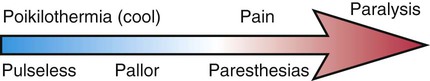
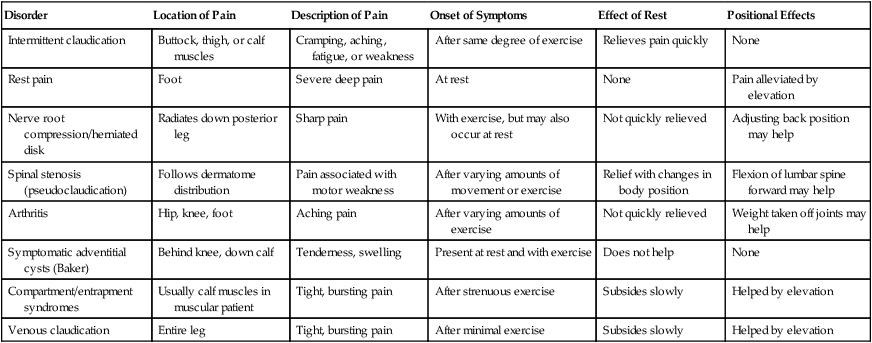
Benjamin S. Brooke and James H. Black, III The natural history of arteriosclerosis in the lower extremity can be viewed as a progression of symptoms that reflect the degree of vessel occlusion and presence of collateral circulation. Symptoms classically begin with an intermittent and reproducible pain termed claudication, a derivation of the Latin word for “limp.” Intermittent claudication is characteristically brought on by a given degree of exercise and relieved after a few minutes of rest. These symptoms reflect a demand for blood flow increases that cannot be met because of atherosclerotic narrowing in one or more arterial segments. Compression of stenotic arteries by exercising muscle and lack of compensatory vasodilation in diseased segments may also contribute to limited extremity perfusion. This pain is often described as aching, cramping, weakness, or fatigue and may present in the buttocks, thighs, calves, or feet. This diagnosis must be considered with any exertional limitation of the lower extremity muscles or any history of walking impairment that gets better shortly after rest. However, there are a number of other causes of extremity pain that must be considered and excluded from the diagnosis (Table 15-1). Among patients with claudication, 25% will experience worsening symptoms, 5% will eventually require revascularization, and only 1% to 2% will come to major amputation.1 TABLE 15-1 Differential Diagnosis of Extremity Pain Adapted from Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD). TASC Working Group. TransAtlantic Inter-Society Consensus (TASC). J Vasc Surg 2000;31(Suppl):S1–S296. A query of the specific distribution of claudication reported by the patient is an important focus of the history. Symptoms typically occur in the muscle groups immediately distal to the region of stenosis. The exact site(s) of discomfort or pain should be recorded, along with the relationship of this pain to rest or degree of exertion. Narrowing of the aortoiliac vessels classically presents as the constellation of buttock pain, impotence, and lower extremity muscle atrophy known as Leriche syndrome. Similarly, occlusion of the femoral, popliteal, or proximal tibial arteries will present as exertional calf pain. Multiple studies have found intermittent claudication to be a reliable symptom in the diagnosis of peripheral arterial disease. A recent meta-analysis found that the presence of claudication increased the likelihood of arterial disease being present by over threefold, whereas its absence lowers the likelihood by half that moderate to severe disease is present.2 The clinical presentation of acute arterial insufficiency and limb ischemia is characterized by new-onset extremity pain with concurrent changes in neurologic function. Pain is usually the first symptom to be described and is characteristically elicited by passive flexion or stretch of the extremity. This pain is not usually localized exclusively to the distal foot and not affected by limb position, which helps differentiate it from the rest pain of chronic arterial insufficiency. Sensory loss is the earliest neurologic sign; it may be very subtle at first but progresses quickly to frank paresthesias. When extremity perfusion continues to be compromised, muscle strength and motor control become diminished. This spectrum of clinical symptoms and findings are termed the 6 Ps: pain, pallor, poikilothermia, paresthesias, paralysis, and pulselessness (Fig. 15-1). The majority of abdominal aortic aneurysms (AAAs) remain asymptomatic until they dissect or rupture. As such, a ruptured AAA is the 13th leading cause of death in the United States.3
Clinical Vascular Examination
History
Chronic Arterial Insufficiency
Disorder
Location of Pain
Description of Pain
Onset of Symptoms
Effect of Rest
Positional Effects
Intermittent claudication
Buttock, thigh, or calf muscles
Cramping, aching, fatigue, or weakness
After same degree of exercise
Relieves pain quickly
None
Rest pain
Foot
Severe deep pain
At rest
None
Pain alleviated by elevation
Nerve root compression/herniated disk
Radiates down posterior leg
Sharp pain
With exercise, but may also occur at rest
Not quickly relieved
Adjusting back position may help
Spinal stenosis (pseudoclaudication)
Follows dermatome distribution
Pain associated with motor weakness
After varying amounts of movement or exercise
Relief with changes in body position
Flexion of lumbar spine forward may help
Arthritis
Hip, knee, foot
Aching pain
After varying amounts of exercise
Not quickly relieved
Weight taken off joints may help
Symptomatic adventitial cysts (Baker)
Behind knee, down calf
Tenderness, swelling
Present at rest and with exercise
Does not help
None
Compartment/entrapment syndromes
Usually calf muscles in muscular patient
Tight, bursting pain
After strenuous exercise
Subsides slowly
Helped by elevation
Venous claudication
Entire leg
Tight, bursting pain
After minimal exercise
Subsides slowly
Helped by elevation
Acute Arterial Insufficiency
Abdominal Aortic and Mesenteric Disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Clinical Vascular Examination