1. Clinical Perspective
Proximal humerus fractures represent a common fall-related condition that occurs primarily in older osteoporotic individuals. Although already common, their incidence is predicted to triple over the next three decades, because of the increasing aging of the population.6,7 Less commonly, proximal humerus fractures may occur in younger active individuals after traumatic shoulder dislocation, or result from violent muscle contraction during a seizure or following an electric shock.
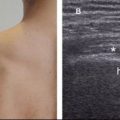
Clinical findings are nonspecific and include pain, immobility, paresthesia, and/or weakness of the affected limb. Hence, imaging is usually required for correct diagnosis and adequate treatment planning. Radiographs are usually considered the first-line of imaging evaluation in trauma setting, but accurate radiographic technique is necessary because many fractures may be missed if only anteroposterior (AP) views are obtained (trauma series should include AP and axillary or lateral views). US, MRI, and CT are adequate alternatives if radiographs fail to demonstrate the cause of symptoms or do not sufficiently delineate the fracture for management purposes. CT is currently considered the gold standard to diagnose proximal humerus fractures, but has limitations to detect adjacent soft tissue disorders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree