CHAPTER 24 Clinical Techniques of Positron Emission Tomography and PET/CT
RADIOPHARMACEUTICALS
Although several tracers have been used for evaluating myocardial perfusion with PET, the most widely used in clinical practice are rubidium 82 and ammonia N 13. In addition, 18FDG is the radiotracer of choice for the evaluation of myocardial viability.1
Rubidium 82
After infusion, rubidium 82 rapidly crosses the capillary membrane and is actively transported to the cell via the sodium/potassium ATP transporter, which depends on coronary blood flow.2 Compared with fluorine 18 or nitrogen 13, the positron range and the spatial uncertainty in the location of the decaying nucleus of rubidium 82 (2.6 mm FWHM [full width at half maximum]) is greater than for fluorine 18 (0.2 mm FWHM) or nitrogen 13 (0.7 mm FWHM), mitigating the improved spatial resolution of PET.
Ammonia N 13
Being a cyclotron product, ammonia N 13 use in routine clinical practice is limited to institutions that have a cyclotron on site. It has a physical half-life of 9.96 minutes and has a shorter positron range compared with rubidium 82, resulting in higher signal-to-noise ratio. After injection, ammonia N 13 rapidly disappears from the circulation, permitting the acquisition of images of excellent quality. Although the sequestration of ammonia N 13 in the lungs is usually minimal, it may be increased in patients with depressed left ventricular systolic function or chronic pulmonary disease and, occasionally, in smokers; this may adversely affect the quality of the images. In these cases, it may be necessary to increase the time between injection and image acquisition to optimize the contrast between myocardial and background activity. When inside the myocyte, ammonia N 13 is incorporated into the glutamine pool and becomes metabolically trapped. Only a small fraction diffuses back into the intravascular space.3
Myocardial retention of ammonia N 13 is heterogeneous, with retention in the lateral left ventricular wall being about 10% lower than that of other segments, even in normal subjects. This heterogeneous retention could result in an apparent perfusion defect in the inferolateral wall, limiting its evaluation. Ammonia N 13 allows the acquisition of ungated and gated images of excellent quality. These studies take full advantage of the superior resolution of PET relative to single photon emission computed tomography (SPECT) because the half-life of ammonia N 13 is sufficiently long, and its average positron range is very short. Gated ammonia N 13 imaging can provide accurate assessments of regional and global cardiac function.4 This imaging agent is not well suited for peak stress gated imaging, however, because of the 3- to 4-minute time interval between radiotracer injection and start of imaging, and the relatively long (20 minutes) acquisition time.
ASSESSMENT OF MYOCARDIAL PERFUSION
Imaging Protocols
Figure 24-1 illustrates common protocols used for imaging myocardial perfusion with PET/CT, where the low-dose CT scan is used for attenuation correction.1 This scan is also called a CT-based attenuation correction scan (CTAC).
Emission Scans
Different protocols can be used to acquire emission scans (see Fig. 24-1), as follows:
Stress testing is most commonly performed using adenosine, dipyridamole, or dobutamine. Protocols using exercise stress testing with PET/CT have been described.5 The use of exercise PET in clinical practice is very limited, however, especially with shorter half-life agents such as rubidium 82 (half-life 76 seconds).
Quality Assurance for Cardiac PET/CT
Diagnostic Accuracy
Table 24-1 summarizes the published studies documenting the diagnostic accuracy of myocardial perfusion PET imaging for detecting obstructive CAD.7 The average weighted sensitivity for detecting at least one coronary artery with greater than 50% stenosis is 90% (range 83% to 100%), and the average specificity is 89% (range 73% to 100%). The corresponding average positive and negative predictive values are 94% (range 80% to 100%) and 73% (range 36% to 100%), and the overall diagnostic accuracy is 90% (range 84% to 98%). Most of the available data have been obtained with dedicated PET cameras, rather than with PET/CT systems. In a more recent study using PET/CT (where the CT was used only for attenuation correction), Sampson and colleagues8 reported a sensitivity of 93%, a specificity of 83%, and a normalcy rate of 100%. In this study of patients without known prior CAD, the positive and negative predictive values of PET/CT were 80% and 94%, with an overall accuracy of 87%. All patients with a low likelihood for CAD showed normal scans, for a normalcy rate of 100%. The sensitivity for detecting CAD in patients with single vessel and multivessel (two or more vessels) disease was 92% and 95%. These results were applicable to men and women and to obese and nonobese individuals.
Comparative Studies of Positron Emission Tomography versus Single Photon Emission Computed Tomography
Two studies have performed a direct comparison of the diagnostic accuracy of rubidium 82 myocardial perfusion PET and thallium 201 imaging in the same patient populations. Go and colleagues9 compared PET and SPECT in 202 patients and showed higher sensitivity with PET than with SPECT (93% vs. 76%), without significant changes in specificity (78% vs. 80%). Stewart and coworkers10 compared PET and SPECT in 81 patients and observed a higher specificity with PET than with SPECT (83% vs. 53%), without significant differences in sensitivity (86% vs. 84%). The differences between these two studies are likely to be attributable to patient selection resulting in differences in prescan likelihood of CAD.
More recently, Bateman and associates11 compared rubidium 82 PET and Tc 99m sestamibi SPECT in two matched patient cohorts undergoing clinically indicated pharmacologic stress perfusion imaging using contemporary technology for SPECT and PET. Overall diagnostic accuracy was higher for PET than for SPECT (87% vs. 71% with a 50% angiographic threshold, and 89% vs. 79% with a 70% angiographic threshold). Differences in diagnostic accuracy reflected primarily the increased specificity (with a marginal advantage in sensitivity) of PET versus SPECT, and applied to men and women and to obese and nonobese individuals.
Evaluation of Multivessel Coronary Artery Disease
The diagnosis of multivessel or left main CAD with diffuse balanced ischemia using MPI remains a challenge. PET (similar to SPECT) often uncovers only the coronary territory supplied by the most severe stenosis. The use of ancillary high-risk markers often helps in ascertaining the presence of multivessel CAD. ECG gating provides a unique opportunity to assess left ventricular function at rest and during peak stress (as opposed to poststress with gated SPECT). More recent data suggest that in normal subjects, LVEF increases during peak vasodilator stress.12 In the presence of CAD, changes in LVEF (from baseline to peak stress) are inversely related to the magnitude of perfusion abnormalities during stress (reflecting myocardium at risk) (Fig. 24-3) and the extent of angiographic CAD (Fig. 24-4). In patients with three-vessel or left main CAD, LVEF during peak stress decreases even in the absence of apparent perfusion abnormalities (Fig. 24-5). In contrast, patients without significant CAD or with one-vessel disease show a normal increase in LVEF. Consequently, the negative predictive value of an increase in LVEF (from rest to peak stress) of 5% or greater to exclude the presence of three-vessel or left main CAD or both is 97%.12
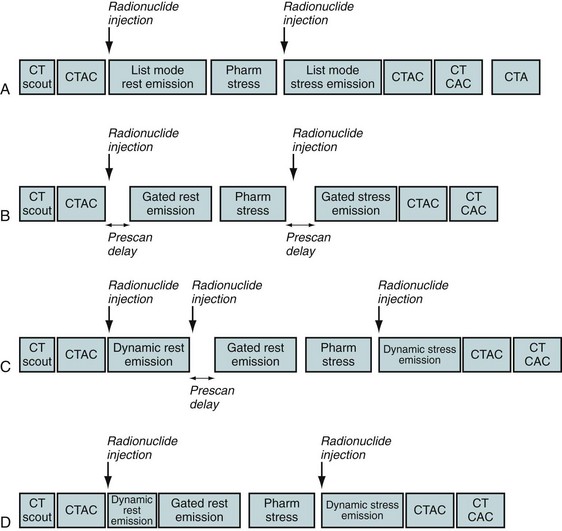
 FIGURE 24-1
FIGURE 24-1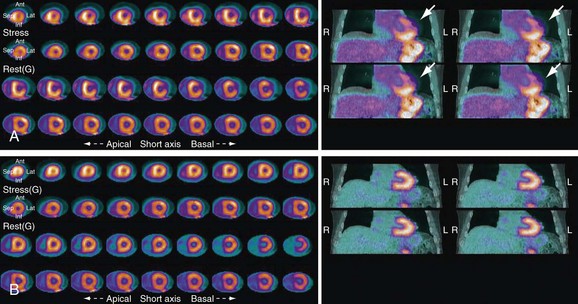
 FIGURE 24-2
FIGURE 24-2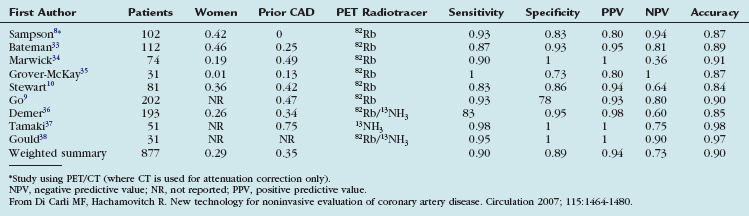
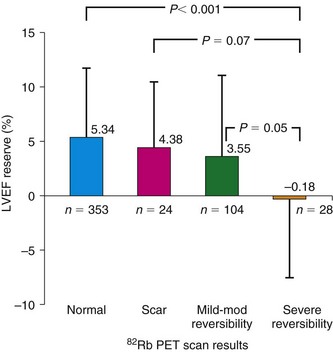
 FIGURE 24-3
FIGURE 24-3
 FIGURE 24-4
FIGURE 24-4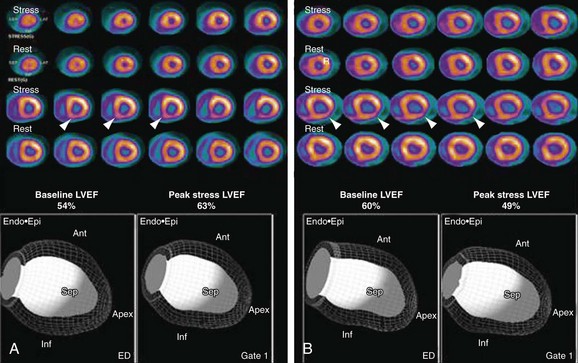
 FIGURE 24-5
FIGURE 24-5


