, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
Abstract
In this chapter, we will describe some tips in the assessment of cervical spine imaging in patients presenting with neck pain and/or cervical radiculopathy. We will also detail imaging findings of cervical spondylotic myelopathy, cervical spondylotic radiculopathy, and cervical herniated intervertebral disks.
In this chapter, we will describe some tips in the assessment of cervical spine imaging in patients presenting with neck pain and/or cervical radiculopathy. We will also detail imaging findings of cervical spondylotic myelopathy, cervical spondylotic radiculopathy, and cervical herniated intervertebral disks.
3.1 Cervical Spine Imaging in Patients with Neck Pain: What Should We Focus on?
Common spinal disorders associated with neck pain include cervical spondylotic myelopathy (CSM), cervical spondylotic radiculopathy (CSR), and cervical herniated intervertebral disks (HIVD). A routine plain radiograph series may consist of up to six images: anterior-posterior (AP), lateral, lateral with flexion and extension, and both oblique views. On AP radiographs, careful evaluation for uncovertebral hypertrophy on both sides of the upper vertebral endplates should be made. On the lateral view, alignment disorders, ossification of the posterior longitudinal ligament (OPLL), and posterior osteophytes may be observed. On flexion/extension views, segmental instability should be determined by assessing for a change of angulation and displacement. On oblique views, the ipsilateral neural foramen is best demonstrated and foraminal stenosis caused by uncovertebral hypertrophy can be observed. For example, in the left anterior oblique view, the left neural foramen is imaged en face and appears widest due to its anterolateral course.
With three-dimensional CT, endplate osteophytes, uncovertebral hypertrophy, and OPLL are easily visualized, while soft disk herniation may be diagnosed by adjusting window level and width settings.
MR is the best method to evaluate spinal pathology including that of the spinal cord. On T2-weighted images, apart from screening the central canal for any pathology obliterating the cerebrospinal fluid space around the cord such as a herniated disk or central canal stenosis due to a bulging disk or ligamentum flavum buckling, it is also important to carefully evaluate the spinal cord. Most pathology involving the spinal cord shows high signal change on T2-weighted images. On T1-weighted images, the signal intensity of the bone marrow should be carefully assessed. Soft disk herniation and osteophytes can be differentiated on T1-weighted images, as disk herniation is usually of isointense signal to the parent disk while osteophytes are usually of lower signal intensity.
Table 3.1
Cervical spine imaging in patients with neck pain: what should we focus on?
AP radiograph | Uncovertebral hypertrophy on both sides of the upper endplate |
Lateral radiograph | Alignment disorders, ossified posterior longitudinal ligament (OPLL), posterior osteophytes |
Lateral radiographs in flexion and extension | Segmental instability |
Oblique radiographs | Ipsilateral neural foraminal stenosis from uncovertebral hypertrophy |
CT | Osteophytes, uncovertebral hypertrophy, OPLL |
T2-weighted MR images | Herniated disk, central canal stenosis, spinal cord pathology |
T1-weighted MR images | Bone marrow signal change, soft disk herniation |
3.2 Cervical Spondylotic Myelopathy
Cervical spondylotic myelopathy (CSM) is a condition in which degenerative changes of the cervical spine result in myelopathy from spinal cord compression. The common mechanical compressive factors contributing to CSM include bulging disks, buckling of the ligamentum flavum, posterior osteophytes, or ossification of the posterior longitudinal ligament. These mechanical compressive factors both directly injure neural tissue and initiate secondary ischemia, inflammation, and apoptosis. The histologic characteristics of CSM include cystic cavitation and gliosis of the central gray matter and demyelination of the medial portions of the white matter long tracks. There is Wallerian degeneration of the posterior columns and posterolateral tracts cephalad to the site of compression, with loss of anterior horn cells and corticospinal tract degeneration at and caudal to the site of compression (Baptiste and Fehlings 2006; Maus 2012).
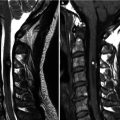
The diagnosis of cervical central canal stenosis and grading of its severity can be made by assessing for cerebrospinal fluid (CSF) obliteration around the spinal cord, spinal cord deformity, and intramedullary T2 high signal change. In grade 1 central canal stenosis, there is central canal narrowing resulting in more than 50 % obliteration of the subarachnoid space around the spinal cord anteriorly and/or posteriorly without spinal cord deformity. Central canal narrowing with deformity of the spinal cord is defined as grade 2 central canal stenosis. Central canal narrowing with intramedullary T2 high signal change is defined as grade 3 central canal stenosis (Kang et al. 2011).
In patients with CSM, T2 hyperintensity in the spinal cord represents edema, demyelination, gliosis, and cystic necrosis. The observed changes may be reversible or irreversible. Faint and indistinct T2 hyperintensity in the spinal cord is more likely to reflect reversible edema, but intense and well-defined T2 hyperintensity more likely represents fixed gliosis or cystic necrotic changes. T1 hypointensity in the spinal cord represents irreversible necrosis and myelomalacia (Al-Mefty et al. 1988; Ohshio et al. 1993; Ramanauskas et al. 1989; Takahashi et al. 1989; Taneichi et al. 1994).
3.3 Cervical Spondylotic Radiculopathy
In the cervical spine, uncovertebral hypertrophy with foraminal stenosis is a more common cause of radiculopathy than HIVD, in contrast to the lumbar spine. The term “cervical spondylotic radiculopathy” (CSR) refers to degenerative narrowing of the cervical neural foramen causing nerve root compression and subsequent radiculopathy. The primary imaging finding of cervical spondylotic radiculopathy is cervical foraminal stenosis mainly caused by uncovertebral hypertrophy or facet osteophytes.
Uncovertebral hypertrophy is seen on AP radiographs as laterally orientated bony projections of the uncovertebral joints (especially from the uncinate processes). On lateral radiographs, uncovertebral hypertrophy can be seen as a double line just above the lower cortical margin of the vertebral body. On oblique views with the ipsilateral neural foramen shown en face, the uncovertebral joint is situated anterior to the neural foramen.
On CT images, uncovertebral hypertrophy can be easily identified on axial and oblique sagittal reconstructed images. However, optimal window settings are required in proper evaluation of the neural foramen because the margins of the uncovertebral joints may be obscured and result in exaggeration of foraminal stenosis under different window settings. It is important to set the window level and width settings to display the bony cortical margins sharply.
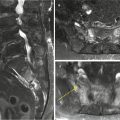
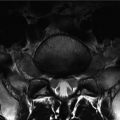
On MR images, axial images are better than sagittal images in evaluating the neural foramina. On axial images, both the disk level and the level at the inferior aspect of the vertebral body above the disk are important in assessing neural foraminal stenosis because (1) the nerve root exits through the inferior portion of the neural foramen at the disk level and at the inferior aspect of the vertebral body above the disk (in contrast to the lumbar spine where the nerve roots exit through the superior portion of the neural foramina) and (2) uncovertebral hypertrophy is best seen at these two levels as the uncinate processes project superiorly. As such, on axial T2-weighted images the AP diameter of the neural foramen at both the disk level and inferior aspect of the vertebral body above the disk should be carefully reviewed for narrowing from uncovertebral or facet hypertrophy. Even though oblique sagittal MR images show the patency of the neural foramen best, most institutions do not include these routinely.
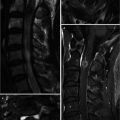
3.4 Herniated Intervertebral Disk
In many cases, it is not easy to differentiate HIVD from endplate osteophytes on MR. CT images can help in the differentiation of HIVD from osteophytes. On MR, careful review of the T1-weighted sagittal images may provide a clue in identifying HIVD, as HIVD is seen as intermediate signal intensity isointense and in contiguity with the parent disk, in contrast to posterior osteophytes or a thickened PLL. Posterior osteophytes are of low signal intensity similar to the vertebral cortex, while thickened PLL is also of low signal intensity on T1-weighted images. On gradient echo T2-weighted images, cervical HIVDs are of high signal intensity similar to the central portion of the intervertebral disk, compared to the low signal seen in osteophytes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree