SONOGRAM ABBREVIATIONS
ACH Achilles tendon
ATFL Anterior talofibular ligament
ATT Anterior tibialis tendon
EDL Extensor digitorum longus tendon
EHL Extensor hallucis longus tendon
FDL Flexor digitorum longus tendon
FHL Flexor hallucis longus tendon
PB Peroneus brevis tendon
PF Plantar fascia
PL Peroneus longus tendon
PTT Posterior tibialis tendon
SOL Soleus muscle
KEY WORDS
Anisotropy. The echogenicity of a tendon may depend on the orientation of the ultrasound beam relative to the tendon structure. This causes an angle-dependent artifact known as anisotropy. If the tendon is perpendicular to the central axis of the sound beam, then the tendon will appear echogenic, and the fibers of the tendon will be well visualized. However, if the tendon is not perpendicular but is oblique to the central axis of the sound beam, the tendon will appear more hypoechoic, and the fibers will be suboptimally visualized.
Ankle Mortise. Ankle mortise is formed by the lower end of the tibia and its malleolus and the malleolus of the fibula, which together form a mortise for the reception of the upper surface of the talus.
Bursitis. Inflammation of a bursa, a fibrous sac around certain tendons and bones. Bursae have a synovial-lined membrane and secrete synovial fluid.
Plantar. Relating to the sole of the foot.
Perimysium. The sheath of connective tissue enveloping bundles of muscle fibers.
Tenosynovitis. An inflammation of the tendon sheath, sometimes manifested as fluid within the synovial sheath.
Tendonitis. Inflammatory condition of a tendon, often from a strain or repetitive injury.
Tendinopathy. A tendon abnormality resulting from ischemic or degenerative processes rather than inflammation. Most cases of tendonitis would more appropriately be termed “tendinopathy” because pathologically there are no inflammatory cells present, but the word “tendonitis” is still used extensively.
Valgus Test. A clinical maneuver used to apply direct stress to the medial aspect of the joint to test medial instability.
Varus Test. A clinical maneuver used to apply direct stress to the lateral aspect of the joint to test lateral instability.
The Clinical Problem
Ankle and foot injuries affect tens of thousands of people and are often difficult to diagnose and treat. Physicians currently use a variety of imaging technologies to evaluate musculoskeletal disease, from magnetic resonance imaging to arthroscopy to x-ray, with varying degrees of success.
Advances in imaging resolution and improved examination techniques are rapidly making ultrasound the imaging modality of choice in the screening of muscles, tendons, ligaments, and other soft tissue structures around the ankle and foot. Ultrasound is cost-effective and is distinct from other imaging modalities because it allows the imager to apply direct stress to soft tissue structures in a real-time fashion. With ultrasound, we can also simultaneously image the opposite joint for comparison. The examination can be custom-tailored to focus on a specific area (affected area of patient’s ankle and foot).
Extra-articular ankle and foot joint pain can be divided into the following regions:
Anterior pain: anterior tibialis tendon (ATT), extensor hallucis longus tendon (EHL), and extensor digitorum longus tendon (EDL)
Medial pain: posterior tibialis tendon (PTT), flexor digitorum longus tendon (FDL), and flexor hallucis longus tendon (FHL)
Lateral pain: peroneus tendons and lateral ligaments
Posterior and plantar pain: Achilles tendon (ACH) and plantar fascia, respectively
Ultrasound can be used also to evaluate soft tissue pathologies around the joint such as ganglion cyst, bursitis, lipoma, joint effusion, and foreign bodies within the foot.
Anatomy
SOFT TISSUE ANATOMY
Ankle Joint
The ankle joint is a synovial articulation acting as a hinge joint, which is formed by mortise (tibia and fibula) and talus. The articulating surfaces of the joint are covered with hyaline cartilage. There is a synovial membrane between the articular margins of the tibia, fibula, and talus. A fibrous capsule surrounds the synovial membrane of the ankle joint. Medially and laterally, there are the collateral ligaments, thickenings of the joint capsule that limit valgus and varus displacement.
Anterior
Passing over the anterior tibiotalar joint space is a group of primary extensor tendons of the ankle that collectively allow dorsiflexion of the joint. From medial to lateral, they consist of the ATT, EHL, and EDL tendons (Fig. 53-1). These extensors are all contained within individual synovial sheaths, which may contain a small amount of normal physiologic fluid. The ATT is the largest in diameter in comparison with the rest of the extensor tendons. The ATT travels medially and then toward the plantar aspect, inserting onto the first medial cuneiform and base of the first metatarsal. Next, located lateral to the ATT, is the EHL tendon; it courses distally over the first toe to insert on the base of the distal phalanx. Lateral to the EHL tendon is the EDL tendon. The EDL branches distally into four separate tendons that insert on the second through fifth toes.
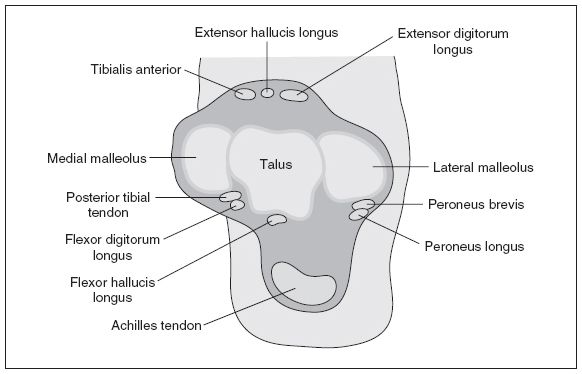
Figure 53-1. ![]() Cross-sectional image of the ankle joint.
Cross-sectional image of the ankle joint.
Medial
Posterior to the bony landmark of the medial malleolus and deep to the flexor retinaculum are a group of tendons and a neurovascular bundle. In a medial to lateral direction (see Fig. 53-3), they consist of the PTT, FDL, neurovascular bundle (posterior tibial artery with venae comitantes and tibial nerve), and FHL. A useful mnemonic to help remember this medial arrangement is:
Tom Dick and A Very Nervous Harry = PTT, FDL (Posterior Tibial Artery, Vein, and Nerve), and FHL
The posterior tibialis muscle originates from the shaft of the tibia and tapers into a long tendon. The PTT hugs the posterior aspect of the medial malleolus and inserts distally onto the tarsal navicular bone. The PTT functions to turn the sole of the foot inward, along with help from the ATT.
The FDL accompanies the PTT and is smaller in diameter. The FDL runs distally along the plantar aspect of the foot to insert on the base of the distal phalanges of the second to fifth toes. The FDL aids in flexing the toes for final push-off in walking.
The FHL originates from the posterior side of the fibula and passes posterior to the talar groove, making it the most lateral of the medial ankle tendons. The FHL inserts onto the plantar aspect of the distal phalanx of the first toe and allows the first toe to flex.
The peroneus longus (PL) and peroneus brevis (PB) course behind the lateral malleolus in the retrofibular groove and are held there by a retinaculum (Fig. 53-2). The PB is located more anteriorly than the longus and closer to the fibula. The PB inserts onto the tubercle of the fifth metatarsal base. The PL descends across the lateral aspect of the calcaneus and crosses over plantarly to insert onto the cuneiform region. The main function of these lateral tendons is to abduct and evert the foot.
The anterior talofibular ligament (ATFL) is the most commonly injured ligament of the ankle. The ATFL originates from the anterior-lateral aspect of the distal fibula and passes anteriorly and medially, inserting onto the neck of the talus (Fig. 53-2). It functions to restrain internal rotation of the talus.
Posterior
The ACH connects the calf muscles to the calcaneus (heel bone) and is made of a strong fibrous band. The calf muscles consist of the two heads of the gastrocnemius muscle and the deep soleus muscle. The contraction of the gastrocsoleus muscle group causes plantar flexion of the foot. The ACH does not have a rich blood supply. It is not invested within a true synovial tendon sheath, but a paratendon composed of fibrous tissue surrounds it. Located deep (anterior) to the distal half of the ACH is Kaegar’s triangular fat pad. There is a deep, retrocalcaneal bursa between the distal anterior wall of the ACH and the posterior superior border of the calcaneus bone (Figs. 53-2 and 53-3).
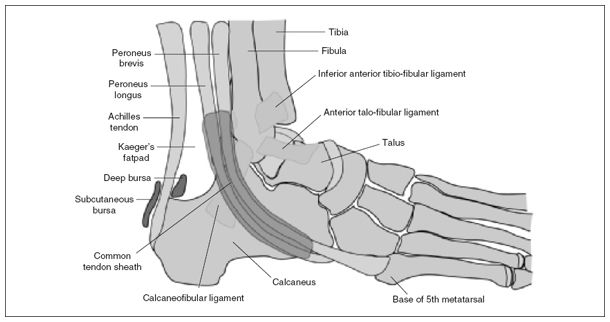
Figure 53-2. ![]() Lateral view of the ankle: peroneal tendons and lateral collateral ligaments.
Lateral view of the ankle: peroneal tendons and lateral collateral ligaments.
The plantar fascia is a dense strip of tissue that runs from the front of the heel bone (calcaneus) to the ball of the foot. There is a large medial band, which originates from the medial tubercle of the calcaneus. A separate, thinner lateral band arises from the lateral tubercle of the calcaneus. The plantar fascia helps to support the longitudinal arch of the foot.
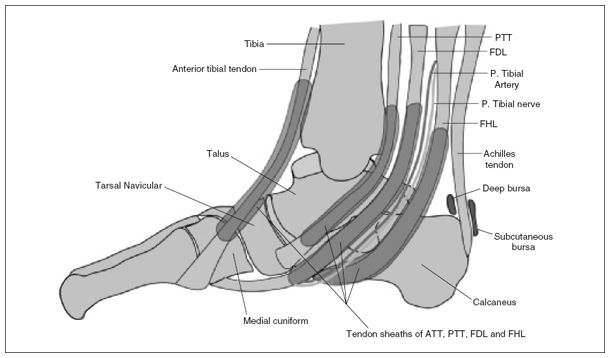
Figure 53-3. ![]() Medial view of the ankle: medial tendons.
Medial view of the ankle: medial tendons.
NORMAL ULTRASOUND APPEARANCE OF MUSCLE AND TENDONS
Muscles
Muscle bundles have a hypoechoic appearance. The fibroadipose septa of the perimysium are seen as hyperechoic lines separating the hypoechoic muscle bundles. This appears as a pennate or feather-like arrangement on ultrasound (Fig. 53-4A).
Tendons
Tendons are composed of parallel running fascicles of collagen fibers. We can see these individual fascicles on high-resolution sonography, especially with high-frequency transducers. Tendon fibers appear more echogenic in comparison with their muscle bellies. The fibers of a tendon appear as echogenic parallel lines and give a regular echogenic striated appearance (Fig. 53-4B). There should be no disruptions or tears within the tendon and its borders. The echogenicity of a tendon may depend on the orientation of the ultrasound beam relative to the tendon structure. This causes an angle-dependent artifact known as “anisotropy” (Fig. 53-5). If the tendon is perpendicular to the central axis of the sound beam, then the tendon will appear echogenic, and the fibers of the tendon will be well visualized. However, if the tendon is not perpendicular but is oblique to the central axis of the sound beam, the tendon will appear more hypoechoic, and the fibers will be suboptimally visualized (Fig. 53-6). Therefore, one must remember to continually tilt the transducer depending on the tendon’s course. Anisotropy may mimic pathologic conditions such as tendinopathy, tendon tears, and abnormal fluid collections.
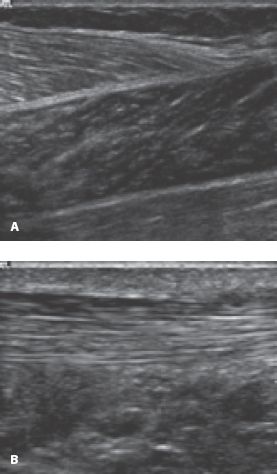
Figure 53-4. ![]() A. Longitudinal image of the medial calf complex shows the feather-like arrangement of a typical muscle bundle. B. Longitudinal image of the Achilles tendon denotes the typical echogenic parallel lines and homogeneous echogenic striated appearance.
A. Longitudinal image of the medial calf complex shows the feather-like arrangement of a typical muscle bundle. B. Longitudinal image of the Achilles tendon denotes the typical echogenic parallel lines and homogeneous echogenic striated appearance.
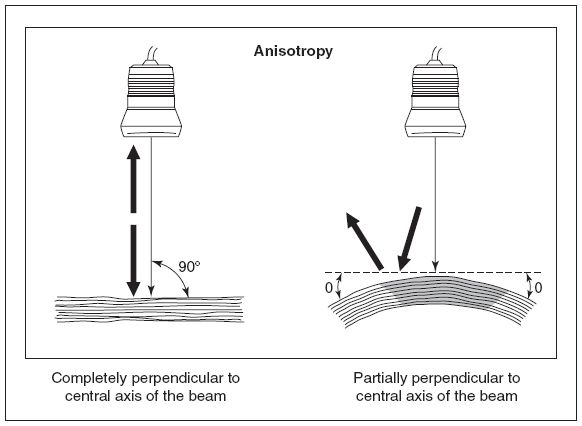
Figure 53-5. ![]() Anisotropy: straight tendon that is perpendicular to the central axis of the sound beam (left). In this case, the tendon appears echogenic and the fibers of the tendon are well visualized. Tendon traveling on a curved path (right). Portions of this tendon are not perpendicular to the central axis of the sound beam. In this case, the tendon appears hypoechoic along the portions that are not perpendicular. In those areas, the fibers of the tendon will be poorly visualized.
Anisotropy: straight tendon that is perpendicular to the central axis of the sound beam (left). In this case, the tendon appears echogenic and the fibers of the tendon are well visualized. Tendon traveling on a curved path (right). Portions of this tendon are not perpendicular to the central axis of the sound beam. In this case, the tendon appears hypoechoic along the portions that are not perpendicular. In those areas, the fibers of the tendon will be poorly visualized.
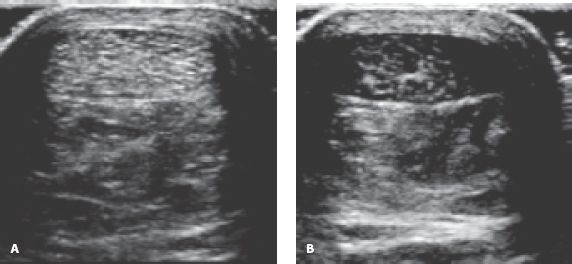
Figure 53-6. ![]() Anisotropy. A. Transverse image of an Achilles tendon that is perpendicular to the central axis of the sound beam. B. Transverse image of Achilles tendon that is not perpendicular but oblique to the central axis of the sound beam. The tendon appears hypoechoic in comparison with images obtained with the ideal angle.
Anisotropy. A. Transverse image of an Achilles tendon that is perpendicular to the central axis of the sound beam. B. Transverse image of Achilles tendon that is not perpendicular but oblique to the central axis of the sound beam. The tendon appears hypoechoic in comparison with images obtained with the ideal angle.
Anterior Approach
We begin our examination of the anterior ankle and foot by laying the patient in a supine position, with the knee flexed so that the symptomatic foot is flat on the examining bed. We first examine the anterior tibiotalar joint and recess in the longitudinal scan plane (Fig. 53-7). This anterior joint recess is located between the echogenic distal tibia and dome of the talus bone. A thin, hypoechoic cartilage layer covers the dome of the talus bone. An echogenic anterior joint capsule drapes over these structures and closes off the joint anteriorly, thereby creating the anterior tibiotalar recess. Normally, this recess contains little or no fluid unless joint effusion is present due to an injury or pathologic process. Interrogate the joint medially to laterally to make sure that the entire anterior recess is scanned.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


