Chapter 2 Clinical assessment and recording
The process of birth is a hazardous journey for any individual. The complete journey is from conception until discharge from hospital of the healthy mother and baby. The continuum of fetal health involves antenatal wellbeing and neonatal wellbeing. This is the modern concept of perinatology. As few, if any, obstetricians are also neonatologists a clearer concept is maternofetal medicine. Although we are not neonatologists, we must maintain an interest in our in-utero patient during his or her stay in the neonatal unit, just as the neonatologist will have joined us in assessment and counselling of the high-risk mother antenatally.
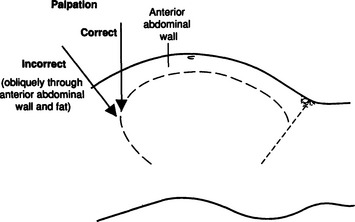
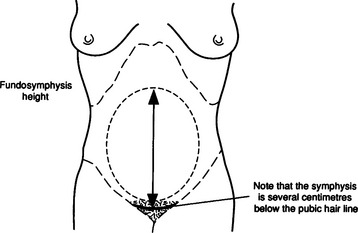
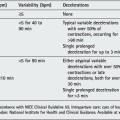
On admission to the labour ward the history is summarized taking particular note of high-risk factors such as previous perinatal loss, previous or existing intrauterine growth restriction, bleeding in pregnancy, diabetes mellitus, reduced fetal movements and a variety of other markers. Breech presentation and multiple pregnancies are obvious high-risk factors. On examination general features such as height, weight, blood pressure, temperature and signs of anaemia are reviewed. Before proceeding to vaginal examination, abdominal examination must be complete. This includes a measurement of abdominal size, an estimate of fetal size, lie, presentation and station of the presenting part. The nature of the contractions, amniotic fluid volume estimation and auscultation of the fetal heart complete this procedure. Traditionally the size of the abdomen and fetus is assessed subjectively. The value of formalizing this with an objective value has been suggested in recent years.6 A measure of the fundosymphysis height (FSH) in centimetres (Figs 2.1 and 2.2) provides a reliable guide to fetal size so long as the observers have been trained in the technique.7, 8 The fundus should not be actively pushed down during the palpation, and the height from the top of the fundus (without correcting the uterus to the midline) to the upper margin of the symphysis pubis should be measured. Ideally a blinded measurement using the blank side of a tape measure is desirable. Due attention should be paid to the possible confounding factors of obesity, polyhydramnios, fibroids or unusual physical characteristics of the mother. After 20 weeks’ gestation the FSH should be equivalent to the gestational age in centimetres ±2 cm up to 36 weeks, and ±3 cm after 36 weeks. No test should be subjected to unrealistic expectations. A tape measure is cheap, available and reasonably reliable with little inter- or intraobserver variation.9 We are not good at identifying small babies in utero; this is obvious from studies of adverse perinatal outcome. The reduced fundosymphysis height may indicate a small fetus who may be suffering from chronic asphyxia (intrauterine growth restriction; see (Ch. 6). Such a fetus is more likely to develop an abnormal heart rate pattern before, and particularly in, labour. A suspicion of a large fetus is also important so that we can anticipate and prepare for mechanical problems. A history of big babies, shoulder dystocia and diabetes mellitus are all important indicators. A rewarding exercise is recording the estimated fetal weight on the partogram. With experience and regular practice this becomes reliable. Management may be altered if abnormal labour progress becomes manifest and there is a likelihood of cephalopelvic disproportion. Marking ‘Beware shoulder dystocia’ in the ‘special features’ box on the partogram of women carrying large babies, and especially with a history of shoulder dystocia, is an important preventative measure. Medical help will be organized to be readily available in the second stage of labour.
Abdominal examination is performed before vaginal examination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree