Congenital Anomalies
Congenital anomalies of the pulmonary vasculature are often asymptomatic but can present in the neonatal period or later in life. The pulmonary artery can be affected by proximal interruption (agenesis, hypoplasia, stenosis) or anomalous origin (pulmonary artery sling, truncus arteriosus). The pulmonary arterial and venous systems can have abnormal connections, as exemplified by arteriovenous malformations. An abnormal systemic artery may supply normal or abnormal lung (intralobar and extralobar sequestration, scimitar syndrome); also, abnormal systemic artery–to–pulmonary vessel shunts can occur. The pulmonary veins can be affected by a partial or total anomalous venous return draining normal or abnormal lung. In this chapter, examples are used to illustrate the numerous varied and interesting congenital anomalies of the pulmonary vasculature.
 Pulmonary Artery Agenesis
Pulmonary Artery Agenesis
 Complete unilateral pulmonary artery agenesis is an uncommon anomaly that occurs on the right more often than the left.
Complete unilateral pulmonary artery agenesis is an uncommon anomaly that occurs on the right more often than the left.
 The affected lung is often hypoplastic and can be absent.
The affected lung is often hypoplastic and can be absent.
 The affected lung is supplied by systemic arterial blood through collaterals, mainly from bronchial arteries but also transpleural branches of the intercostal, internal mammary, subclavian, and innominate arteries.
The affected lung is supplied by systemic arterial blood through collaterals, mainly from bronchial arteries but also transpleural branches of the intercostal, internal mammary, subclavian, and innominate arteries.
 Left pulmonary artery agenesis is often associated with a right aortic arch and other congenital cardiovascular anomalies.
Left pulmonary artery agenesis is often associated with a right aortic arch and other congenital cardiovascular anomalies.
 Some patients remain asymptomatic, but recurrent pulmonary infection, hemoptysis, dyspnea on exertion, and pulmonary hypertension are seen.
Some patients remain asymptomatic, but recurrent pulmonary infection, hemoptysis, dyspnea on exertion, and pulmonary hypertension are seen.
 Imaging typically shows volume loss of the affected hemithorax, with diaphragmatic elevation and mediastinal shift to the affected side (Figs. 2.1, 2.2); the contralateral lung is hyperinflated. Collateral vessels are often seen (Fig. 2.1).
Imaging typically shows volume loss of the affected hemithorax, with diaphragmatic elevation and mediastinal shift to the affected side (Figs. 2.1, 2.2); the contralateral lung is hyperinflated. Collateral vessels are often seen (Fig. 2.1).
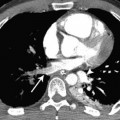
 Partial unilateral pulmonary artery agenesis can also occur (Fig. 2.3).
Partial unilateral pulmonary artery agenesis can also occur (Fig. 2.3).
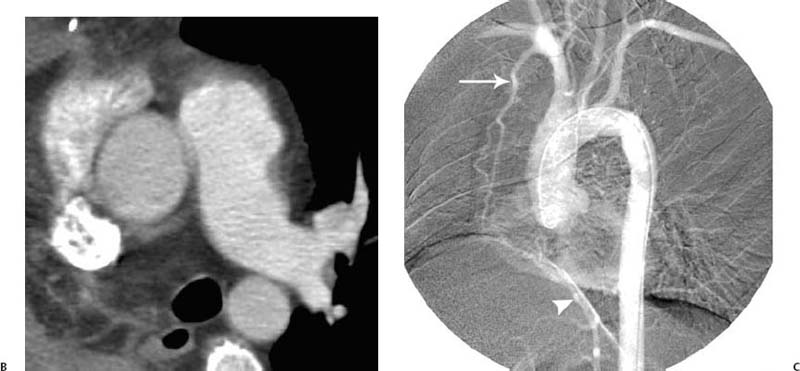
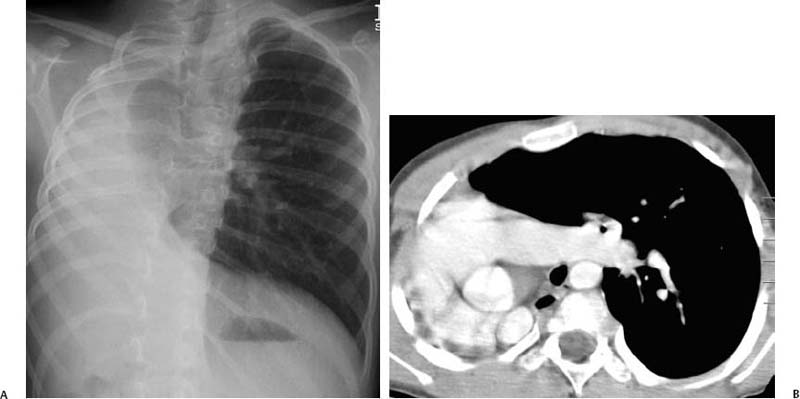
Fig. 2.1 (A–C) Agenesis of the right pulmonary artery in a 38-year-old man. (A) Chest radiograph demonstrates shift of the mediastinum to the right and a hypoplastic right lung with attenuation of the pulmonary vessels on the right. Agenesis of the right pulmonary artery in a 38-year-old man. (B) CT demonstrates agenesis of the right pulmonary artery.
Fig. 2.2 (A,B) Agenesis of the right lung in a 7-year-old boy. (A) Chest radiograph demonstrates complete shift of the mediastinum to the right as the right pulmonary artery and lung did not form. (B) CT shows the heart against the right side of the chest wall and compensatory over-inflation of the left lung.
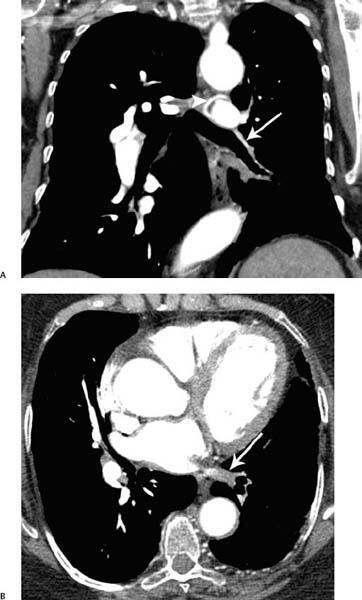
Fig. 2.3 (A,B) Agenesis of the left lower lobe pulmonary artery in a 64-year-old woman. (A) Coronal reformatted CT demonstrates absence of the left lower lobe pulmonary artery (arrow). There are collateral bronchial arteries (arrowhead). (B) A small left inferior pulmonary vein demonstrates poorly opacified pulmonary venous return (arrow).
 Pulmonary Artery Hypoplasia
Pulmonary Artery Hypoplasia
 A unilateral congenital small pulmonary artery usually occurs in association with an ipsilateral congenital small lung (Fig. 2.4) because normal pulmonary blood flow is needed for normal lung development.
A unilateral congenital small pulmonary artery usually occurs in association with an ipsilateral congenital small lung (Fig. 2.4) because normal pulmonary blood flow is needed for normal lung development.
 Bilateral small pulmonary arteries are usually associated with congenital heart disease, particularly tetralogy of Fallot.
Bilateral small pulmonary arteries are usually associated with congenital heart disease, particularly tetralogy of Fallot.
 The morphologic features of tetralogy of Fallot include sub-pulmonary infundibular stenosis, ventricular septal defect, overriding of the aorta, and right ventricular hypertrophy.
The morphologic features of tetralogy of Fallot include sub-pulmonary infundibular stenosis, ventricular septal defect, overriding of the aorta, and right ventricular hypertrophy.
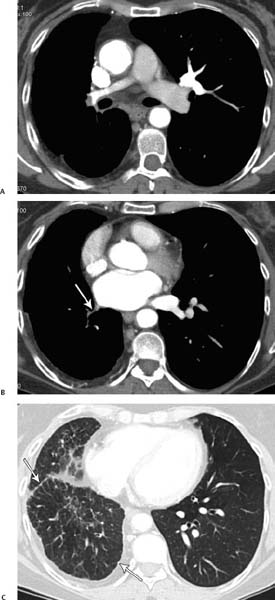
Fig. 2.4 (A–C) Hypoplasia of the pulmonary artery in a 40-year-old woman. (A) CT demonstrates a very small right pulmonary artery in comparison with the left. (B) CT obtained more caudad demonstrates a hypogenic right inferior pulmonary vein (arrow). (C) Lung windows at the level of the lung bases demonstrate nodularity along the pleural margins, likely due to transpleural collateral vessels (arrows).
 Pulmonary Artery Stenosis
Pulmonary Artery Stenosis
 Pulmonary artery stenosis can be associated with other congenital cardiac malformations, as in Williams syndrome, or may occur as a primary isolated condition (Fig. 2.5)
Pulmonary artery stenosis can be associated with other congenital cardiac malformations, as in Williams syndrome, or may occur as a primary isolated condition (Fig. 2.5)
 Left Pulmonary Artery Sling
Left Pulmonary Artery Sling
 An aberrant left pulmonary artery arises from the proximal right pulmonary artery, courses between the trachea and esophagus, and extends to the left hilum (Fig. 2.6).
An aberrant left pulmonary artery arises from the proximal right pulmonary artery, courses between the trachea and esophagus, and extends to the left hilum (Fig. 2.6).
 Affected patients may be classified generally into two groups. Those in one group have a normal bronchial pattern; those in the other have tracheobronchial malformations, including stenosis of a long segment of the trachea or absence of the pars membranacea, as well as cardiovascular abnormalities.
Affected patients may be classified generally into two groups. Those in one group have a normal bronchial pattern; those in the other have tracheobronchial malformations, including stenosis of a long segment of the trachea or absence of the pars membranacea, as well as cardiovascular abnormalities.
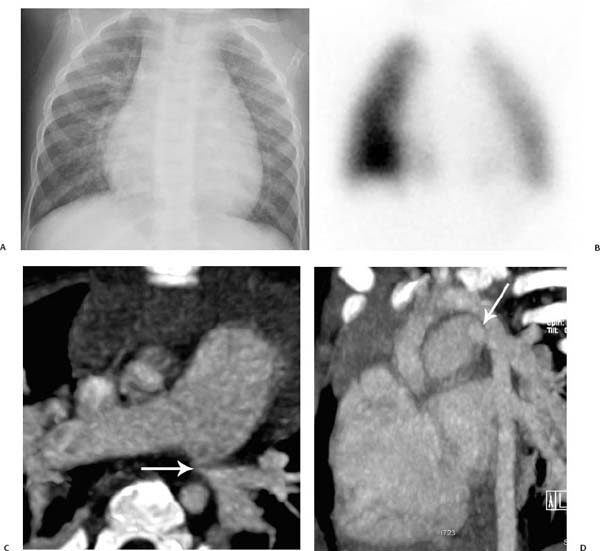
Fig. 2.5 (A–D) Pulmonary artery stenosis in an 18-month-old boy. (A) Chest radiograph demonstrates cardiomegaly as well as plethoric vasculature on the right. (B) Nuclear medicine perfusion scan demonstrates a decrease in perfusion in the left lung. (C) CT demonstrates a left pulmonary artery stenosis (arrow). (D) Sagittal oblique maximum-intensity projection (MIP) CT reconstruction image demonstrates the stenosis at the origin of the left pulmonary artery (arrow).
Fig. 2.6 Pulmonary artery sling in a 45-year-old man. The main pulmonary artery (arrow) passes to the right of the esophagus before dividing into the right and left pulmonary arteries. Lung and pleural changes of congestive heart failure are present.
 Patients with tracheobronchial malformations have high morbidity and mortality rates during infancy.
Patients with tracheobronchial malformations have high morbidity and mortality rates during infancy.
 Patients without tracheobronchial malformations are often asymptomatic. The left pulmonary artery sling can mimic a mediastinal mass on chest radiography.
Patients without tracheobronchial malformations are often asymptomatic. The left pulmonary artery sling can mimic a mediastinal mass on chest radiography.
 Truncus Arteriosus
Truncus Arteriosus
 Truncus arteriosus is a consequence of failure of formation of the spiral septum of the primitive truncus.
Truncus arteriosus is a consequence of failure of formation of the spiral septum of the primitive truncus.
 Affected individuals present with a cyanotic heart lesion and increased pulmonary blood flow in the neonatal period.
Affected individuals present with a cyanotic heart lesion and increased pulmonary blood flow in the neonatal period.
 The single arterial trunk arises from the ventricle via a single arterial valve with two to six cusps and supplies the systemic, pulmonary, and coronary artery circulations.
The single arterial trunk arises from the ventricle via a single arterial valve with two to six cusps and supplies the systemic, pulmonary, and coronary artery circulations.
 All patients have a high ventricular septal defect and 35% have a right aortic arch.
All patients have a high ventricular septal defect and 35% have a right aortic arch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree