Chapter Outline
Techniques, 512
General, 512
Hardware, 514
Pharmacologic Manipulation, 516
Angiographic Interventions, 516
Thrombolysis, 517
Angioplasty, 518
Venous Access, 521
Vascular US, 521
Magnetic Resonance Imaging, 522
Other Techniques, 523
Conscious Sedation, 523
Coagulation, 524
Antibiotics, 525
Thoracic Aorta and Great Vessels, 525
General, 525
Thoracic Aortic Aneurysm, 526
Aortic Dissection, 528
Traumatic Aortic Injury, 531
Aortitis, 532
Abdomen and Pelvis, 532
Inferior Vena Cava, 532
Abdominal Aorta, 533
Aortic Interventions and Surgery, 535
Mesenteric Vessels, 536
Liver, 541
Kidneys, 543
Spleen, 546
Chest, 546
General Anatomy, 546
Angiographic Techniques, 547
Pulmonary Thromboembolism, 548
Other Pulmonary Vascular Diseases, 549
Extremities, 550
Differential Diagnosis, 558
Techniques
General
Preprocedure Evaluation
- 1.
What is the indication for the procedure?
- •
Diagnosis
- •
Preoperative staging
- •
Therapy
- •
- 2.
Define the problem.
- •
What is the diagnostic question that is to be answered?
- •
Which study can best answer the question (ultrasound [US], computed tomography [CT], magnetic resonance imaging [MRI], angiography)?
- •
- 3.
Patient history, interview, examination
- •
Review chart
- •
Key data: signs and symptoms
Previous vascular surgery/interventions
Previous studies
Laboratory values
Other medical illnesses
Pulse examination
- •
Explanation of the procedure to the patient
- •
Obtain informed consent
- •
- 4.
Assess risk versus benefit (there are no absolute contraindications to angiography).
- •
Approach and access
- •
Coagulopathy?
- •
Renal insufficiency?
- •
What are alternative options?
- •
- 5.
Preprocedural orders
- •
Appropriate laboratory samples drawn (i.e., prothrombin time [PT]/partial thromboplastin time [PTT])?
- •
Appropriate medication withheld (i.e., Coumadin [warfarin])?
- •
Intravenous (IV) access present?
- •
Hydration
- •
Clear liquids only
- •
Premedication if necessary
- •
- 1.
Access
Types of Arterial Approach
- •
Right femoral artery
- •
Left femoral artery
- •
Left axillary artery
- •
Right axillary artery
- •
Translumbar aorta
- •
Brachial arteries
- •
Antegrade femoral artery
- •
Through a surgical graft
- •
Right Femoral Approach (Preferred)
- •
Easily accessible for manipulations and hemostasis
- •
Large-caliber vessel
- •
Well-defined landmarks exist.
- •
Most angiographers are right-handed.
- •
Low complication rate compared with other approaches
- •
Standard Femoral Approach: Seldinger Technique
- •
Double-wall technique is preferred.
- •
Advantages of “single-wall” puncture are only theoretical.
- •
Use fluoroscopy to determine puncture level.
Artery entry: midfemoral head
Skin entry: inferior margin of femoral head
- •
Local anesthesia at skin entry site: 1%–2% lidocaine
- •
Palpate artery above site
- •
Advance 18-gauge Seldinger needle (45–60 degree angle) to bone.
- •
Remove central stylet and withdraw slowly.
- •
Advance guidewire through needle while good pulsatile flow jets out of the hub.
- •
Always use fluoroscope when advancing a guidewire.
- •
Never advance guidewire against resistance.
- •
Exchange needle over wire for dilator or catheter.
- •
Advantage of Puncturing Symptomatic Extremity
- •
Inflow can be assessed by obtaining pull-down pressures.
- •
Should complications arise (i.e., emboli, thrombosis), they will affect the already compromised extremity.
- •
Conversion to antegrade approach is possible if necessary.
- •
Disadvantage of Puncturing Symptomatic Extremity
- •
May interfere with surgical procedure if complication develops (e.g., hematoma)
- •
If a severe stenosis is present, a catheter may obturate the vessel completely.
- •
Axillary Artery Approach
- •
Main indication for this approach is nonpalpable femoral pulses (i.e., aortic occlusion)
- •
Left-sided approach is preferred.
Easier to access descending aorta
Left-sided approach crosses fewer central nervous system (CNS) arteries.
- •
3J wire is preferred.
- •
Disadvantages:
Difficult to compress
Relatively high incidence of complications (e.g., stroke, bleeding, thrombosis)
Brachial plexus injury
- •
Always check for blood pressure (BP) differential to detect occult arterial disease.
- •
Translumbar Approach (TLA)
- •
Main indication for this approach is nonpalpable peripheral pulses.
- •
High TLA is preferred: above abdominal aortic aneurysm (AAA), grafts, diseased distal aorta
- •
Disadvantages:
Patient must lie prone for entire study.
Higher incidence of bleeding (debatable)
More difficult to manipulate catheters
- •
Use an 18-gauge needle/sheath system
- •
Antegrade Femoral Approach
- •
The main indication for this approach is a distal extremity intervention (e.g., percutaneous transluminal angioplasty [PTA] of the superficial femoral artery [SFA]).
- •
Retrograde catheterization may be converted to antegrade access with a Simmons 1 catheter and a 3J or angled guidewire.
- •
Difficult to manage in obese patients
- •
Angiography Complications
There are four types of complication:
- •
Puncture site complications (e.g., groin hematoma)
- •
Contrast agent complications (e.g., anaphylactoid reaction)
- •
Catheter-related complications (e.g., vessel dissection)
- •
Therapy-related complications (e.g., CNS bleeding during thrombolysis)
- •
Problems with the puncture site and contrast media are the most frequent complications during angiography. Puncture site problems depend on coagulation status, size of catheter, patient body habitus, and compliance issues. The overall incidence of death related to angiography is very low (<0.05%).
Puncture Site Complications
- •
Minor hematoma, >5%
- •
Major hematoma that requires surgical therapy, <0.5%
- •
Arteriovenous fistula (AVF), 0.05%
- •
Pseudoaneurysm, 0.01%
- •
Vessel thrombosis, 0.1%
- •
Neuritis
- •
Infection
- •
Contrast Complications (see Chapter 13 )
- •
Renal failure
- •
Cardiac failure
- •
Phlebitis (venography)
- •
Anaphylactoid reactions (rare with arteriography)
- •
Catheter-Related Complications
- •
Cholesterol emboli
- •
Thromboembolism
- •
Cerebrovascular accident (CVA)
- •
Arterial dissection
- •
Pearls
- •
Complications can be limited by:
Careful preangiography assessment (e.g., correct coagulopathies)
Appropriate approach (e.g., history and pulse examination)
Good technique (e.g., trained angiographer)
- •
Risk factors for development of AVF or pseudoaneurysm:
Low puncture
Heparinization
Large catheters
- •
Most puncture site complications can be prevented by good manual compression and correction of coagulopathies before angiography.
- •
Always reassess patient after the procedure.
- •
Hardware
Catheters
Generic Types
Diagnostic catheters
- •
High-flow catheters with side holes are used for central vessels (>10 mL/s).
- •
Low-flow catheters with end holes are used for selective arterial work.
- •
Therapeutic catheters
- •
Balloon catheters (percutaneous transluminal angioplasty [PTA] and balloon occlusion)
- •
Atherectomy catheters
- •
Coaxial infusion catheters
- •
Embolization catheters
- •
Measurements
- •
Outer diameter (OD): catheter size is determined by the OD and given in “French” size. French (Fr) = the circumference in millimeters. Divide French size by 3 to obtain OD in millimeters.
- •
Inner diameter (ID): measured in 1/1000 of an inch
- •
Length: measured in centimeters. 65 cm is commonly used for abdominal studies. 100 cm is usually used for arch and carotid studies.
- •
| Location | Catheter | Injection a | Comments |
|---|---|---|---|
| Thoracic aorta | Pigtail | 25/50 | |
| Abdominal aorta | Pigtail/tip occluded straight | 20/40 | Tip occluded straight catheter for iliac pressures |
| Celiac | C2, S2 | 5/50 | Variations in anatomy common |
| Renals | C2, S2 | 4/8 | Multiple vessels in 25% |
| SMA | C2, S2 | 5/50 | IA tolazoline (Priscoline) for venous phase |
| CT portography | In SMA | 3/120 | Helical CT |
| IMA | S2, C2 | 3/30 | |
| Splenic | Variable | 5/50 | Good splenic vein opacification |
| Hepatic | Variable | 5/50 | Dual (artery, portal) blood supply; variable anatomy |
| Aortic bifurcation/pelvic | Pigtail | 10/20 | Position above bifurcation |
| Internal iliac | C2, S2 | 5/25 | |
| One leg runoff | Straight tip | 4/48 | Positioned in external iliac |
| Two leg runoff | Pigtail | 6/72 | Position above bifurcation |
| Arm | H1 | Variable | LOCA (reduces pain) |
| IVC | Pigtail | 20/30 | |
| Pulmonary | Pigtail | 20/40 | |
| Aortic arch | Pigtail | 30/60 | Higher injections in young patients |
| CCA | Davis A1 | 8/10 | 60% HOCA or LOCA |
| ICA | Davis A1 | 6/8 | 60% HOCA or LOCA |
| ECA | Davis A1 | 2/4 | 60% HOCA or LOCA |
| Vertebral | Davis A1 | 6/8 | 60% HOCA or LOCA |
| Coronary | Judkins | 4/8 | LOCA |
Materials
- •
Thermoplastic materials (polyurethane and polyethylene) are very commonly used for catheter manufacturing.
- •
Nylon: combined with polyurethane to manufacture high-flow, small French catheters
- •
Teflon: very stiff, low-friction material
- •
Braided catheters: internal wire mesh improves torquability.
- •
Pearls
- •
Rate and volume of contrast are reduced for digital subtraction angiography.
- •
Rate and volume always depend on rate of blood flow and size of vessel observed under fluoroscopy.
- •
Shorter catheters allow for higher flow rates and easier exchangeability.
- •
The larger the ID, the better the flow dynamics.
- •
It is good practice to size catheters, sheaths, and wires before their use; considerable discrepancy of dimensions may occur (variable among manufacturers).
- •
Maximum flow rate and pressure tolerance of catheters are specified by manufacturer on package or insert.
- •
Guidewires
All nonspecialty guidewires have a similar construction:
- •
Central stiff steel core with a distal taper
- •
Wire coil spring wound around core
- •
Thin filamentous safety wire holding the other two components together
- •
Most wires are coated with Teflon to decrease friction.
- •
Measurements
- •
Length: 145 cm is the standard length and allows exchanges of 65-cm catheters. “Exchange length” wires are 220–250 cm in length and are used for long catheters.
- •
OD: guidewires are designated by OD in 1/1000 of an inch: 0.018–0.038 is the most common size range.
- •
J tip: refers to the radius of wire curvature in millimeters (i.e., a 3J wire has a 3-mm distal curvature)
- •
| Wire | Major Use/Comments |
|---|---|
| 3J | Tortuous and diseased vessels, avoids selecting branch vessels |
| 15J | Large vessels: femoral, aorta, IVC |
| Straight wire | Dissection is more common |
| Rosen | Exchanges/PTA |
| Amplatz stiff | Exchanges, tortuous iliac arteries |
| Bentson | Long, flexible taper (floppy end) |
| Terumo | Slippery hydrophilic coating; glides well, torque guide |
Pharmacologic Manipulation
| Dosage a | Use | Comments | |
|---|---|---|---|
| Vasodilator | |||
| Nitroglycerin | 50–300 µg | Peripheral spasm | Direct muscle relaxant |
| Verapamil | 1–10 mg in 10 mL saline | Peripheral spasm | Calcium channel blocker; More potent, longer acting than nitroglycerin |
| Vasoconstrictor | |||
| Vasopressin (Pitressin) | 0.2–0.4 U/min | GI bleeding | Contraindication: CAD, HTN, arrhythmias |
a See manufacturer’s package insert for specific rates of administration.
Angiographic Interventions
Embolization
Indication
Hemorrhage
- •
Gastrointestinal (GI) bleeding
- •
Varices
- •
Traumatic organ injury
- •
Bronchial artery hemorrhage
- •
Tumors
- •
Postoperative bleeding
- •
Vascular lesions
- •
Arteriovenous malformation (AVM) or fistula (AVF)
- •
Pseudoaneurysms
- •
Preoperative devascularization
- •
Renal cell carcinoma (RCC)
- •
AVM
- •
Vascular bone metastases
- •
Other
- •
Hypersplenism
- •
Gonadal varices
- •
Hepatic chemoembolization
- •
General Principles
- •
Proximal occlusion is equivalent to surgical ligation. It does not compromise collateral flow. For this reason, it may be ineffective to control bleeding if collaterals continue to supply the bleeding site.
- •
Distal embolization usually infarcts tissue and is followed by necrosis.
- •
Temporary versus permanent embolization: tumors, vascular lesions, varices, and preoperative embolizations are usually permanent occlusions. GI bleeding is best treated with Gelfoam at first (if vasopressin has failed).
- •
Be as selective as possible (i.e., use tracker catheter).
- •
Prevent reflux of embolic material into other vessels.
- •
Document preangiographic and postangiographic appearance.
- •
Embolic Agents
Temporary
- •
Surgical gelatin (Gelfoam): not U.S. Food and Drug Administration (FDA)–approved for embolization. Pledgets are cut to size or occlude large vessels; Gelfoam powder occludes distal vessels and causes infarction.
- •
Permanent
- •
Steel coils of variable sizes are commercially available; coils obstruct proximal vessels.
- •
Microcoils (platinum) are used to occlude more distal vessels.
- •
Detachable balloons are used for large vessel occlusion. FDA restricted. Useful for pulmonary AVF, carotid cavernous fistula (CCF).
- •
Polyvinyl alcohol (Ivalon): small particles for distal occlusion. 200–1000 µm. Suspend in albumin–contrast agent mixture.
- •
Absolute ethanol: causes tissue necrosis. Used with proximal balloon occlusion to minimize shunting and reflux. Useful for solid organ necrosis (i.e., malignant tumors).
- •
Plastic polymers: glue, tissue adhesives
- •
| Material | Occlusion | Primary Use |
|---|---|---|
| Temporary Agents | ||
| Autologous blood clot | 6–12 hr | Rarely used currently |
| Gelfoam | Weeks | Upper GI, hemorrhage, pelvic, trauma |
| Permanent Agents | ||
| Ethyl alcohol (1 mL/kg) | Permanent | Tumors (causes coagulative necrosis) |
| Steel/platinum coils | Permanent | Large vessel, aneurysm, tumor |
| Polyvinyl alcohol (200–1000 m) | Permanent | Tumors |
| Tris-acryl gelatin microspheres (embospheres) | Permanent | Uterine embolization |
| Balloons | Permanent | High-output AVF |
| Cyanoacrylate (glue) | Permanent | AVM |
Complications
- •
Postembolization syndrome (fever, elevated white blood cell [WBC] count), 40%
- •
Infection of embolized area (administer prophylactic antibiotics)
- •
Reflux of embolic material (nontarget embolization)
- •
Alcohol causes skin, nerve, and muscle infarction if used in the periphery; its use should be restricted to parenchymal organs.
- •
Hepatic Chemoembolization
- •
Palliative only; prolonged survival or relief of endocrine symptoms
- •
Dual hepatic/portal supply allows for arterial embolotherapy
- •
Agents: Gelfoam or Ethiodol mixed with chemotherapeutic agents; drug-eluting microspheres
- •
Tumors: hepatocellular carcinoma (HCC), ocular melanoma, metastatic endocrine tumors
- •
Hepatic Radioembolization
- •
Ytrium-90 (Y-90) radioembolization of hepatic artery (HA) is an effective treatment for unresectable HCC. It is a form of brachytherapy.
- •
Y-90 is a pure beta emitter with a short half-life (64 hr). The size of the microspheres ranges between 20 and 40 µm (sufficient for local trapping).
- •
Basic requirements
Absent surgical or ablative options
Absent other conventional treatment options
Preserved liver function
Adequate general condition
Liver dominant tumor burden
Life expectancy >3 months
- •
Thrombolysis
Indication
- •
Arterial graft thrombosis
- •
Native vessel acute thrombosis
- •
Before percutaneous intervention
- •
Hemodialysis AVF or graft
- •
Venous thrombosis
Axillosubclavian
Portal vein (PV), superior mesenteric vein (SMV)
Inferior vena cava (IVC)
- •
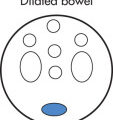
General Principles ( Fig. 8.1 )
- •
Always obtain a diagnostic angiogram before thrombolysis.
- •
Streptokinase is no longer used (antigenic side effects).
- •
Recombinant tissue plasminogen activator (r-tPA) is no more effective than urokinase (UK) but is much more expensive.
- •
Favorable prognostic factors for thrombolysis:
Recent clot (<3 months)
Good inflow/outflow
Positioned in thrombus
- •
End points of thrombolytic therapy:
No lysis present after 12 hours of infusion
Major complication develops
Severe reperfusion syndrome
Progression to irreversible ischemia
- •
Successful thrombolysis is defined as:
>95% lysis of thrombus
Clinical reperfusion
- •
Always treat underlying lesions.
- •
Overall success:
Grafts, 90%
Native arteries, 75%
- •
Heparinize concomitant with UK infusion
- •
Monitor in intensive care unit (ICU)
- •
No good correlation among success, complications, and blood tests
- •
| SK | UK | r-tPA | |
|---|---|---|---|
| Source | Streptococcus culture | Renal cell culture | DNA technology |
| Dosage | 5000 U/hr | 100,000 U/hr | 0.001–0.02 mg/kg per hr a |
| Half-life | 20 min | 10 min | 5 min |
| Treatment time | 24–48 hr | 24 hr | 6 hr |
| Bleeding cost | 20% | 10% | 10% |
| Cost | Inexpensive | Expensive | Very expensive |
a Dosage not to exceed 10 mg for a single bolus; total dose should be <40 mg.

Techniques
Low-dose technique (constant)
- •
100,000 U/hr of UK
- •
Repeat angiogram after 12 hours
- •
High-dose technique (graded)
- •
250,000 U/hr × 4 hours of UK
- •
Repeat angiogram and then 125,000 U/hr
- •
Pulse spray ultrahigh dose
- •
600,000 U/hr in 5000 U of UK bolus doses
- •
Aliquots every 30 s
- •
Catheter placement
- •
Coaxial dual infusion is best.
- •
5-Fr catheter lodged in proximal thrombus
- •
T3 or infusion wire (Katzen) coaxially into distal thrombus
- •
Split infusion of UK into proximal and distal catheters
- •
Secure skin entry site
- •
Tissue plasminogen activator (tPA) infusion
- •
tPA (arterial): infuse at 1 mg/hr total dose divided among infusion sites. Total maximum dose per patient is 100 mg. tPA has half-life of 6 min.
- •
tPA (venous): same infusion rate as arterial, lower bleeding complication rate
- •
tPA (line clearance): 0.5 mg/hr × 3–4 hours
- •
Contraindications
Absolute
- •
Active bleeding
- •
Intracranial lesion (stroke, tumor, recent surgery)
- •
Pregnancy
- •
Nonviable limb
- •
Revascularization of nonviable limb will cause acute renal failure and cardiovascular collapse because of lactic acid and myoglobin
- •
Infected thrombus
- •
Relative
- •
Bleeding diathesis
- •
Cardiac thrombus
- •
Malignant hypertension (HTN)
- •
Recent major surgery
- •
Postpartum
- •
Complications
- •
Major hemorrhage requiring termination of UK, surgery, or transfusion (e.g., intracranial hemorrhage, massive puncture site bleed), 7%
- •
Minor hemorrhage, 7%
- •
Distal embolization
- •
Pericatheter thrombosis
- •
Overall, termination of therapy is required in 10%.
- •
Angioplasty
PTA is a method to fracture the vascular intima and stretch the media of a vessel by a balloon ( Fig. 8.2 ). Atherosclerotic plaques are very firm and are fractured by PTA. Healing occurs by intimal hyperplasia.

Indication
- •
Claudication or rest pain
- •
Tissue loss
- •
Nonhealing wound
- •
Establish inflow for a distal bypass graft
- •
Hemodialysis AVF or grafts
- •
General Principles
- •
Premedication with aspirin and 10 mg of nifedipine
- •
Ipsilateral approach is preferred.
- •
Heparinize (5000–10,000 U) after the lesion is crossed.
- •
Diagnostic angiogram is obtained before PTA.
- •
Measure pressure gradients with borderline lesions.
- •
Significant gradient >10 mm Hg at rest; >20 mm Hg after vasodilator; >10% systolic BP
- •
Pharmacologic adjuncts
Intraarterial (IA) nitroglycerin or tolazoline for vasospasm and provoked pressure measurements
- •
Balloon size: sized to adjacent normal artery
Common iliac artery: 8–10 mm
External iliac artery: 6–8 mm
Superficial femoral artery (SFA): 4–6 mm
Renal artery: 4–6 mm
Popliteal artery: 3–4 mm
- •
Wire should always remain across lesion
- •
Repeat angiogram and pressure measurements after angioplasty.
- •
Postprocedure heparin with “limited flow” results (dissection, thrombus)
- •
Prognostic Indicators
- •
Large vessels/proximal lesions respond better than small vessel/distal lesions.
- •
Stenoses respond better to PTA than occlusions.
- •
Short stenoses respond better to PTA than long stenoses.
- •
Isolated disease responds better to PTA than multifocal disease.
- •
Poor inflow or poor outflow decreases success.
- •
Limb salvage interventions have a poor prognosis.
- •
Diabetics have a poorer prognosis than nondiabetic patients.
- •
PTA Results
Iliac system
- •
95% initial success
- •
70%–80% 5-year patency
- •
Femoral-popliteal
- •
90% initial success
- •
70% 5-year patency
- •
Renal artery
- •
95% initial success
- •
Fibromuscular dysplasia (FMD): 95% 5-year patency
- •
Atherosclerosis: 70%–90% 5-year patency
- •
Ostial lesions have a poorer prognosis.
- •
Acute failures are due to thrombosis, dissection, or inability to cross a lesion.
Recurrent stenosis
- •
Intimal hyperplasia (3 months–1 year)
- •
Progression of disease elsewhere (>1 year)
- •
Complications
- •
Groin complications (same as diagnostic angiography)
- •
Distal embolism
- •
Arterial rupture (rare)
- •
Renal infarction or failure (with renal PTA)
- •
Intravascular Stents
Metallic stents have an evolving role in interventional angiography. Two major types of stents:
Balloon-expandable stent (Palmaz, Genesis, Omniflex, Herculink, Crown)
- •
Balloon mounted; usually made of nitinol
- •
Placement is precise; shortens slightly
- •
Less flexible (minimal elastic deformation because of hoop strength), limited by balloon size
- •
Should not be placed at sites where extrinsic forces could crush the stent
- •
Thoracic outlet veins
- •
Dialysis graft
- •
Self-expandable (Wallstent, Protégé, Luminex, Symphony, SMART, Dynalink)
- •
Bare; usually made of stainless steel
- •
Placement is less precise; can have large diameters
- •
Considerable elastic deformity (flexible)
- •
Useful in tortuous vessels and tight curves
- •
Gianturco zigzag stent (Cook)
Stent grafts (metallic stents combined with synthetic graft material) are used in aortic aneurysms and dissections (AneuRx, Ancure, Gore [descending thoracic] are FDA-approved).
Indications for Metallic Stents
- •
Unsuccessful PTA
- •
Recurrent stenosis
- •
Venous obstruction, thrombosis
- •
Transjugular intrahepatic portosystemic shunt (TIPS)
- •
Indications for Stents in Revascularization Procedures
- •
Long-segment stenosis
- •
Total occlusion
- •
Ineffective or unsuccessful PTA:
Residual stenosis >30%
Residual pressure gradient >5 mm Hg rest, >10 mm Hg posthyperemia
Hard, calcified plaque
Large post-PTA dissection flap
- •
Recurrent stenosis after PTA
- •
Ulcerated plaque
- •
Renal ostial lesions
- •
Stent Results
- •
Iliac artery: over 90% 5-year patency (better than PTA)
- •
Renal artery and other vessels: limited long-term data
- •
Transjugular Intrahepatic Portosystemic Shunt (Tips)
Established Indications
- •
Portal HTN with variceal bleeding that has failed endoscopic treatment
- •
Refractory ascites
- •
Hepatic pleural effusion (hydrothorax)
- •
Controversial Indications
- •
Budd-Chiari syndrome
- •
Pretransplant
- •
Hepatorenal syndrome
- •
Venoocclusive disease
- •
General Principles
- •
Confirm PV patency before procedure (US, CT, or angiography).
- •
Preprocedure paracentesis may be helpful.
- •
Right internal jugular vein (RIJV) is the preferred access vessel.
- •
Goal: portosystemic gradient <10 mm Hg, decompression of varices
- •
Contraindications
- •
Absolute
Severe right-sided heart failure with elevated central venous pressure
Severe polycystic liver disease
Uncontrolled systemic infection or sepsis
Liver abscess
Unrelieved biliary obstruction
Portal HTN from arterioportal fistula
- •
Relative
Severe encephalopathy
PV thrombosis
Hepatic vein obstruction/thrombosis
Severe coagulopathy (INR >5)
Thrombocytopenia (<20,000/cm 3 )
Moderate pulmonary HTN
Severe stenosis or occlusion of celiac or HA
Large liver hypervascular tumor (hepatoma)
Severe liver failure (TIPS have unclear survival benefit)
- •
Technique ( Fig. 8.3 )
- •
RIJV approach
- •
Obtain wedged hepatic pressure and venogram
- •
Create tract from right hepatic vein to PV with 16-gauge needle
- •
Advance catheter over wire into portal venous system
- •
Obtain portal venogram
- •
Measure portal pressures
- •
Dilate tract with PTA balloon (8 mm)
- •
Deploy metallic stent (Palmaz or Wallstent) or stent graft
- •
Dilate stent until gradient <10 mm Hg
- •
Coil embolization of varices optional
- •

Results
- •
Patency: 50% at 1 year
- •
Recurrent bleeding in 10%
- •
Complications
- •
Hepatic encephalopathy 10%; more likely when residual gradient is <10 mm Hg
- •
Bleeding
- •
Shunt thrombosis or stenosis
- •
Right-sided heart failure
- •
Renal failure
- •
Signs of Malfunction
- •
No flow
- •
Low-velocity flow (<50–60 cm/s) at portal venous end of shunt
- •
Reversal of flow in hepatic vein away from IVC
- •
Hepatopedal flow in intrahepatic PV
- •
Reaccumulation of ascites; varices; recanalized umbilical vein
- •
Alternatives to Tips
- •
Direct intrahepatic portocaval shunt (DIPS)–modified TIPS with intravascular US guidance
- •
Balloon-occluded retrograde transvenous obliteration (BRTO)–gastric varices
- •
Partial splenic embolization (PSE)–variceal hemorrhage
- •
These techniques increase portal venous pressure and may result in worsening of untreated varices
- •
Transjugular Liver Biopsy
May be preferred over percutaneous liver biopsy in patients with bleeding disorders and when a hepatic venous pressure gradient (= wedged – free hepatic venous pressure) is desired.
Technique
- •
RIJV approach preferred.
- •
Right hepatic vein is selected with wire/catheter, and sheath advanced.
- •
Core biopsy device (18- to 19-gauge) is advanced into the liver parenchyma.
- •
| Device | Purpose/Situation |
|---|---|
| External tunneled catheter (silicone or polyurethane) | Continuous use, multiple simultaneous uses |
| Implantable port | Intermittent use; immunocompromised patient |
| High-flow catheter | Temporary hemodialysis; pheresis |
| Peripherally inserted central catheter | Short-term use, usually <2–3 months; infrequent blood drawing |
Venous Access
Central Venous Access Catheters
The catheters are typically inserted through axillary (subclavian), internal jugular, or arm vein. Pneumothorax, symptomatic vein stenosis, and thrombotic complications are less common with jugular than subclavian vein approaches. Internal jugular approach preserves subclavian for future fistula/graft. For the axillary vein puncture, the entry site should be lateral to the ribs in the subcoracoid region ( Fig. 8.4 ). This approach eliminates the possibility of pneumothorax and also ensures that the catheter is well within the subclavian vein as it passes through the costoclavicular space. If the catheter is extravascular at this site, chronic compression may occur and lead to catheter erosion and fracture—“pinch-off syndrome.” For IJV puncture, a site on the midneck above the clavicle is selected. The vein is punctured under transverse US guidance, ensuring that the carotid artery is avoided.

Complications of Central Venous Catheter Placement
- •
Pneumothorax
- •
Arterial puncture
- •
Hemorrhage or hematoma
- •
Occlusion
- •
Mechanical problems
- •
Air embolism
This usually occurs when venous dilator is removed from peel-away sheath to be replaced with the catheter. The embolism can be avoided by covering the opening with a gloved finger and removing the dilator with patient in suspended deep inspiration.
If air does get sucked in, perform fluoroscopy of the chest. If there is air in the pulmonary artery (PA) do the following:
- •
Place patient in left lateral decubitus position to keep air in the right chamber.
- •
Suck out air with Swan-Ganz balloon catheter.
- •
Administer supplemental O 2 and monitor patient.
- •
- •
Vascular US
General
Frequency shift = 2 × transducer frequency × velocity of blood × cosine of angle × 1/speed of sound (1540 m/s). Cos of 90 degrees = 0 and cos of 0 degrees = 1. The optimal angle between the probe and the vessel is less than 60 degrees ( Fig. 8.5 ).

Continuous Wave Doppler
- •
Performed with a pencil probe. No static image is produced, as the machine does not stop to listen. If one vessel is located behind the other, one cannot use continuous wave Doppler because it will reveal both waveforms.
- •
Pulsed Wave Doppler
- •
Frequently used for interrogating arteries and veins; duplex Doppler refers to the fact that one gets gray scale and Doppler images.
- •
The operator can set the machine to listen only to those Doppler shifts coming from a particular depth. This is called Doppler gate or sample volume.
- •
Color flow is used to determine the direction of flow (by convention, red is toward the transducer and blue is away), as well as magnitude of shift.
- •
Color machines do not display velocity, because angle of insonation is not used to assign color; the color indicates magnitude of frequency shift. The greater the shift, the lower the saturation of color. In simple terms, in a tortuous vessel the frequency shifts and angle of insonation changes; thus change in color is due to frequency shift even though velocity is the same.
- •
The color image is a display of average frequency shift and not peak frequency shift. Calculations of stenosis from Doppler data are based on peak frequency shift or peak velocity.
- •
Power Doppler US
- •
The signal is related to the number of moving targets (usually red blood cells [RBCs]).
- •
This technique ignores velocity and direction of flow. Used to detect flow and has high sensitivity.
- •
Aliasing
Aliasing is the result of flow velocity exceeding the measuring ability of pulsed wave Doppler. By Doppler imaging, this is seen as a wraparound with high velocity below the bottom of the scale rather than on the top. By color imaging, aliasing becomes evident by inversion of color (blue within an area of red and vice versa). Ways for reducing aliasing:
- •
Pulse repetition frequency (PRF) can be increased by raising the scale.
- •
The Doppler shift can be reduced by manipulating variables of equation, thus either a greater angle (reduced cosθ value) or a lower frequency can be used.
- •
Color aliasing refers to wrapping of signal displayed as areas of color reversal.
- •
Changes because of vessel tortuosity can also change colors, but in that case color changes are marked by a band of black, thus red to blue with black (no signal) in between. Artifacts due to 0 = 90 degrees.
- •
Because the US machine typically only displays either gray scale or color information, there is competition as to which signal is displayed. If the gray scale gain setting is high, the color image is suppressed when flow is low, giving the impression of absent flow or smaller lumen.
- •
Magnetic Resonance Imaging
Noncontrast Imaging Techniques
Two main noncontrast MR angiography (MRA) techniques: time of flight (TOF) MRA and phase contrast (PC) MRA. Both techniques can be acquired in either two dimensions (2D) or three dimensions (3D).
TOF-MRA
- •
Maximizes contrast between flowing blood and stationary tissue; flow-related enhancement repetition interval (TR) < T1
- •
3D has higher signal-to-noise ratio (SNR) and shorter imaging times than 2D.
- •
Works well for high-flow arterial systems
- •
Limitations for imaging: slow flow vessels (especially venous system), tortuous vessels, poor background resolution
- •
PC-MRA
- •
Flowing spins encoded with a bipolar gradient
- •
Velocity encoding gradient setting critical
- •
Speed or flow images
- •
2D good for slow flow
- •
3D has better spatial resolution.
- •
Less saturation effects
- •
Flow velocity information
- •
Longer imaging times
- •
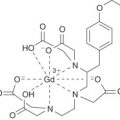
Gadolinium (GD)-Enhanced MRA
A perfectly timed Gd contrast agent injection with 3D spoiled gradient-echo (SPGR) produces high SNR MRA covering extensive regions of vascular anatomy within a breathhold. Compared with noncontrast techniques, signal does not depend on inflow of blood, is not subject to problems of flow saturation, and reduces intravoxel dephasing. The IV-administered Gd shortens the T1 of blood to <270 ms (T1 of fat), so all bright signal essentially originates from vessels. Images are reconstructed as maximum-intensity projections (MIPs). Technique:
- •
Dose: two or three bottles (20 mL each) of the Gd (about 0.3 mmol/kg Gd)
- •
Timing: perfect contrast agent bolus timing is crucial to ensure that the maximum arterial Gd occurs during the middle of the acquisition, when central k-space data are acquired. Begin injecting Gd immediately after starting the scan. Finish the injection just after the midpoint of the MR acquisition. To ensure full use of the entire dose of contrast, flush the IV tubing with 20 mL of normal saline.
- •
Spinal GD MRA
Spinal AVF/AVM is a potentially devastating disease that is often overlooked. MRA can be an excellent screening examination in suspected patients and for preangiographic planning. Patients usually present with pain and weakness of the extremities. On MRI, there is often an abnormal T2-weighted (T2W) signal change in the cord, most commonly near the conus (congestive phenomenon), which can be reversible if the AVF/AVM is treated. Small flow voids can also be seen on T2W sagittal images. MRA protocol:
- •
Acquire MRA in the coronal plane unless there is extensive scoliosis; then, the sagittal plane is preferred.
- •
Timing run: axial image, one slice centered on the aorta at L2; 2 mL of Gd bolus (usually about 17 s)
- •
Acquisition: 30 mL of contrast followed by 30 mL of saline push with number of averages (NEX) = 1 (no repetition) to ensure arterial phase
- •
Look for early enhancing tortuous venous structures, usually posterior to the spinal cord.
- •
| Technique | Application |
|---|---|
| Multiplanar reformation | Routine |
| MIP | Overall survey; identify areas of further interest |
| Targeted MIP | Isolate vessel of interest; reduce background signal |
| Curved reformations | Obtain vessel measurements |
| Shaded surface display | Convey depth perception |
| Volume rendering | Convey anatomic relationship |
| Subtraction | Eliminate background; produce pure venous images |
Other Techniques
Digital Subtraction Angiography (DSA)
Venous DSA
- •
Catheter in central venous structure; a combined large volume and high concentration of contrast agent is given as a bolus.
- •
Adequate results in only 70% of patients
- •
Invasive study
- •
Arterial DSA
- •
Advantages: lower iodine concentration required than that for cut radiograph, less pain, speedy
- •
Disadvantages: less resolution, motion, and bowel gas artifacts
- •
Petrosal Vein Sampling
Venous blood is obtained from bilateral inferior petrosal veins (which drain the cavernous sinus) to detect lateralization of hormones produced by pituitary tumors (very sensitive test). Simultaneous tracker catheters are advanced into the inferior petrosal veins. Simultaneous samples are obtained to distinguish paraneoplastic/endocrine production of hormones from pituitary sources and localize the abnormality to left or right.
Lymphography
- •
Isosulfan blue, 1 mL, injected between 1st–2nd and 4th–5th toes; wait 10 min for lymphatic uptake.
- •
Cutaneous cutdown to the fascia (dorsum of foot)
- •
Isolate a lymphatic; pass a silk suture above and below.
- •
Milk the blue dye into the vessel.
- •
Puncture lymphatic with a 30-gauge needle lymphography set.
- •
Hook up needle to pump and inject oily contrast medium (Ethiodol)
- •
Obtain initial images of lymphatic vascular phase and later of the nodal phase.
- •
Conscious Sedation
Form of sedation in which the patient is given sedation and pain medication but should remain easily arousable. The following parameters are continuously monitored:
- •
BP
- •
Oxygenation using a pulse oximeter
- •
Electrocardiogram (ECG) and heart rate (HR)
- •
Conscious sedation is usually achieved by small aliquot dosing of midazolam and fentanyl.
| IV Dosage | Total Dose | Duration (hr) | Comments | |
|---|---|---|---|---|
| Benzodiazepines | ||||
| Diazepam | 1–5 mg | 10–25 mg | 6–24 | Long-acting |
| Lorazepam | 0.5–2.0 mg | 2–4 mg | 6–16 | |
| Midazolam | 0.5–2.0 mg | <0.15 mg/kg | 1–2 | Good amnesic effect; short-acting |
| Flumazenil | 0.2 mg | May repeat q 1 min up to 1 mg | 0.5–1 | For benzodiazepine reversal |
| Narcotic Analgesics | ||||
| Morphine | 1–5 mg | <0.2 mg/kg | 3–4 | Histamine release |
| Meperidine | 12.5–25 mg | 0.5–1 mg/kg | 2–4 | MAOI interaction |
| Fentanyl | 15–75 µg | 1–3 µg/kg | 0.5–1 | Immediate onset |
| Naloxone | 0.4–0.8 mg | Repeated as needed | 0.3–0.5 | For narcotic overdose |
| Antiemetics | ||||
| Metoclopramide | 10 mg | 0.5–1 mg/kg | 1–2 | Stimulates GI motility |
| Ondansetron | 4 mg | 8 mg | 4–8 | |
| Prochlorperazine | 2.5–10 mg | 10 mg | 4–6 | Adjust dosage for age |
| Promethazine | 12.5–25 mg | 25 mg | 4–6 | CNS depressant effects |
| Droperidol | 0.625–1.25 mg | Higher dose: sedation | 4–6 | Potent antiemetic at low doses |
a See manufacturer’s packet insert for specific rates of administration.
Coagulation
General ( Fig. 8.6 )
- •
Warfarin interferes with vitamin K-dependent synthesis of clotting factors.
- •
Heparin inactivates thrombin by combining with antithrombin III.
- •
PTT is the time required for 1 mL of recalcified whole blood to clot. It therefore reflects the intrinsic clotting axis.
- •
PT is the time required for 1 mL of recalcified whole blood to clot in the presence of thromboplastin (phospholipid extract); it therefore reflects the extrinsic clotting axis.
- •
| Clotting Parameter | Normal Value | Causes of Abnormal Values |
|---|---|---|
| Prothrombin time (extrinsic coagulation system) | <3 s of control | Warfarin, heparin, liver disease |
| Coagulopathy (DIC, thrombolytic therapy) | ||
| Vitamin K deficiency (parenteral nutrition, biliary obstruction, malabsorption, antibiotics) | ||
| PTT (intrinsic coagulation system) | <6 s of control | Lupus anticoagulant |
| Hemophilia | ||
| Bleeding time | <8 min | Platelet count <50,000/mm 3 |
| Qualitative: uremia, NSAIDs, | ||
| von Willebrand disease |

Normalization of Prolonged Coagulation Times
Interventions (biopsy, aspiration, drainage) should not be performed if coagulation times are markedly prolonged (i.e., beyond above values); correction of coagulopathies (see table) can often be achieved in several hours.
| Anticoagulant | PT/PTT | Antidote | Normalization |
|---|---|---|---|
| Heparin | Both prolonged | Stop heparin | 3–6 hr |
| IV protamine titration | Minutes | ||
| Warfarin | Both prolonged | IV vitamin K for 3 doses | Days |
| Fresh frozen plasma | Minutes | ||
| Aspirin | Normal (platelet aggregation reduced) | Platelet concentrates Stop aspirin | Minutes, week |
Monitoring Heparin Therapy
- •
Activated clotting time (ACT) is the method of choice for monitoring heparin therapy.
Preheparin administration: <120 s
Heparin drip: <300 s
Catheter and percutaneous transluminal coronary angioplasty (PTCA): >200 s
Postprocedure/sheath removal: <200 s
- •
Anticoagulation Drugs and Procedures
Heparin
Mechanism of action: Potentiates the action of antithrombin III and thereby inactivates thrombin (as well as activated coagulation factors IX, X, XI, XII, and plasmin) and prevents the conversion of fibrinogen to fibrin; heparin also stimulates release of lipoprotein lipase (lipoprotein lipase hydrolyzes triglycerides to glycerol and free fatty acids). Half-life: 1–2 hours, depending on route. Stop 2 hours before procedure.
Coumadin (Warfarin)
Mechanism of action: Interferes with hepatic synthesis of vitamin K-dependent coagulation factors (II, VII, IX, X). Duration of action is 2–5 days. Stop 4 days before procedure.
Fragmin (Dalteparin)
Low-molecular-weight heparin. Subcutaneous (SC) dose, once daily after the loading dose. Duration: >12 hours; half-life: 2–5 hours. Stop the dose 24 hours before procedure.
Argatroban
Direct thrombin inhibitor, IV infusion; half-life: 39–51 min. Stop 4 hours before procedure.
Arixtra (Fondaparinux)
Factor X inhibitor; half-life: 17–21 hours, SC dose once. Stop 24 hours before procedure.
Plavix (Clopidogrel)
Platelet aggregation inhibitor. Pharmacodynamic/kinetic peak effect: 75 mg/day; bleeding time: 5–6 days. Platelet function: 3–7 days; half-life: ~8 hours. Discontinue 7 days before procedure.
ReoPro (Abciximab)
Glycoprotein IIb/IIIa inhibitor. IV dosage. Pharmacodynamic/kinetic half-life: ~30 min. Platelet function returns to normal 24–48 hours after discontinuation of infusion. Antiplatelet effects can be reversed with platelet transfusions.
Other Antiplatelet Agents
Aspirin, cilostazol, dipyridamole, eptifibatide, ticlopidine, tirofiban. Stop most of the antiplatelet agents 5 days before procedure.
Antibiotics
Recommended
- •
All biliary, renal, and other nonvascular interventions
- •
Stent placements, TIPS, ports
- •
(Chemo)embolizations
- •
Patients with increased risks: endocarditis, transplant
- •
G-tube in patients with head and neck cancer
- •
Solid organ biopsies
- •
Not Recommended
- •
Diagnostic angiography
- •
Vena cava filter
- •
Regular G-tube (nonhead and neck cancer patients)
- •
Simple biopsies: thyroid, subcutaneous
- •
Paracentesis and thoracentesis
- •
| Procedure | Antibiotic |
|---|---|
| All routine procedures | Ampicillin (1 g IV) and gentamicin (80 mg IV or 40 mg IV if creatinine elevated) |
| Ampicillin allergy (low cost) | Clindamycin (Clindacin, 600 mg IV) and gentamicin (80 mg IV or 40 mg IV if creatinine elevated) |
| Ampicillin allergy (higher cost) | Levofloxacin (Levaquin, 500 mg IV or 250 mg if creatinine elevated) |
| Septic patients | Consider adding metronidazole (Flagyl, 500 mg IV) to above combination of ampicillin and gentamicin |
| Tube injection | Levofloxacin (Levaquin, 500 mg PO) |
| G-tube (HN CA) | Cefazolin (Ancef, 1 g, IV) followed by 5 days cephalexin (Keflex 500 mg BID PO) |
| Prostate biopsy | Gentamicin (80 mg IM on day of procedure) and ciprofloxacin (Cipro, 500 mg PO for 7 days including day before procedure) |
| Transplant patients | Piperacillin and tazobactam (Zosyn, 3.375 mg IV) |
| Indwelling catheter and continued resistant growth | Consider giving vancomycin (500 mg IV) instead of gentamicin. Consult resistance tests. |
Thoracic Aorta and Great Vessels
General
Anatomy ( Fig. 8.7 )
- •
The normal ascending aorta is always larger in diameter than the descending aorta.
- •
Branches:
Great vessels
Intercostal arteries
Bronchial arteries
- •
Normal great vessel configuration, 70% (see Fig. 8.7 ). Variants occur in 30%:
Bovine arch, 20%: common origin of brachiocephalic and left common carotid artery (CCA)
Left vertebral artery (LVA) comes off aortic arch (AA) between left CCA and subclavian artery (SA), 5%
Common carotid trunk, 1%
Arteria thyroidea inferior mesenteric artery (IMA) to thyroid isthmus
- •
Intercostal arteries are usually paired from 3rd–11th intercostal spaces; these arteries may give rise to spinal arteries.
- •
Bronchial artery configuration is quite variable. Most common configurations are:
Single right bronchial artery
Multiple left bronchial artery
- •
Superior vena cava (SVC) congenital variants
- •
Persistent left SVC (most common variant)—right SVC may be normal, small, or absent
- •
Right upper lobe partial anomalous pulmonary venous return—one or more pulmonary veins drain into the systemic venous system or right atrium (RA) instead of the left atrium (LA)
- •
SVC aneurysm—asymptomatic, caused by congenital weakness in the SVC wall or muscular layer of the tunica adventitia
- •
- •

Imaging Principles
Computed Tomography
- •
Indications:
Diagnosis and surveillance of aneurysms
Aneurysm rupture
Aortic dissection
- •
Spiral CT is currently expanding CT indications.
- •
CT is not yet validated as the sole evaluation of traumatic arch injuries.
- •
Magnetic Resonance Imaging
- •
Indications:
Diagnosis and surveillance of aneurysms
Aortic dissection
- •
Allows evaluation of the aortic root better than CT
- •
MRA of great vessels is gaining in diagnostic importance.
- •
Aortography
- •
Indications:
Preoperative aneurysm assessment
Traumatic arch injury
Equivocal CT or MRI
- •
Remains the gold standard diagnostic tool but is rarely the initial diagnostic examination for the thoracic aorta.
- •
Transesophageal Echocardiography
- •
Indications:
Aortic dissection
Associated cardiac disease (aortic insufficiency [AI], left ventricle [LV] dysfunction)
- •
Not validated to evaluate traumatic aortic injury
- •
Thoracic Aortography Technique
- •
Catheter: 7- to 8-Fr pigtail
- •
Contrast: Hypaque 76 or nonionic equivalent
- •
Rate: 30–40 mL/s × 2 s (total: 60–80 mL)
- •
Fast filming: 3/s × 3. Higher rate for DSA.
- •
Always perform imaging in at least two orthogonal views.
- •
Thoracic Aortic Aneurysm
General
True aneurysms contain all three major layers of an intact arterial wall. False aneurysms lack one or more layers of the vessel wall; false aneurysms are also called pseudoaneurysms. Most thoracic aortic aneurysms are asymptomatic and are detected incidentally. Clinical symptoms usually indicate large size, expansion, or contained rupture.
Causes
- •
Atherosclerosis
- •
Dissection
- •
Cystic medial generation
- •
Connective tissue diseases (Marfan, Ehlers-Danlos)
- •
Syphilis
- •
Posttraumatic pseudoaneurysm
- •
Mycotic aneurysm
- •
Aortitis
Takayasu arteritis
Giant cell aortitis
Collagen vascular diseases (rheumatoid arthritis, ankylosing spondylitis)
- •
Pearls
- •
True aneurysms tend to be fusiform.
- •
False aneurysms tend to be saccular.
- •
Posttraumatic, mycotic, and postsurgical aneurysms are false aneurysms.
- •
Bicuspid aortic valve is a risk factor for thoracic aortic aneurysm
- •
Ascending aorta aneurysm associated with annuloaortic ectasia, syphilis, postoperative aneurysm, aortic valve disease, or aortitis.
- •
thoracic aortic aneurysm mimics: ductus diverticulum, aortic spindle
- •
Atherosclerotic Aneurysm
90% of these aneurysms are fusiform because thoracic atherosclerosis is usually circumferential; 10% are saccular. A saccular shape should therefore raise the suspicion of a false aneurysm (pseudoaneurysm). Atherosclerotic thoracic aneurysm is more common in the descending aorta and has a high incidence of concomitant AAA.
Complications
Expansion
- •
Pain
- •
Hoarseness, dysphagia
- •
Aortic insufficiency
- •
Rupture (uncommon if <5 cm)
- •
Rupture into pericardial or pleural space, trachea, mediastinum, esophagus
- •
Rupture into SVC (aortocaval fistula), PA (aortopulmonary fistula)
- •
Radiographic Features
Angiography ( Fig. 8.8 )
- •
Most useful in preoperative assessment of asymptomatic patients
- •
Appearance
Fusiform > saccular
Determine proximal and distal extent (often thoracoabdominal)
Determine branch involvement
Coexistent aneurysmal or occlusive disease
- •
Not accurate in determining aneurysm size because of:
Magnification
Layering of contrast
Thrombus in the lumen
- •
An indicator of an impending rupture is focal ectasia (so-called pointing aneurysm, or nipple of aneurysm)
- •