative cancers have a predilection to occur in the posterior region of the breast and also have a benign appearance. Because the mass is not classic for any specific lesion, additional evaluation is required.
46.7 Essential Facts
DBT has shown promise in better characterizing benign findings and thus avoiding unnecessary recall mammography.
Some benign-appearing lesions will only be seen on DBT.
Recall rates are higher for those with no prior imaging studies than those with prior imaging studies.
FFDM plus DBT has demonstrated a significant reduction in recall rates in women with a baseline mammogram compared to FFDM alone. There was no associated reduction in sensitivity with the decrease in recall rates.
46.8 Management and Digital Breast Tomosynthesis Principles
There is a learning curve for reading DBT images before the reader is comfortable and confident.
Early in the implementation of DBT, there is often a slight increase in recalls owing to readers’ readjustment of sensitivity and specificity in reading images from a new modality.
Although DBT offers the ability to better define lesions and identify them as benign. Care should be taken to ensure that the imaging findings meet all the criteria to dismiss them as benign.
46.9 Further Reading
[1] Roth RG, Maidment AD, Weinstein SP, Roth SO, Conant EF. Digital breast tomosynthesis: lessons learned from early clinical implementation. Radiographics. 2014; 34(4): E89‐E102 PubMed
[2] Sumkin JH, Ganott MA, Chough DM, et al. Recall Rate Reduction with Tomosynthesis During Baseline Screening Examinations: An Assessment From a Prospective Trial. Acad Radiol. 2015; 22(12): 1477‐1482 PubMed

Fig. 46.1 Left craniocaudal (LCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree