Common Orthopaedic Terminology and General Fixation Devices
Appropriate use of terminology is critical when communicating with orthopaedic surgeons. Common definitions, descriptive terms, eponyms, and proper description of common orthopaedic fixation devices will be discussed in this chapter to avoid redundancy in later anatomic chapters. For ease of discussion, we will review terminology in sections with terms in alphabetic order.
Fracture/Dislocations
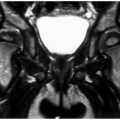
Bone bruise: Marrow edema pattern without a fracture line or cortical disruption best seen on magnetic resonance (MR) images (see Fig. 2-1)
Closed fracture: Osseous disruption with intact overlying soft tissues and no penetrating wound
Complete fracture: Structural break involving both cortices (see Fig. 2-2)
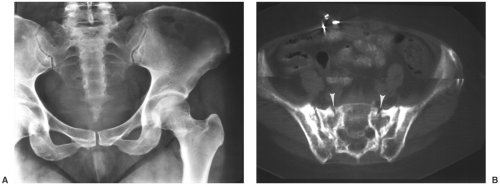
Diastasis: Complete separation of adjacent bones, such as the tibia and fibula, at the syndesmosis or rupture of a nonmobile or minimally mobile articulation such as the sacroiliac joint or pubic symphysis (see Fig. 2-3)
Dislocation: Complete displacement of the articular surfaces of a given joint (see Fig. 2-4)
Fatigue fracture: Fracture resulting from abnormal muscle tension on normal bone (see also “Stress fracture”)
Incomplete fracture: Structural break involving only one cortex (see Fig. 2-5)
Incongruency: Asymmetry of the articular surfaces of a joint with minimal or no subluxation (see Fig. 2-6)
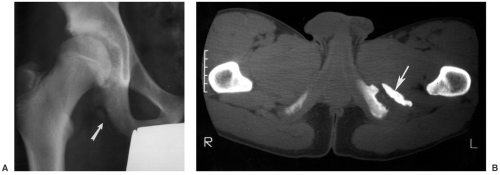
Insufficiency fracture: Osseous injury due to normal stress or muscle tension acting on a bone with abnormal elastic resistance; may only be visible on radionuclide scan, computed tomography (CT), or magnetic resonance imaging (MRI); common locations include the sacrum, acetabulum, pubic rami, and femoral neck (see Fig. 2-7)
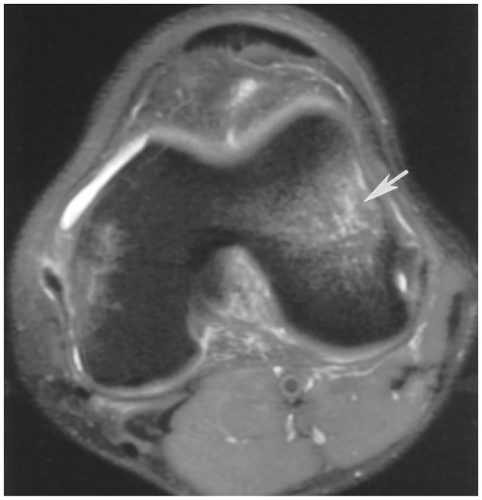
Fig. 2-1 Bone bruise. Axial fat-suppressed T2-weighted magnetic resonance (MR) image demonstrating marrow edema in the femoral condyle (arrow) in a patient with an anterior cruciate ligament tear.
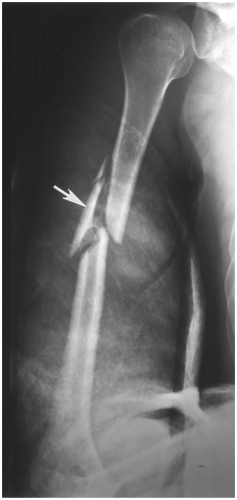
Open fracture: Lack of continuity of skin due to fracture fragment penetration or penetrating wound (see Fig. 2-8)
Stress fracture: Variety of fractures that result from repetitive stress of lesser magnitude than required for an acute fracture; may only be visible on radionuclide scan or MRI (see Fig. 2-9)
Subluxation: Partial displacement of articular surfaces of a joint (see Fig. 2-10)
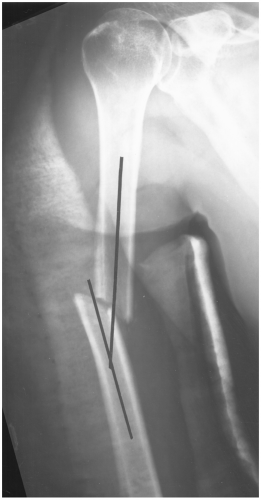 Fig. 2-2 Complete fracture. Oblique fracture of the mid-humerus involving both cortices with lateral angulation (lines). Image taken in a hanging cast. |
 Fig. 2-4 Dislocation. Lateral radiograph of the hand demonstrating a dorsal dislocation of the interphalangeal joint (arrow) with complete loss of articular contact. |
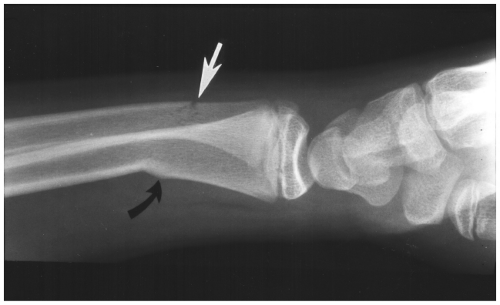 Fig. 2-5 Incomplete fracture. Incomplete fractures of the ulna (white arrow) and radius (curved black arrow). The radial fracture is a torus or buckle fracture. |
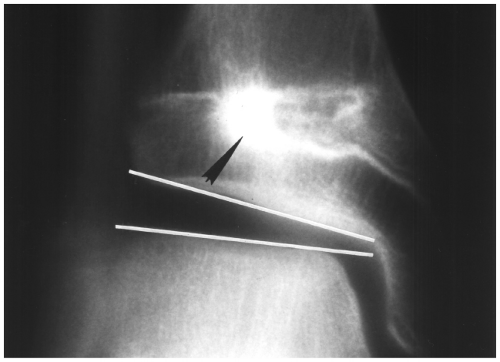 Fig. 2-6 Incongruency. Anteroposterior (AP) radiograph of the ankle with physeal bar after prior growth plate fracture (arrowhead) with resulting joint space asymmetry (lines). |
Descriptive Fracture Terminology
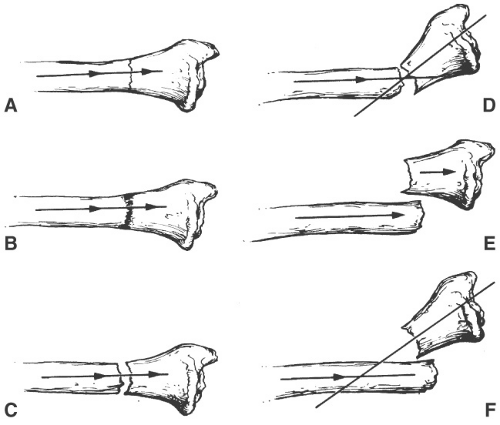
Alignment: Fracture fragment position related to the normal long axis of the involved bone (see Fig. 2-11A–C and E)
Angulated: Loss of normal alignment described by apex direction or displacement of the distal fragment (Fig. 2-11D and F and see Fig. 2-12)
Apophyseal fracture: Avulsion fracture through an apophysis or bony prominence (see Fig. 2-13)
Apposition: Degree of bone contact at the fracture site (see Fig. 2-14)
Avulsion fracture: Fracture caused by abrupt muscle contraction or at a ligament attachment associated with joint separation (Fig. 2-13)
Bayonet position: Fragments touch and overlap, but are in good alignment (Fig. 2-11E)
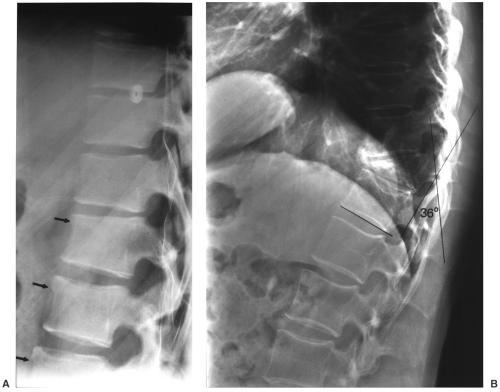
Burst: Fracture of the vertebral body with multiple fragments and expansion of the vertebral body, usually into the spinal canal (see Fig. 2-15)
Butterfly fracture: Triangular fragment displaced from a long bone fracture (see Fig. 2-16)
Comminution: Fracture with more than two fragments (see Fig. 2-17)
Compression: Trabecular fracture with loss of height usually reserved for spinal injuries (see Fig. 2-18)
Condylar: Fracture involving the condyle of the distal humerus or femur (see Fig. 2-19)
Depression: Calvarial or articular fracture with the fragment displaced below the calvarial table or in the case of a joint, below the articular surface (see Fig. 2-20)
Displaced: Fracture fragments angulated, rotated, or separated by >2 mm (Fig. 2-11)
Distraction: Separation of the fragments; may be associated with soft tissue interposition or excessive traction (Fig. 2-11C)
Extracapsular: Fracture near, but outside of the joint capsule
Flake fracture: Linear fracture fragment due to ligament or tendon injury (peroneal tendon dislocation may cause a fibular flake fracture) (see Fig. 2-21)
Impaction: Fracture compressed so the fragment is driven into the adjacent fragment (Fig. 2-11B)
Infraction (pseudofracture): Lucent line in abnormal bone, usually metabolic, such as osteomalacia (see Fig. 2-22)
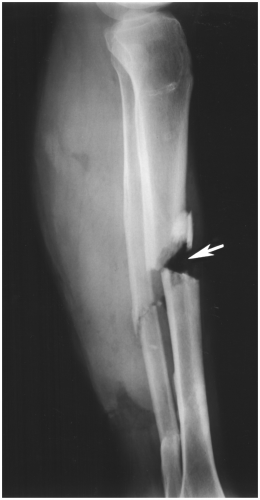
Fig. 2-8 Open fracture. Comminuted fractures of the mid-tibia and fibula with an open wound and air in the wound (arrow) at the fracture site.

Fig. 2-9 Stress fracture. Radiograph of the foot demonstrating subtle periosteal reaction (arrow) due to a stress fracture of the distal second metatarsal. See also march fracture (Fig. 2-77).

Fig. 2-10 Subluxation. Lisfranc injury with partial lateral displacement of the first and second metatarsals (arrows).
Intra-articular: Fracture line enters the joint surface (Fig. 2-20)
Intracapsular: Fracture of the osseous portion of bone within the capsule, but not involving the articular surface (see Fig. 2-23)
Linear: Straight transverse or longitudinal fracture line (see Fig. 2-24A)
Metaphyseal: Fracture involving the metaphysis
Oblique: Fracture line oriented at an angle to the axis of a long bone (Fig. 2-24B)
Occult: Fracture not visible on radiographs, but may be seen on MRI or radionuclide scans (see Fig. 2-25)
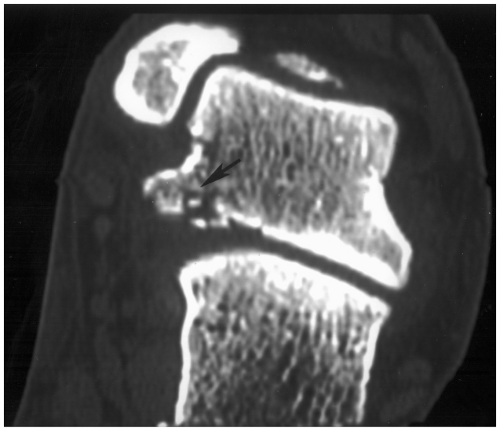
Osteochondral: Fracture involving the cartilage and bone of a joint surface (see Fig. 2-26)
Pathologic: Fracture through abnormal bone (see Fig. 2-27)
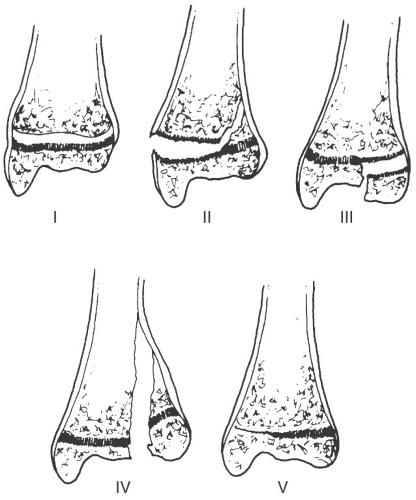
Physeal: Fracture through the physis or growth plate; classified by Salter and Harris (see Fig. 2-28)
Type I—fracture through the physis without metaphyseal or epiphyseal involvement
Type II—fracture of the physis that exits through the metaphysis
Type III—fracture of the physis that exits through the epiphysis
Type IV—fracture line extends through the metaphysis, physis, and epiphysis
Type V—growth plate or physeal impaction or compression
Rotation: Fragment turned on the opposing fragment, usually internal or external rotation (see Fig. 2-29)
Secondary: Fracture in pathologic or weakened bone (Fig. 2-27)
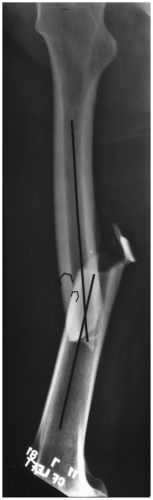
Segmental: Several large fracture fragments in the same long bone (see Fig. 2-30)
Spiral: Fracture line rotates obliquely about the bone, usually due to twisting or rotation injury (Fig. 2-24C)
Stellate: Numerous fracture lines radiating from the central point of injury (see Fig. 2-31)
Subchondral: Fracture beneath the articular surface of the joint, commonly seen with abnormal bone and stress or insufficiency injuries (see Fig. 2-32)
Torus: Incomplete fracture of childhood with cortical buckling (see Fig. 2-33)
Transcondylar: Fracture that crosses the condyles of the distal humerus or femur
Transverse: Fracture line perpendicular to the axis of a long bone (Fig. 2-24A)
Tuft: Fracture of the distal aspect of the distal phalanx in the hand or foot (see Fig. 2-34)
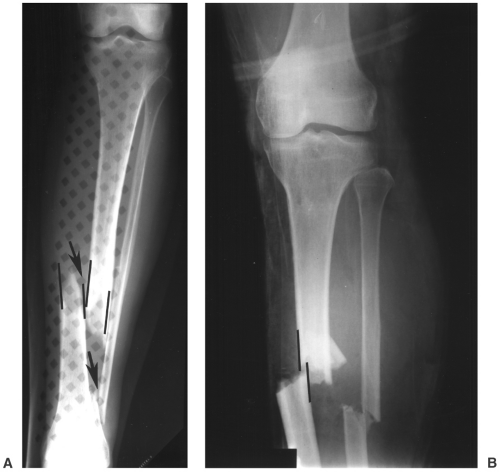 Fig. 2-14 Apposition. A: Anteroposterior (AP) radiograph of the leg demonstrating displaced fractures of the tibia and fibula (arrows) with no cortical apposition of the fracture margins (lines). Splint in place. B: Fractures of the tibia and fibula with minimal apposition (lines). See Figure 2-11A which demonstrates 100% apposition. |
Fracture Healing Terminology
Bone union: Clinical—no pain or motion at fracture site; radiographic—fracture site bridged by trabecular bone and/or callus
Callus formation: Radiographically identifiable periosteal bone formation at the fracture site (see Fig. 2-35)
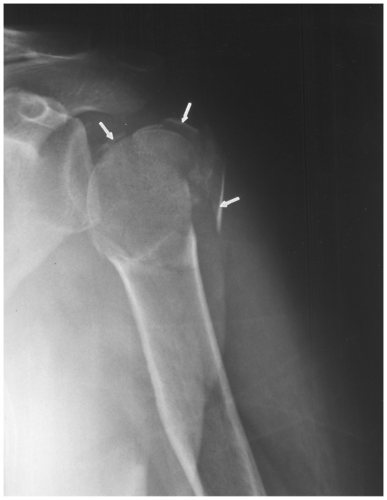
Fig. 2-17 Comminuted fracture. Anteroposterior (AP) radiograph of the humerus demonstrating a displaced, comminuted fracture (arrows).
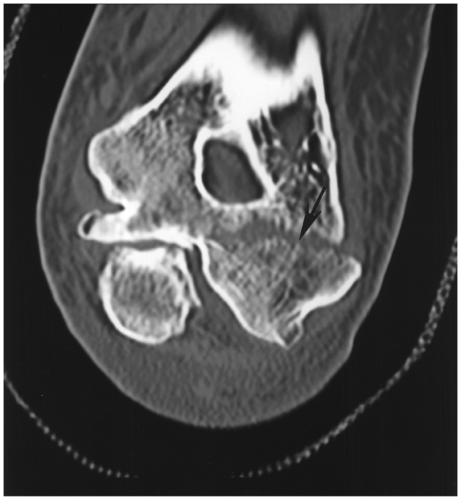
Fig. 2-19 Condylar fracture. Coronal computed tomographic (CT) image demonstrating a condylar fracture of the distal humerus (arrow).
Delayed union: Union (healing) which takes more than the average time for a given anatomic site; fracture ends may be sclerotic on radiographs or CT (see Fig. 2-36)

Fig. 2-20 Depression fracture. Anteroposterior (AP) radiograph of the knee demonstrating a depressed intra-articular fracture of the medial tibial plateau.

Fig. 2-21 Flake fracture. Mortise view of the ankle demonstrating a flake fracture of the fibula (arrowhead) due to peroneal tendon dislocation.
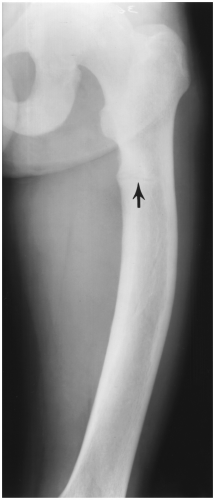
Fig. 2-22 Radiograph of the femur demonstrating a lucent infraction or pseudofracture in a patient with osteomalacia.
Early union: Appearance of trabeculae across the fracture site earlier than expected for a given anatomic site
Established union: Cortical callus organization and remodeling begin (Fig. 2-35C–I)
Fibrous union: No pain at the fracture line with clinical stability; lucent line persists radiographically with low signal intensity on T1- and T2-weighted MR images
Malunion: Fracture heals in poor or nonanatomic position (see Fig. 2-37)
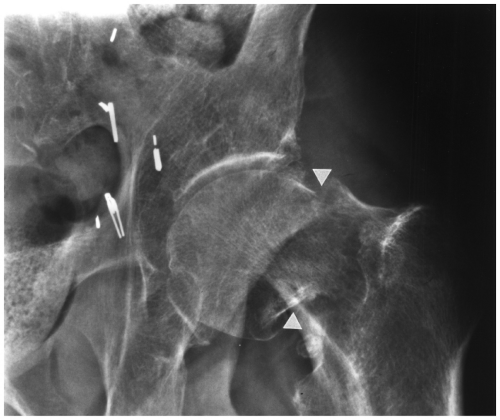
Fig. 2-23 Intracapsular fracture. Anteroposterior (AP) radiograph demonstrating a displaced intracapsular fracture of the femoral neck (arrowheads) without articular involvement.
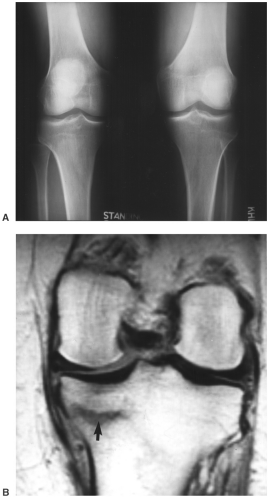
Fig. 2-25 Occult fracture. A: Standing radiographs of the knee in a patient with left knee pain are normal. B: T1-weighted magnetic resonance (MR) image demonstrates a linear stress fracture (arrow).
Nonunion: Diagnosed by clinical evaluation due to failure to heal properly; radiographic features:
Atrophic—atrophy of fracture ends (see Fig. 2-38)
Hypertrophic—prominent hypertrophic nonbridging callus at the fracture site (see Fig. 2-39)
Phases of healing: There are three phases of fracture healing (Fig. 2-35)
Reactive phase—fracture and inflammatory phase; granulation tissue formation; first 10% of healing process
Reparative phase—callus formation and lamellar bone deposition; second 40% of healing process
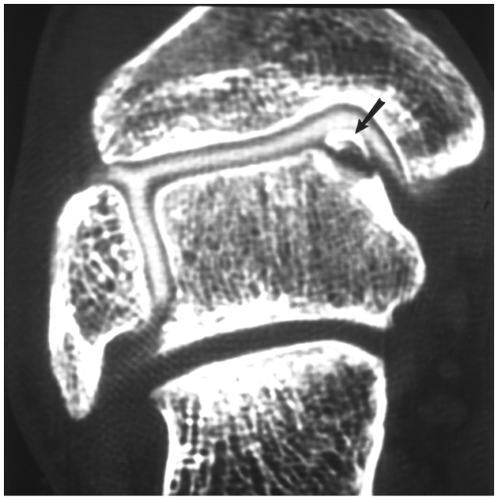
Fig. 2-26 Osteochondral fracture. Coronal computed tomographic (CT) arthrogram demonstrating a displaced osteochondral fracture (arrow) of the talar dome.

Fig. 2-27 Pathologic fracture. Anteroposterior (AP) (A) and lateral (B) radiographs demonstrating a fracture through a femoral metastasis. Traction in place.
Remodeling phase—remodeling of original bone contour; 70% of healing process
Pseudarthrosis: Nonunion with formation of a synovial lined capsule in the fracture line
 Fig. 2-30 Segmental fracture. Anteroposterior (AP) radiograph of the femur demonstrating three large shaft fragments. |
Fracture/Dislocation Eponyms
Ankle mortise diastasis: Separation of the distal tibia and fibula due to syndesmotic and interosseous ligament tears; may be associated with dislocations (see Fig. 2-40)
Archer’s shoulder: Recurrent posterior subluxation or dislocation of the shoulder
Aviator’s astragalus: A variety of fractures of the talus caused by impaction of the foot into the ankle; may be associated with subtalar or tibiotalar dislocations (see Fig. 2-41)
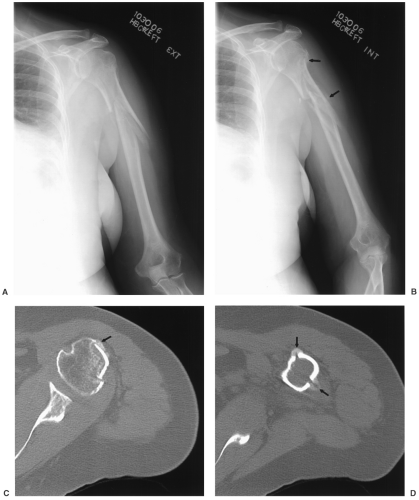
Bankart: Anterior-inferior glenoid rim or labral detachment seen with anterior dislocations (see Fig. 2-42)
Barton: Intra-articular fracture of the dorsal or volar lip of the distal radius (see Fig. 2-43)
Baseball finger: Hyperflexion injury of the distal interphalangeal joint due to extensor tendon avulsion, which may have
an associated osseous fragment (dropped or mallet finger) (see Fig. 2-44)
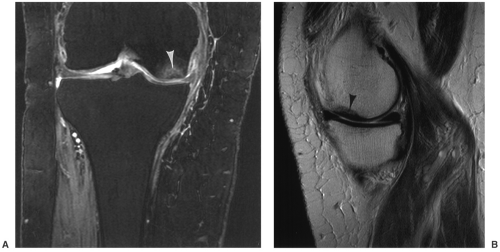
Fig. 2-32 Subchondral fracture. Coronal double echo steady state (DESS) (A) and sagittal T1-weighted (B) magnetic resonance (MR) images demonstrating a subchondral fracture (arrowheads).
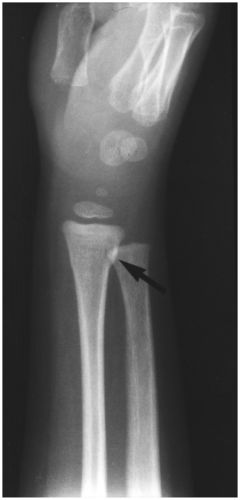
Fig. 2-33 Torus fractures. Oblique radiograph demonstrating subtle buckling of the radial cortex (arrow). Also see Figure 2-6.
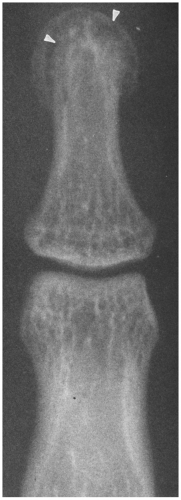
Fig. 2-34 Tuft fracture. Posteroanterior (PA) radiograph of the finger demonstrating a comminuted fracture of the phalangeal tuft (arrowheads).
Basketball foot: Subtalar dislocation (see Fig. 2-45)

Fig. 2-36 Delayed union. Anteroposterior (AP) radiograph demonstrates a mid-tibial fracture with sclerotic margins and hypertrophic nonbridging callus 5 months after injury.

Fig. 2-37 Malunion. Healed fracture of the proximal phalanx with angulation (lines) rotation and articular incongruency.
Bennett: Intra-articular fracture of the base of the first meta-carpal with volar ulnar fragment due to the attachment of the strong ulnar oblique ligament (see Fig. 2-46)
Boot top: Fractures of the distal third of the tibia and fibula at the level of the top of a ski boot (see Fig. 2-47)
Bosworth: Fracture dislocation of the ankle with an oblique distal fibular fracture with locking of the distal fragment behind the tibia
Boutonniere deformity: Hyperflexion of the proximal interphalangeal joint of the finger with hyperextension of the distal interphalangeal joint due to disruption of the central extensor tendon (see Fig. 2-48)
Boxer: Fracture of the fifth metacarpal neck with palmar displacement of the metacarpal head and dorsal angulation at the fracture site (see Fig. 2-49)
Boxer’s elbow: Chip fracture of the olecranon due to rapid extension of the elbow
Bucket handle: Vertical shear injury to the pelvis with fracture of the anterior pubic rami and opposite ilium or sacroiliac (SI) joint diastasis (see Fig. 2-50)
Bumper: Fracture of the tibia or femur due to a direct blow to the tibial tuberosity region caused by car bumper; may be bilateral
Bunkbed: Childhood fracture involving the intra-articular base of the first metatarsal
Buttonhole: Perforation fracture of bone associated with penetrating injury such as a gunshot wound (see Fig. 2-51)
Cedell: Fracture of the posterior talar process (see Fig. 2-52)

Fig. 2-38 Nonunion. Atrophic nonunion of the distal humerus demonstrated on frontal (A) and lateral (B) radiographs. Note the atrophy of the fracture ends (arrowheads). Compare to Figure 2-39 which is hypertrophic nonunion.
Chance: Flexion distraction injury of the spine with posterior ligament injury and fracture and associated, although often mild, anterior vertebral compression; usually at L1 or the thoracolumbar junction; associated with lap seat belts (see Fig. 2-53)
Chaput: Fracture of the anterior tubercle of the distal tibia due to avulsion of the distal anterior tibiofibular ligament
Chauffeur: Intra-articular fracture of the radial styloid; also called backfire fracture (see Fig. 2-54)
Chisel: Intra-articular fracture of the radial head with extension distally approximately 1 cm from the central articular surface (see Fig. 2-55)
Chopart: Fracture dislocation of the talonavicular and calcaneocuboid articulations; derived from surgical amputation at these joints described by Chopart (see Fig. 2-56)
Clay shoveler: Isolated or multiple fractures of the spinous processes; most often affecting the lower cervical and upper thoracic spine (see Fig. 2-57)
Coach’s finger: Dorsal dislocation of the proximal interphalangeal joint (Fig. 2-4)
Colles: Fracture of the distal radial metaphysis with dorsal displacement of the distal fragment; may or may not have associated ulnar styloid fracture (see Fig. 2-58)
Cotton: Trimalleolar ankle fracture with the posterior and superior displacement of the posterior tibial fragment
Dashboard: Fracture of the posterior acetabular rim caused by force transmitted from the knee to the femur and hip during a motor vehicle accident (see Fig. 2-59)
De Quervain: Fracture of the scaphoid with volar displacement of the proximal fragment and lunate
Desault: Dislocation of the distal radioulnar joint; best demonstrated on axial CT or MR images in neutral, pronation, and supination (see Fig. 2-60)
Descot: Fracture of the distal posterior margin of the tibia (third malleolus) (see Fig. 2-61)
Die punch: Depression fracture of the lunate fossa of the distal radius with proximal migration of the lunate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree