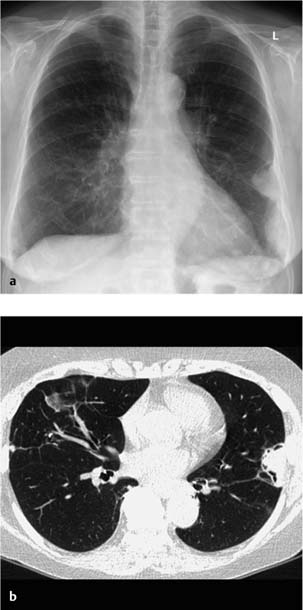
6 Collagen Diseases and Vasculitis Generalized inflammatory joint disorder of uncertain etiology. Most common collagen vascular disease Etiology is unclear CT. Low sensitivity Pathologic findings are visualized in about 30% of cases. – Pleural findings (most common): Include slight pleural effusion – Parenchymal findings (predominantly basal and subpleural): Include finely to coarsely reticular and nodular opacities with honeycombing, similar to idiopathic pulmonary fibrosis or nonspecific interstitial pneumonitis – Airway findings: Include bronchiolitis Coarsely reticular and nodular interstitial changes in combination with joint symptoms. Presentation is variable; patients may be asymptomatic Anti-inflammatory treatment of the underlying disorder (anti-inflammatory agents, steroids, TNF-α blockers, immunosuppressives). Fig. 6.1 Plain chest radiograph of a 70-year-old man with a long history of rheumatoid arthritis. Relatively nonspecific bilateral basal finely reticular streaky shadowing consistent with pulmonary interstitial changes. Depend on the underlying disorder. Characterize and ascertain the extent of findings.
Rheumatoid Arthritis
Definition
 Epidemiology
Epidemiology
 Extraarticular manifestations are rare
Extraarticular manifestations are rare  More common in men than women
More common in men than women  Rarely occurs before joint symptoms
Rarely occurs before joint symptoms  Occurs in middle age.
Occurs in middle age.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 Pleuropulmonary manifestations include pleural involvement and, less pronounced, fibrosing alveolitis, rheumatoid nodules, airway changes (bronchitis, bronchiolitis, bronchiectasis).
Pleuropulmonary manifestations include pleural involvement and, less pronounced, fibrosing alveolitis, rheumatoid nodules, airway changes (bronchitis, bronchiolitis, bronchiectasis).
Imaging Signs
 Modality of choice
Modality of choice
 Radiographic findings
Radiographic findings
 Severe cases show predominantly basal reticulonodular shadowing and linear, nonseptal opacities
Severe cases show predominantly basal reticulonodular shadowing and linear, nonseptal opacities  Honeycombing
Honeycombing  Pleuritis (pleural effusion
Pleuritis (pleural effusion  Rheumatoid nodules (< 5% of cases).
Rheumatoid nodules (< 5% of cases).
 CT findings
CT findings
 Pleural thickening.
Pleural thickening.
 Ground-glass opacities
Ground-glass opacities  Rheumatoid nodules (solitary or multiple, peripheral, sharply demarcated, 50% showing cavitation, rarely calcified).
Rheumatoid nodules (solitary or multiple, peripheral, sharply demarcated, 50% showing cavitation, rarely calcified).
 Bronchiectasis.
Bronchiectasis.
 Pathognomonic findings
Pathognomonic findings
Clinical Aspects
 Typical presentation
Typical presentation
 Dyspnea with nonproductive
Dyspnea with nonproductive  Pleuritis
Pleuritis  Lung function is restricted with impaired diffusion capacity and reduced vital capacity
Lung function is restricted with impaired diffusion capacity and reduced vital capacity  Positive rheumatoid factor in 80% of cases
Positive rheumatoid factor in 80% of cases  Pleural exudate is high in protein and low in glucose with a high level of lactate dehydrogenase and low pH and contains lymphocytic, neutrophilic, and eosinophilic cells.
Pleural exudate is high in protein and low in glucose with a high level of lactate dehydrogenase and low pH and contains lymphocytic, neutrophilic, and eosinophilic cells.
 Therapeutic options
Therapeutic options
 Course and prognosis
Course and prognosis
 What does the clinician want to know?
What does the clinician want to know?
Differential Diagnosis
Idiopathic pulmonary fibrosis | – Ambiguous radiographic morphology – No pleural changes – No rheumatoid nodules – No joint pathology |
Scleroderma | – Ambiguous radiographic morphology – Esophageal dilation – No joint pathology |
Asbestosis | – Ambiguous radiographic morphology – Pleural plaques – History of occupational exposure |
Tips and Pitfalls
In the presence of a known underlying disorder, the diagnosis is straightforward  However, the findings themselves are nonspecific
However, the findings themselves are nonspecific  Focal lesions require histologic evaluation.
Focal lesions require histologic evaluation.
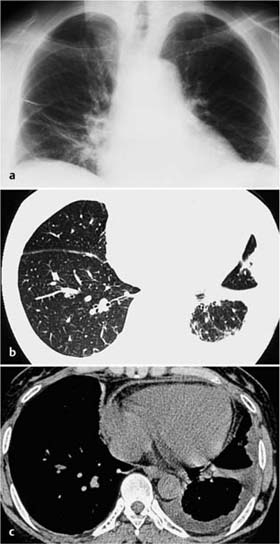
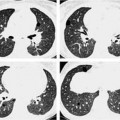
Fig. 6.2 Rheumatoid nodules in a 70-year-old woman.
a The plain chest radiograph shows bilateral focal lesions, the largest of which occur in the left laterobasal pleural region.
b Findings on CT include isolated eccentric cavities and bronchiectatic changes.
Selected References
Biederer J et al. Correlation between HRCT findings, pulmonary function tests and bronchoalveolar lavage cytology in interstitial lung disease associated with rheumatoid arthritis. Eur Radiol 2004; 14: 272–280
Remy-Jardin M et al. Lung changes in rheumatoid arthritis: CT findings. Radiology 1994; 193: 375–382
Systemic Lupus Erythematosus
Definition
 Epidemiology
Epidemiology
Systemic autoimmune disorder, a member of the group of collagen diseases.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Antinuclear antibodies are present in 95% of cases  Genetic disposition
Genetic disposition  90% of patients are women
90% of patients are women  Pleuropulmonary involvement in about 50% of cases, usually in the form of pleural effusions, less often as acute lupus pneumonitis with damage to the alveolar-capillary membrane and alveolar hemorrhages
Pleuropulmonary involvement in about 50% of cases, usually in the form of pleural effusions, less often as acute lupus pneumonitis with damage to the alveolar-capillary membrane and alveolar hemorrhages  Pulmonary fibrosis rarely develops.
Pulmonary fibrosis rarely develops.
Imaging Signs
 Modality of choice
Modality of choice
CT is preferable to plain radiography.
 Radiographic and CT findings
Radiographic and CT findings
Pleuritis or pleural effusion in 70% of cases, pericardial effusion in 35% (usually slight and bilateral)  Lupus pneumonitis in 5% with nodular consolidations, ground-glass opacities, alveolar hemorrhages, predominantly basal
Lupus pneumonitis in 5% with nodular consolidations, ground-glass opacities, alveolar hemorrhages, predominantly basal  “Shrinking lung” syndrome: increasing volume loss without significant parenchymal changes (from diaphragmatic dysfunction or pleuritis)
“Shrinking lung” syndrome: increasing volume loss without significant parenchymal changes (from diaphragmatic dysfunction or pleuritis)  Fibrosis, thickening of the bronchial wall, or bronchiectasis are rare
Fibrosis, thickening of the bronchial wall, or bronchiectasis are rare  Note: Pneumonia is common in immunosuppression (whether pathologic or drug-induced).
Note: Pneumonia is common in immunosuppression (whether pathologic or drug-induced).
 Pathognomonic findings
Pathognomonic findings
There are no pathognomonic findings. Pleural and pulmonary changes tend to be nonspecific.
Clinical Aspects
 Typical presentation
Typical presentation
Presence of at least four of the following symptoms is diagnostic: butterfly erythema, discoid lupus, photosensitivity, oral ulcerations, arthritis, serositis, renal involvement, CNS involvement, antinuclear antibodies  With pulmonary involvement, symptoms include fever, dyspnea, cough, chest pain, and hemoptysis.
With pulmonary involvement, symptoms include fever, dyspnea, cough, chest pain, and hemoptysis.
 Therapeutic options
Therapeutic options
Immunosuppressives.
 Course and prognosis
Course and prognosis
Depend on the organs involved.
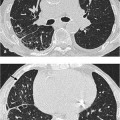
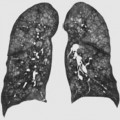
Fig. 6.3
a Pleuritis with systemic lupus erythematosus. The plain chest radiograph of a patient with reduced depth of inspiration shows a left pleural effusion with strips of dystelectasis on the right.
b, c The CT scans show pericardial involvement in addition to the pleural effusion but no interstitial or parenchymal changes.
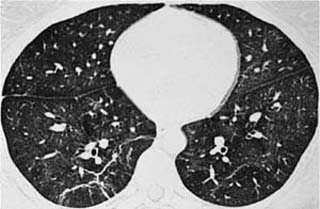
Fig. 6.4 CT in systemic lupus erythematosus showing discrete inter-stitial changes resembling ground-glass opacity.
Differential Diagnosis
Other collagen diseases | – Clinical findings are crucial to the diagnosis – Morphologic findings on the radiograph are usually ambiguous |
Idiopathic interstitial pneumonia | – Pulmonary changes are most important and are crucial to the diagnosis |
Pneumonia | – In systemic lupus erythematosus there is usually other pulmonary pathology with pleural involvement, pulmonary hemorrhage, and interstitial changes |
Tips and Pitfalls
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree