Chapter Outline
X-Ray Contrast Agents, 729
Iodinated Contrast Agents, 729
Acute Contrast Reactions, 730
Other Adverse Events Related to Iodinated Contrast, 731
Oral X-Ray Contrast Agents, 732
Magnetic Resonance Imaging Contrast Agents, 733
Classes, 733
Paramagnetic Agents, 735
Special Considerations, 735
Other Agents, 736
Supraparamagnetic Agents, 737
Treatment of Contrast Reactions, 737
X-Ray Contrast Agents
Iodinated Contrast Agents
Classification
Iodinated contrast agents can be classified based on osmolarity (high, low, or iso) and ionitiy (ionic or nonionic).
A variety of iodinated contrast agents have been developed and are distributed by different manufacturers. The agents all consist of iodinated benzene ring derivatives, and ionic agents are typically formulated as sodium and/or meglumine salts. Two generic classes of agents include:
- •
High-osmolar contrast agents (HOCAs, “ionics”)
- •
Low-osmolar contrast agents (LOCAs, “nonionics”); includes iso-osmolar agents
A previously used low-osmolar ionic contrast agent called Hexabrix (ioxaglate) was discontinued in 2015.
| Bayer Healthcare | Urovist | Ultravist |
| Angiovist | ||
| Mallinckrodt | Conray | Optiray |
| Vascoray | ||
| Squibb (Bracco) | Renovue | Isovue |
| Renografin | ||
| Renovist | ||
| GE Healthcare | Hypaque | Omnipaque |
| Visipaque | ||
| Guerbet | Oxilan |
Iodine (I) Content
For nonionic agents, the I content is easy to determine because it is written on the label. For example, Omnipaque 300 contains 300 mg I/mL of solution. For ionic agents, the iodine content has to be calculated because contrast concentrations are expressed on a salt weight basis. For example, Conray 60 contains 60% meglumine iothalamate = 600 mg salt/mL = 282 mg I/mL. Because meglumine and sodium have different molecular weights, a 60% (weight/volume) solution of contrast contains different amounts of iodine, depending on the accompanying cation:
- •
60% meglumine diatrizoate: 282 mg I/mL
- •
60% sodium diatrizoate: 358 mg I/mL
High-Osmolarity Contrast Agents (HOCAs) ( Fig. 13.1 )
There are two major ionic agents on the market, differing in the R-group:
- •
Diatrizoate (i.e., Hypaque)
- •
Iothalamate (i.e., Conray)

The osmolarity of ionic agents depends on the concentration, which typically ranges from 30% (550 milliosmole [mOsm]/kg H 2 O) to 76% (~2000 mOsm/kg H 2 O). The ionic agents have been in clinical use since the 1950s.
Low Osmolarity Contrast Agents (LOCAs) ( Fig. 13.2 )
Nonionic LOCAs have a lower incidence of adverse reactions when used intravenously and are equally effective as imaging agents. Intravascular contrast agents in current use are thus exclusively nonionic LOCAs. The main nonionic agents on the market are:
- •
Iodixanol (Visipaque)
- •
Iopamidol (Isovue)
- •
Ioversol (Optiray)
- •
Iopromide (Ultravist)

Nonionic agents do not require an accompanying cation and therefore have lower osmolarity. The osmolarity depends on the concentration, which typically ranges from 300 mg I/mL (= 670 mOsm/kg H 2 O) to 370 mg I/mL (= 800 mOsm/kg H 2 O).
Pharmacology ( Fig. 13.3 )
Plasma levels of iodinated agents depend on:
- •
Rate of administration (intravenous [IV] bolus, IV drip)
- •
Blood half-life
- •
Distribution
Rapid exchange between plasma and extracellular space
Exclusion from intracellular space
Agents do not cross intact blood-brain barrier.
- •
Excretion
Glomerular filtration with no resorption in
the tubules.
Hepatic excretion (vicarious excretion)
increases in renal failure.

Acute Contrast Reactions
Overview
- •
Frequency of reactions has decreased considerably with the use of modern nonionic LOCAs, with an overall incidence of 0.2%–0.7%.
- •
Acute reactions can be categorized as either allergic like or physiologic and subclassified as mild, moderate, or severe.
- •
A history of allergies or asthma increases the risk of an acute reaction.
- •
No evidence to support a relationship between shellfish/seafood allergy and contrast reaction
Type and Timing of Acute Reactions
- •
Allergic like: typically mediated by type 1 hypersensitivity mechanism, small minority related to immunoglobulin E (IgE) mechanism
- •
Physiologic: results from disruption of homeostasis related to physical/chemical characteristics of the agent such as osmolality and viscosity or from chemotoxicity
- •
Most reactions occur within 1 hour, many within 5 minutes.
- •
Delayed reactions can occur between 1 hour and 1 week after exposure and are typically cutaneous and self-limiting.
Premedication
- •
In patients with a previous contrast reaction, subsequent reactions are most likely to be of a similar severity, though could be either more or less severe.
- •
Premedication may help reduce mild or moderate reactions, though is not appropriate for patients with severe reactions as there is no proven benefit.
- •
Elective premedication: prednisone 50 mg orally (PO) at 13, 7, and 1 hour before contrast injection, as well as diphenhydramine (Benadryl) 50 mg PO 1 hour before injection
- •
Emergent premedication: methylprednisolone 40 mg or hydrocortisone 200 mg IV every 4 hours until contrast injection, plus diphenhydramine 50 mg IV 1 hour before the injection
| Allergic Like a | Physiologic a | |
|---|---|---|
| Mild |
|
|
| Moderate |
|
|
| Severe |
|
|
a Classification of acute contrast reactions (adapted from ).
Other Adverse Events Related to Iodinated Contrast
Contrast-Induced Nephropathy (CIN)
- •
Decrease in renal function following recent intravascular administration of iodinated contrast
- •
Usually occurs within 24–48 hours of injection; generally self-limited
- •
Incidence rate is controversial due to contamination of published studies by bias.
- •
Primary risk factor is preexisting renal insufficiency; evidence suggests increased risk of CIN if glomerular filtration rate (GFR) is <30 mL/min.
- •
Can consider prehydration with GFR of 30–45 mL/min; 100 mL/hour for 6–12 hours before and 4–12 hours after contrast injection if inpatient, more rapid volume expansion if outpatient
- •
No proven benefit for pretreatment with N -acetylcysteine or sodium bicarbonate
- •
Patients with anuric end-stage renal disease (ESRD) can receive iodinated contrast with no further potential for damage as kidneys are already nonfunctional.
Contrast Extravasation
- •
Iodinated contrast is toxic to soft tissues and skin.
- •
Serious complications such as compartment syndrome or skin ulceration/necrosis are uncommon but can occur.
- •
Patient should always be evaluated by the radiologist.
- •
Management generally includes elevating the site of injection and applying warm or cold compresses.
- •
Obtain surgical consultation if:
Progressive swelling or pain
Skin blistering or ulceration
Altered tissue perfusion/skin discoloration
Change in sensation distal to site of extravasation
Miscellaneous Considerations
Metformin
- •
Oral antihyperglycemic agent used to treat noninsulin-dependent diabetes mellitus (DM)
- •
Lactic acidosis is a rare complication with a 50% mortality rate that occurs mainly in patients with concomitant renal failure or hepatic dysfunction.
- •
Iodinated contrast agents are only a concern in patients taking metformin if CIN develops.
- •
No need to discontinue metformin before or after iodinated contrast injection in patients with normal renal function.
- •
In patients with chronic kidney disease or acute kidney injury, discontinue metformin for 48 hours after iodinated contrast injection.
Pregnancy
- •
Iodinated contrast crosses the placenta and enters the fetus.
- •
No evidence of mutagenic or teratogenic effects in animals and no documented evidence of harm in humans, though no well-controlled studies have been performed.
- •
Reasonable to administer iodinated contrast in pregnant patients if medically necessary
Breastfeeding
- •
Plasma half-life of IV iodinated contrast media is 2 hours, <1% is excreted into breast milk in the first 24 hours, and <1% ingested by the infant is absorbed from its gastrointestinal (GI) tract.
- •
Expected systemic dose absorbed by infant from breast milk is <0.01% of intravascular dose given to mother.
- •
No evidence of need to stop breastfeeding, though concerned mothers can consider abstaining from breastfeeding for 24 hours by expressing and discarding milk.
Thyroid Scan
- •
Thyroid uptake of 131 I is decreased to about 50% at one week after iodinated contrast injection but normalizes within a few weeks.
- •
If 131 I therapy is planned, iodinated contrast should be avoided for at least a few weeks before therapy.
Oral X-Ray Contrast Agents
Water-Soluble Iodinated Oral Contrast Agents
- •
Gastrografin and Gastroview are HOCAs consisting of a mixture of diatrizoate meglumine and diatrizoate sodium.
- •
ΙV contrast agents (LOCAs) can also be safely administered for use as oral contrast agents; iohexol (Omnipaque) is the only one technically Food and Drug Administration (FDA)–approved for oral use.
- •
Can be used for fluoroscopic and computed tomography (CT) examinations and is preferred to barium in patients suspected of having perforation as water-soluble agents are readily absorbed from interstitial spaces and peritoneal cavity.
- •
Often diluted with water or other beverage at ratio of approximately 1 : 40 for CT examinations to avoid streak artifact.
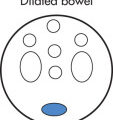
- •
Agents concentrate as they pass distally in the bowel as a result of water absorption, resulting in progressive increase in CT density.
- •
Adverse effects
Chemical pneumonitis if an HOCA is aspirated, though not as much of an issue at diluted concentrations for CT examinations or with LOCAs; avoid undiluted HOCAs for fluoroscopic examinations in patients at risk for aspiration
Diarrhea as a result of fluid loss into bowel from osmotic effect of undiluted HOCAs; pediatric and older adult patients at risk for hypovolemia
Allergic like reactions are theoretically possible since 1%–2% of oral iodinated contrast is absorbed into circulation (higher percentage if mucosa impaired from infection/inflammation), though moderate or severe reactions only very rarely reported; avoid in patients with known IV iodinated contrast allergy
Barium
- •
Micronized barium (BaSO 4 , particle size 5–10 µm) is commonly used to prepare different barium products such as:
“Thin barium” (e.g., EZ-Jug) for upper GI studies, small bowel (SB) follow-through, barium enema (BE): 40% weight per weight (w/w) BaSO 4 solution
“Thick barium” (e.g., EZ-HD) for double contrast studies: 85% w/w BaSO 4 solution
CT barium (e.g., Readicat): 1.2% w/w BaSO 4 solution, 450-mL bottles
- •
Typical additives to barium suspensions include: agents to prevent flocculation (clumping), antifoam agents, osmotically active sugars (sorbitol), sweetening/flavoring/coloring to improve palatability, preservatives such as potassium sorbate and sodium benzoate, and tannic acid, an astringent that precipitates proteins and results in improved mucosal coating
- •
Adverse effects
Relatively contraindicated if suspected perforation, as intraperitoneal or mediastinal extravasation in the setting of perforation can result in extensive fibrosis
Exacerbation of GI obstruction above a preexisting large bowel obstruction (but not SB obstruction)
Aspiration is less of an issue since barium is relatively inert; relevant with large-volume aspiration or in patients with preexisting lung disease who have impaired ciliary clearance
Significant allergic like reactions to barium are exceedingly rare but possible; moderate to severe reactions in 1 out of 2.5 million exposures
Negative Oral Contrast Agents
- •
Increasingly used in CT enterography for evaluation of inflammatory bowel disease (IBD) by increasing conspicuity of the hyperenhancing mucosa and wall against a low density luminal agent
- •
Also useful in assessing for GI bleeding and mesenteric ischemia
- •
VoLumen is the preferred agent and contains a very small amount of barium (0.1%) as well as sorbitol to limit reabsorption of water, resulting in a CT attenuation of approximately 20 Hounsfield units (HU); other options include methylcellulose solutions, polyethylene glycol (PEG), and lactulose
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree