Overview
Chronic liver disease (CLD) is a significant cause of morbidity and mortality worldwide, and in Chapter 1 the extent of the problem is fully discussed. There are now effective treatments for liver disease caused by hepatitis B or hepatitis C virus, and these causes are expected to continue to decrease in incidence over time. Nonalcoholic fatty liver disease (NAFLD) is a worldwide problem, and the incidence is expected to increase worldwide. The only treatment at this time is lifestyle intervention.
B-mode ultrasound (US) plays a major role in the diagnostic imaging armamentarium for CLD. Because it is widely available, repeatable, relatively inexpensive, cost effective, and poses no exposure to ionizing radiation, US is usually the first imaging modality in the evaluation of liver disease. In patients with advanced CLD, a surveillance program for hepatocellular carcinoma (HCC) with B-mode US performed every 6 months, with or without alpha-fetoprotein, is recommended by guidelines issued by several scientific societies.
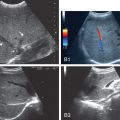
However, even combined with Doppler, B-mode US is not able to adequately characterize focal liver lesions (FLLs). Contrast-enhanced US (CEUS) provides information on tissue perfusion and allows excellent differential diagnosis of FLLs based on arterial phase enhancement patterns and assessment of the timing and intensity of wash-out. It has an accuracy similar to computed tomography and magnetic resonance imaging, which are the established imaging methods for an accurate diagnosis of FLLs. CEUS liver imaging reporting and data system (LI-RADS) provides a detailed methodology for the characterization of FLLs in patients with CLD.
Doppler US coupled with B-mode US may help in the diagnosis of portal hypertension (PH). Doppler parameters, especially of the portal vein, correlate with PH and were largely used in the past; however, they represent additional findings and should be integrated with other data rather than used independently for PH diagnosis. The presence of typical signs might allow the diagnosis, but the absence of these signs cannot exclude it. Newer methods of quantifying PH are being evaluated but remain at the research phase as of early 2022.
Over the past several years, other US-based techniques have been introduced, leading to the possibility of a US-based multiparametric approach for the evaluation of diffuse liver disease.
With the availability of shear wave elastography (SWE) techniques, the number of liver biopsies performed for staging liver fibrosis in several clinical scenarios has drastically decreased. It must be considered that SWE techniques were validated using liver histology as the reference standard. However, elastography measures the stiffness, not fibrosis, and therefore it is inappropriate to report and interpret the values using a histological classification. Moreover, stiffness is a quantitative estimate, whereas the histological scoring systems for liver fibrosis staging are based on categorical scales. Therefore, even in “ideal” conditions, an overlap between consecutive stages of liver fibrosis is inevitable when using liver stiffness (LS) as a surrogate marker of liver fibrosis. It is recommended that LS values be interpreted as the probability of compensated advanced chronic liver disease (cACLD), which is what is most clinically relevant.
Before performing liver elastography, the patient should be evaluated clinically. As highlighted by guidelines/consensus on liver SWE, the interpretation of LS measurement (LSM) depends on the specific clinical scenario, the prevalence of disease in the population under investigation, the current patient’s comorbidities, and the cause of the liver disease.
For all US SWE techniques, adherence to a strict protocol when assessing LS is required for obtaining the most reliable measurement. Factors that affect the reproducibility of the measurement are similar across the different techniques and are related to the operator’s experience and to factors dependent on the subject being examined.
To-date, most studies have been performed in patients with viral hepatitis or NAFLD. However, evidence is growing about the use of SWE techniques in other causes of liver disease, mainly alcohol-related, cholestatic, and autoimmune liver disease.
For patients with virus-related chronic hepatitis or with NAFLD, guidelines have suggested to interpret LSMs by vibration controlled transient elastography (VCTE) and acoustic radiation force impulse (ARFI)–based techniques by using the “rule of 5” and “rule of 4,” respectively. ,
In monitoring fibrosis over time, it should be kept in mind that there is a rapid decline of LS in patients with chronic hepatitis C who have been successfully treated with direct-acting antiviral (DAA) agents. This is mainly because of its positive effect on reducing liver inflammation. Therefore the use of LS cutoff values obtained in untreated patients can underestimate liver fibrosis in patients who have achieved sustained virologic response with DAA agents. In this setting, the Society of Radiologists in Ultrasound consensus has proposed to use the delta change of LSM over time instead of the absolute value as the best method to assess progression or regression of CLD and to consider as baseline stiffness value the one obtained at the end of the treatment in patients with hepatitis C virus. Obtaining an LSM before DAA agent treatment is helpful. If the patients have cACLD before treatment, they are still at elevated risk, although to a lesser extent, for the complications including HCC, PH, and varices and thus require continued monitoring for complications.
Elastography has been used for evaluating the longitudinal changes in LSMs in patients with chronic hepatitis undergoing antiviral treatment, and a significant decline of LS in the long-term follow-up has been reported. However, without histological confirmation with paired liver biopsies, whether the decrease in LSMs is associated with regression of liver fibrosis, improvement in necroinflammation, or both is unclear.
Elastography has been proposed as a tool to predict the risk of death or complications in patients with CLD. In patients with cACLD, the risk of liver decompensation increases with increasing LSM. LSM by VCTE combined with platelets count is a validated noninvasive method for varices screening with very good results in terms of invasive procedures being spared (see Chapter 8 ). ARFI-based techniques also show promising results in this setting (see Chapter 8 ).
In patients with chronic viral hepatitis, the risk of developing liver-related events cannot be completely eliminated, even in those who achieve complete virological response; this risk is mainly related to the degree of liver fibrosis before starting the treatment. Some models that include LSM have been developed to predict the risk of HCC in patients with chronic hepatitis B treated with antivirals (see Chapter 7 ).
Screening for liver fibrosis in the general population is not recommended by guidelines; however, because of the high prevalence of CLD and the development of cirrhosis and HCC as major causes of death worldwide, such possibility in subjects at risk is gaining interest.
The diagnosis and quantification of hepatic fat can predict future development of diabetes and other cardiovascular events. Moreover, it has been shown that significant steatosis is associated with fibrosis progression in patients with NAFLD; therefore the quantitative assessment of the fat in the liver is of great interest. B-mode US gives a subjective estimate of fatty infiltration and has low sensitivity for mild steatosis. There is also a substantial intra- and interobserver variability. Moreover, the presence of an underlying CLD may reduce the accuracy of US in the diagnosis of hepatic steatosis. To improve the quantification of liver fat with B-mode US, some indices and scoring systems, including the hepatorenal index, have been proposed. However, they are impacted by the operator’s experience and lack validation in large cohorts.
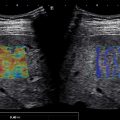
As of early 2022, quantitative US parameters for liver fat estimate are attenuation coefficient (AC), backscatter coefficient, and speed of sound. Most of the commercially available algorithms are those that estimate the AC. Controlled attenuation parameter (CAP), which was the first commercially available, needs a dedicated device that does not allow a morphological evaluation of the liver. It is obtained together with LSM and has become a point-of-care technique that is easy to use in the hepatologist’s office. A large overlap of CAP values between consecutive grades of liver steatosis has been reported, thus limiting its use in follow-up studies that evaluate changes over time. Moreover, the cutoffs are not clearly defined. The AC algorithms available on US systems seem to have good accuracy in quantifying hepatic steatosis. The major advantage on using them is that the fat quantification is obtained together with B-mode evaluation and other US parameters. These algorithms have only recently been introduced, and their use needs to be standardized.
Ultrasound multiparametric approach
There are now several US parameters that can be obtained for evaluation of CLD in a fast, relatively inexpensive, widely available, reproducible manner using a nonradiation technique. These include evaluation with conventional B-mode US, LS evaluation with SWE, fat quantification using quantitative US, dispersion imaging, Doppler US, and CEUS for the characterization of FLLs.
As of early 2022, not all the new techniques are implemented in all US systems, but it is expected that they will be in the near future, at least on high-end systems. Fortunately, attenuation imaging does not require expensive hardware or software and should be available on mid-range and low-range US systems soon. The ability to quantify liver fat is needed worldwide to identify patients with NAFLD in screening programs who are at risk for nonalcoholic steatohepatitis (NASH) so these patients can be triaged for appropriate treatment and follow-up. Liver elastography either by the VCTE or ARFI-based techniques continues to improve, and there is a trend for better standardization between vendors as well as improved quality of measurements. Both VCTE and ARFI-based techniques have matured, and appropriate guidelines for how to acquire LSMs as well as interpret the results are available. The confounding factors and artifacts are well defined as presented in Chapters 4 and 6 .
SWE provides biomechanical information regarding tissue elasticity. However, all tissues are viscoelastic. Dispersion is related to the frequency dependence of the shear wave speed (SWS) and is affected by the attenuation of shear waves because of the viscous component of the tissue. If a tissue is dispersive, the SWS and the attenuation of the shear waves will increase with frequency. Analysis of the dispersion properties of the shear waves can therefore serve as an indirect method for measuring viscosity. Shear wave dispersion is a US parameter that is only recently commercially available and that seems to provide more information than SWE alone. Dispersion imaging is still a relatively new technique, and more studies are needed to understand the extent of the additional information that can be obtained for evaluating CLD. Early research from a small number of centers suggests it may be helpful in assessing liver inflammation. Nevertheless, other factors that may influence the dispersion slope results are not yet well understood. This technique, which evaluates the change of SWS at different frequencies, should provide information related to the viscosity of tissue. However, it is not known what the best range of frequencies is to obtain information on CLD. The dispersion parameter is usually acquired at the same time as the LS value. Another interesting feature of the use of dispersion is that a reference frequency may be selected that can be used to better standardize the various systems acquiring LS.
Ideally, multiparametric ultrasound (MP-US) will help identify patients at risk of CLD at an earlier stage of disease, prompting earlier treatment intervention so they do not progress to cACLD. With low cost, rapid fat quantitation screening for fatty liver disease can detect patients at risk, and intervention can be started at an early stage to decrease the progression to NASH and its consequences. Whether the use of LSMs and dispersion will allow assessing the probability of NASH and monitoring the patient’s progression or regression of disease, as well as monitoring treatment, still remains to be defined by futures studies. If a patient has progressed to cACLD, US screening for development of the complications (HCC, PH, varices) is advised. If a focal lesion is identified, it can be characterized with CEUS using the CEUS LI-RADS scoring system. Early detection of HCC is necessary to impact the survival of the patient. CEUS can be used to guide treatment interventions as well as follow-up treatment for HCC.
Future advancements
Liver stiffness measurements
One problem with MP-US is evaluation of patients with high body mass index (BMI). The accuracy of LSM decreases in these patients because of the attenuation of the ARFI pulse and poorer B-mode image to track the shear waves. One method of improving evaluation of patients with a high BMI is to use a US system equipped with a lower frequency transducer that allows for stronger ARFI pulses at depth at the expense of B-mode image resolution. This has been adopted by one vendor, and the transducer is also able to evaluate the liver deeper in B-mode and color-Doppler US but with some decrease in resolution. The transducer also allows for CEUS image improvement at depth in the liver. There is some interest in having the power limit for ARFI increased so that more energy deposition will create larger shear waves, especially at a depth where there is presently a problem.
Another method in the research phase is using external vibration sources to generate shear waves similar to that in magnetic resonance elastography. This can be done having a “shaker” incorporated in the scanning table or using speakers (sound waves) incorporated into the scanning table or placed on the patient. , A US algorithm can then be applied to determine the LS. The system can only generate one frequency at a time but is able to have adequate shear waves present throughout the liver. Artifacts are not well defined at this stage of development. This could allow for better LS at depth and may not be influenced by the frequency bandwidth associated with the ARFI techniques.
A technique called time-harmonic ultrasound elastography (THE) that is based on US and continuous vibrations produced by a loudspeaker integrated in the patient bed has been developed. THE employs continuous harmonic shear vibrations at several frequencies from 30 to 60 Hz in a single examination and determines the elasticity and the viscosity of the liver from the dispersion of the SWS within the applied frequency range. The mechanical excitation is able to reach a deeper part of the liver, allowing assessment of stiffness in morbidly obese individuals. THE is not commercially available yet, and the published studies so far have been performed by a single center.
Elastance is a method that uses multiple acoustic speakers that are either placed on the scanning table beneath the patient or other acoustic speakers that can be placed appropriately on the patient near the area to be assessed. The technology allows for multiple frequencies from 50 to 2000 Hz to be utilized at the same time, creating a reverberant field (a complex pattern of waves). The US transducer can be used to acquire the information from all the applied frequencies and generate a dispersion curve over the frequencies that were applied. At each frequency, a LS value can be obtained. The acquisition of the data can be performed in less than 1 minute. Preliminary work on patients with a high BMI confirmed that the reverberant field is present throughout the liver, allowing for measurements at various depths, and is not limited by patient body habitus. The artifacts using this system are still not well understood.
Measuring of portal pressure
Presently the most accurate method of measuring the portal pressure is the hepatic venous pressure gradient, which is an invasive and expensive technique that has some risks and is not widely available. A noninvasive test that allows for quantifying PH and is able to monitor changes with treatment would be extremely helpful in the assessment and treatment of PH. Spleen stiffness studies suggest it may be a biomarker of portal pressures. This is more developed for VCTE than ARFI techniques, and more research is needed as of early 2022.
The use of subharmonic CEUS is at a very early research stage as of early 2022, and its accuracy is not known. In this technique, US contrast bubbles are injected into the vascular system, and subharmonic imaging is used to assess the response of the bubbles. The response of the bubbles can be then correlated with pressure.
Another possible method to compute the volume flow is in very early development by the Quantitative Imaging Biomarker Alliance (QIBA) Volume Blood Flow Biomarker Committee. This technique combines standard Doppler measurements and gray-scale decorrelation. Using steered Doppler to determine the in-plane velocities, out-of-plane velocities from the temporal A-line decorrelation can be estimated. The result is a three-dimensional vector flow field computed over the imaging plane without using the vessel orientation. The volume flow is computed by integrating the out-of-plane flow over the vessel cross-section.
Assessment of inflammation
The use of dispersion imaging, which assesses how the LS changes when the ARFI frequency is changed, theoretically can provide information on the tissue viscosity as discussed previously. Inflammation should change the tissue viscosity, and therefore dispersion imaging may provide some information on inflammation. However, it seems that several cofactors may affect the shear wave dispersion values, and the clinical implications of these intricate interrelationships need to be better clarified in future studies. The use of present ARFI modalities only allows for a small range of ARFI frequencies. It is not known which frequency ranges would provide the most information on CLD. The research systems using external vibratory methods may be able to allow for a much greater range of frequencies and could provide more information than the present approved systems. ,
Conclusions
The US techniques presently available for clinical use when taken together (i.e., a multiparametric approach) allow for assessment of CLD from any cause. MP-US is a nonradiation technique, relatively inexpensive, that is widely available but does require adequate training to obtain accurate results. New improvements to existing technology and new techniques in the research phase as of early 2022 should only improve the ability to assess CLD with MP-US, providing a complete assessment of the patient’s condition in a rapid and noninvasive manner that can be used to follow patients over time. The assessment of LS, dispersion, and biomarkers of portal pressure for the near future will require a high-end system for accurate measurements. However, the techniques to quantify liver fat content will likely be implemented on low-end systems, allowing for screening for NAFLD and, if these techniques prove to be accurate and reproducible, for triaging patients at risk for NASH for further evaluation.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree