Fig. 19.1
Esophageal atresia with tracheoesophageal fistula in a neonate with excessive oral secretion. (a) Chest radiograph at 1 hour of life shows the blind-ending proximal esophageal pouch distended with air and coiled tube. (b) Chest radiograph at 1 day of life demonstrates infiltration of the right upper and middle lobes. The presence of gas in the stomach indicates fistulous communication between the lower esophageal segment and trachea. (c) The distal TEF and distal esophageal pouch (arrows) are briefly outlined by air on air esophagogram
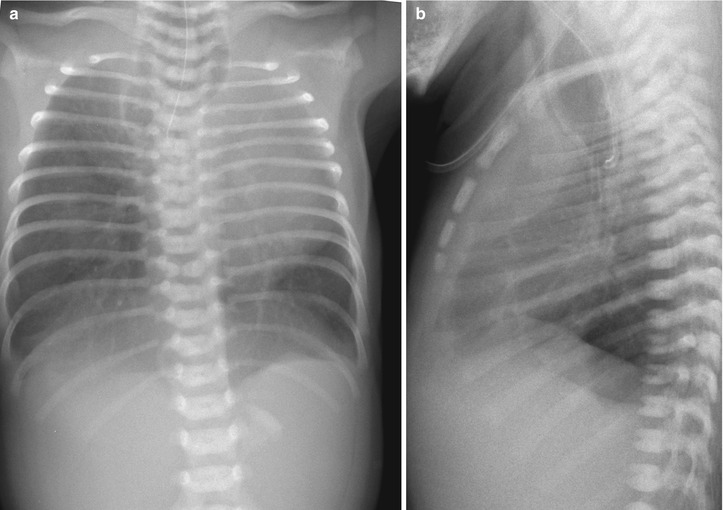
Fig. 19.2
Esophageal atresia without tracheoesophageal fistula in a 1-day-old neonate with high-type imperforate anus. (a) Chest radiograph shows a radiopaque tube curling in the distended proximal esophageal pouch and gasless abdomen indicating lack of a distal TEF. Note coronal cleft in the eighth thoracic vertebra. (b) Lateral radiograph clearly demonstrates the distended proximal esophageal pouch with resulting anterior bowing and pressure deformity of the trachea
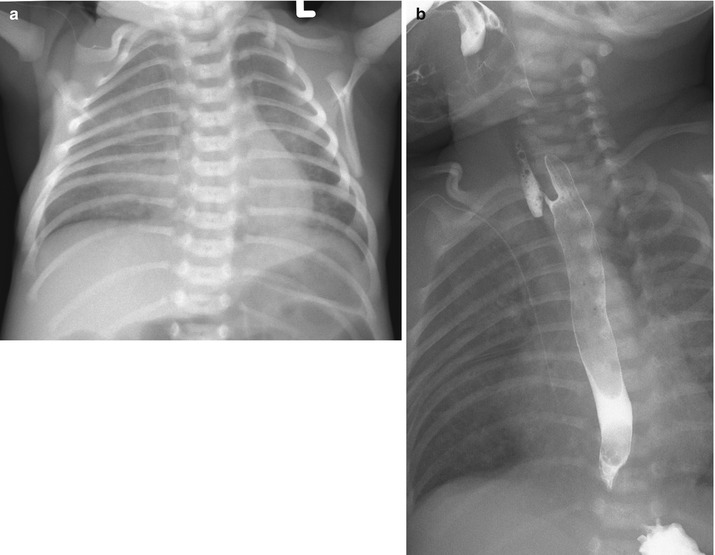
Fig. 19.3
H-type tracheoesophageal fistula in a 12-day-old neonate. (a) Chest radiograph shows infiltration in the right lung, which is gradually aggravated after birth. (b) Lateral view of esophagogram confirms a fistulous tract extending from the esophagus anteriorly and cephalad toward the trachea. Note venous catheter tip at the right atrium
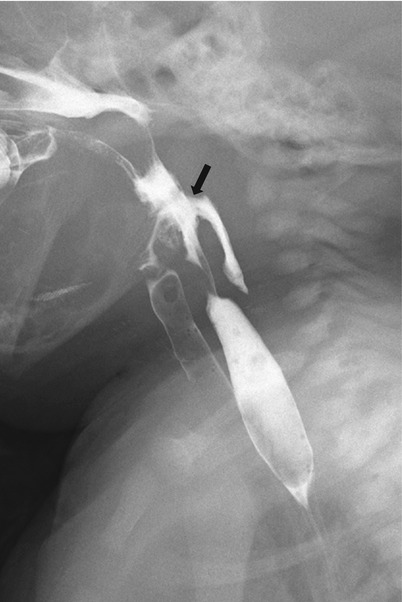
Fig. 19.4
Pharyngoesophageal perforation in a 1-day-old neonate transferred from the outside hospital due to respiratory difficulty. The neonate was intubated after birth and underwent vigorous suctioning. Lateral view of esophagogram confirms a retroesophageal blind-ending tract from the hypopharynx, as pharyngeal pseudodiverticulum (arrow)
19.6.2 Laryngoesophageal Clefts
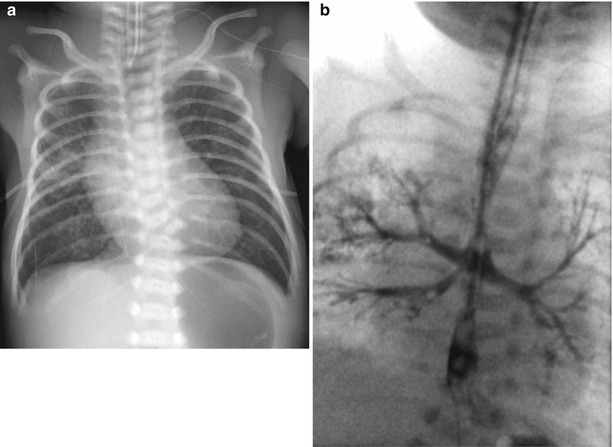
Fig. 19.5
Persistent esophagotrachea in a premature with progressive desaturation and prenatal US diagnosis of esophageal atresia. (a) Chest radiograph on 4 days of life demonstrates infiltrations in both lung fields and a tubular-shaped hyperlucency over the cervical and upper thoracic vertebrae. Note segmentation anomaly of the lower thoracic vertebrae. (b) Esophagogram shows a common lumen with both nasogastric and endotracheal tubes inserted. Note bronchial bifurcation from the distal one-third of a common lumen, which is distally continued to the esophagus
19.6.3 Congenital Esophageal Stenosis
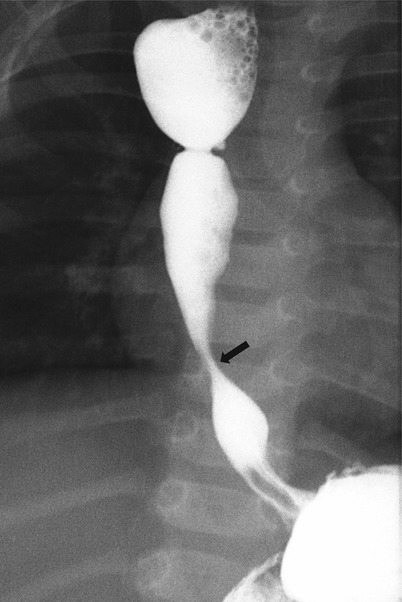
Fig. 19.6
Congenital esophageal stenosis in a 6-month-old girl with history of surgical repair of esophageal atresia. Frontal view of the esophagram demonstrates focal concentric narrowing (arrow) of the distal third of the esophagus. Note residual deformity at the proximal esophagus indicating the site of the anastomosis
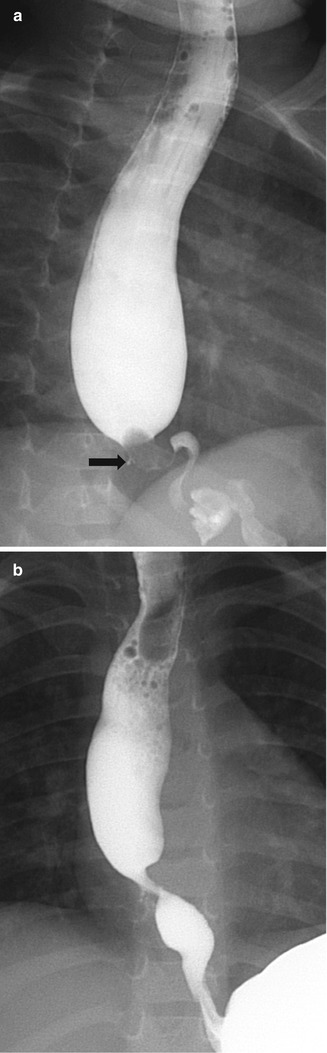
Fig. 19.7
Congenital esophageal stenosis in a 20-month-old girl with sudden onset of choking. (a) Oblique view of the esophagram demonstrates an ovoid radiolucent filling defect impacted in the distal third of the esophagus and small barium projection (arrow) along the right lateral border of the filling defect. (b) Esophagogram after endoscopic removal of a bean shows focal narrowing at the distal esophagus and clearer demonstration of barium-filled diverticulum-like structure, representing characteristic of cartilaginous tracheobronchial remnants
19.6.4 Gastric Volvulus
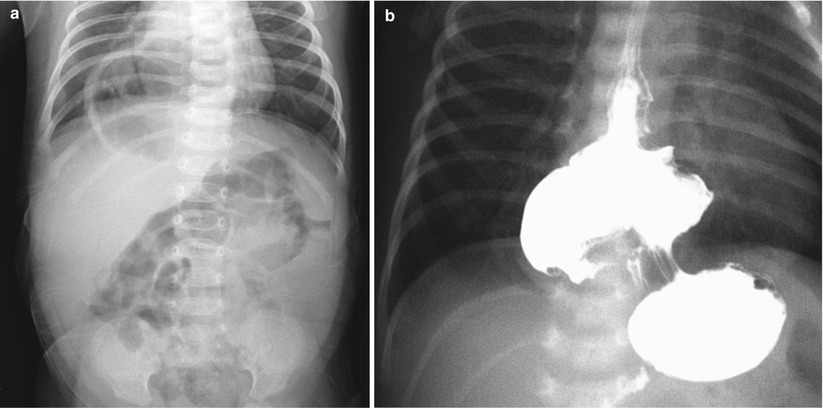
Fig. 19.8
Organoaxial volvulus in a 12-day-old neonate with hiatal hernia. (a) Plain radiograph shows air-filled structure with an unusual configuration in the retrocardiac and right paravertebral areas. (b) Image from UGI study demonstrates partial herniation of the stomach with inferiorly pointed pylorus. The greater curvature lies to the right of and superior to the lesser curvature
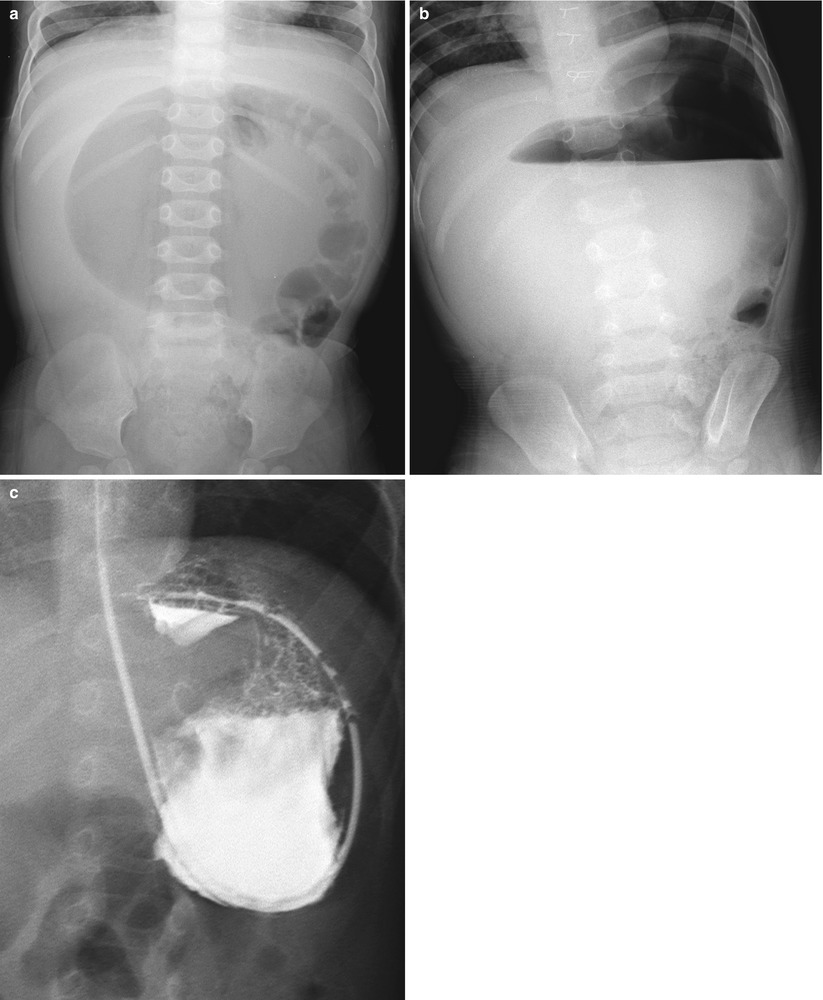
Fig. 19.9
Mesenteroaxial volvulus in a 11-month-old girl with abdominal distension and vomiting. Supine (a) and erect (b) abdominal radiographs show a marked spherical distension of the stomach with two air-fluid levels. Note sternal wirings by previous surgery for congenital heart disease. (c) Image from UGI study after gastric decompression shows the antrum and pylorus lying above the fundus with upside-down stomach and pyloric obstruction with beaking. The lesser and greater curvatures maintain their normal relationship. Asplenia was confirmed at surgery
19.6.5 Duodenal Atresia and Stenosis

Fig. 19.10
Duodenal atresia in a 1-day-old premature presented with vomiting. Abdominal radiograph demonstrates a markedly distended stomach and duodenal bulb giving the classic double bubble sign. Note lack of gas in the rest of the intestinal tracts
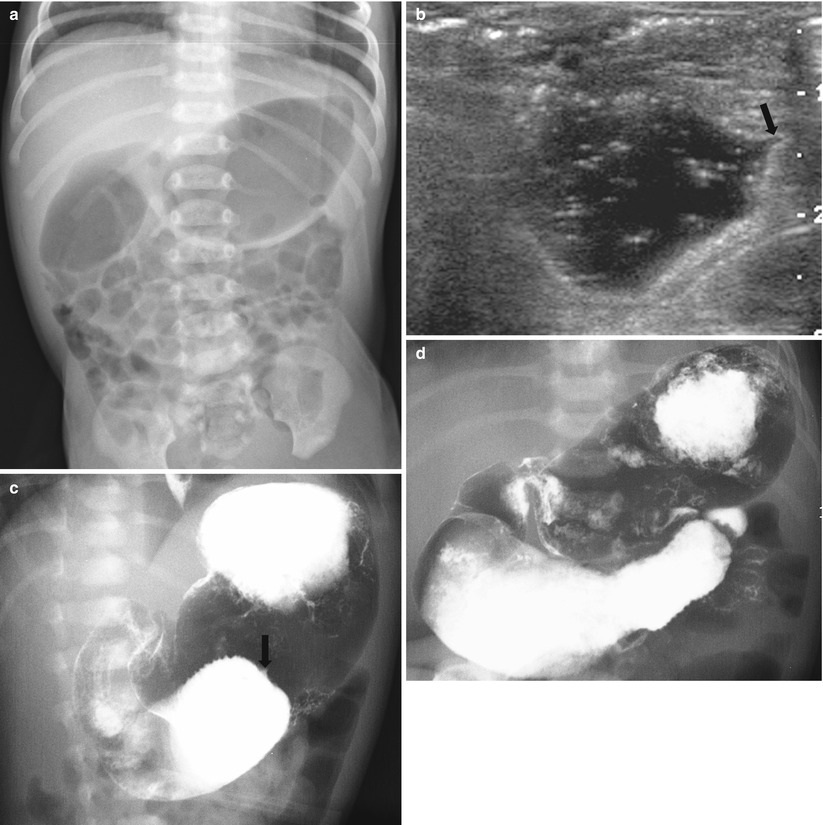
Fig. 19.11
Duodenal stenosis by web in a 4-day-old neonate with bilious vomiting. (a) Abdominal radiograph shows gaseous distension of the duodenum and nondilated scattered gas-filled bowel loops distally. (b) Transverse abdominal US shows the fluid-filled, distended duodenum with a central teat configuration in the obstructed end (arrow). (c) Images from UGI study show the barium passage halting at the third portion of the duodenum, the bolus ending with a central teat configuration (arrow), similar to US finding. (d) Delayed image demonstrates a smooth transverse filling defect crossing the duodenal lumen and passage of barium beyond the lesion. The duodenal web with a pinpoint hole was found at surgery
19.6.6 Midgut Malrotation and Volvulus
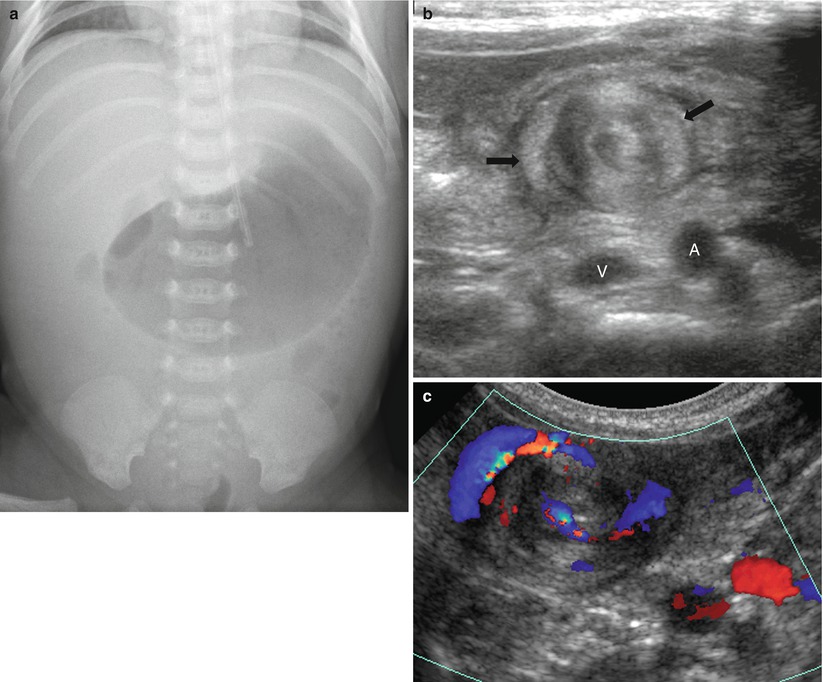
Fig. 19.12




Midgut volvulus with Ladd band in a 1-month-old boy presenting with bilious vomiting. (a) Abdominal radiograph demonstrates the distended stomach and paucity of gas in the remainder of the bowel loops. (b) Transverse US of the upper abdomen shows a whirl-like mass (arrows) in the upper abdomen in front of the vena cava (V) and aorta (A). (c) Corresponding color Doppler study shows a clockwise whirlpool sign with complete wrapping of the superior mesenteric vein, mesentery, and bowel loops around the superior mesenteric artery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree