Chapter Outline
Pulmonary Imaging, 691
Cardiac Imaging, 695
Gastrointestinal Imaging, 703
Genitourinary Imaging, 706
Bone Imaging, 709
Thyroid Imaging, 712
Positron Emission Tomography, 716
Miscellaneous Imaging Techniques, 720
67 Ga Citrate Imaging Isotope, 720
Leukocyte Imaging, 720
Brain Imaging, 721
Lymphoscintigraphy, 722
Tumor Imaging, 722
Differential Diagnosis, 723
Radiopharmaceuticals, 723
Pulmonary, 724
Cardiovascular, 725
Gastrointestinal, 725
Genitourinary, 726
Bone, 727
Thyroid, 728
Pulmonary Imaging
Radiopharmaceuticals
Pulmonary scintigraphy uses ventilation agents and/or perfusion agents, depending on the specific imaging task.
| Agent | Half-life | Main Energy | Collimator | Comments |
|---|---|---|---|---|
| Ventilation | ||||
| 133 Xe | 5.2 days | 81 | Low | Inexpensive; washout images helpful |
| 99m Tc DTPA aerosol | 6 hr | 140 keV | Low | Delivery not as good as with gases; multiple projections possible |
| Perfusion | ||||
| 99m Tc MAA | 6 hr | 140 keV | Low | |
If both ventilation (V̇) and perfusion (Q̇) imaging are performed (V̇/Q̇ scan), the ventilation imaging part is usually performed first because the 81 kiloelectron volt (keV) 133 xenon (Xe) photon energy lies in the range of significant Compton downscatter of the 140-keV 99m technetium (Tc) photon. Examination rooms must have negative internal pressure so that escaped Xe is not recirculated to other areas. Exhaled Xe can be vented to the outside atmosphere.
133 Xenon (XE)
133 Xe is a commonly used ventilation agent. It is relatively inexpensive and has a physical half-life of 5.2 days. Xe is an inert gas that is distributed to lung spaces through normally ventilated areas. Three phases of distribution are usually distinguishable although the biologic half-life is less than 1 minute:
- •
Inspiration (15–20 s)
- •
Equilibrium (patient breathes Xe/O 2 mixture in a closed system for 3–5 min)
- •
Washout (patient breathes room air and exhales into charcoal trap)
- •
Less than 15% of inhaled gas is absorbed in the body. Since Xe is highly soluble in fat, it localizes to liver and fatty tissues once absorbed. Xe also adsorbs onto plastic syringes (10% at 24 hours), for which reason glass syringes are used for handling. Xe ventilation cannot be performed on a portable basis because negative pressure is required to remove gas. Tc aerosol can be used for portable scans.
99M tc Diethylenetriaminepentaacetic Acid (DTPA) Aerosol
A large amount (1110–1850 megabecquerel [MBq]) of activity is loaded into a specially shielded nebulizer that produces droplets containing the radionuclide. Approximately 18–28 MBq of activity reaches the lungs during the 3–5 minutes of breathing. Once in the lungs, droplets diffuse through interstitium into capillaries and 99m Tc DTPA is finally excreted renally. Pulmonary clearance usually takes >1 hour (much faster in smokers and those with idiopathic pulmonary fibrosis [IPF] or acute respiratory distress syndrome [ARDS]), for which reason the aerosol cannot be used for single breath or washout phase imaging. Slow pulmonary clearance allows multiple projection images to be obtained typically in the same views as in the perfusion study. Because the aerosol delivers only a small amount of activity (20% of activity used for perfusion imaging), ventilation imaging is performed before perfusion imaging. Alternatively, a reduced dose of macroaggregated albumin particles (MAA) (1 millicurie [mCi]) can be given first for perfusion imaging. Particle deposition in large central airways occurs in obstructive lung disease.
99M tc Macroaggregated Albumin (MAA)
The theoretical basis for using MAA in perfusion imaging is that particles become physically trapped in arterioles, thus allowing one to measure regional perfusion. MAA is prepared by heat and pH denaturation of human serum albumin (HSA). For quality assurance purposes, the size of at least 100 particles has to be determined (optimum from 10–90 µm; particles should not be <10 µm or >150 µm). 200,000 to 700,000 MAA particles are injected intravenously (IV) to occlude precapillary arterioles (20–30 µm) and capillaries (8 µm). Injection of <70,000 particles leads to a statistically inaccurate examination (because of quantum mottle). The number of injected particles should be reduced in:
- •
Pulmonary hypertension (HTN)
- •
Neonates, pediatric patients
- •
R–L shunts
- •
Pharmacokinetics
- •
>90% of particles are trapped in lung capillaries during first pass (particles <10 µm are phagocytosed by liver and spleen).
- •
Approximately 100,000 of the 280 billion capillaries are occluded during a normal lung perfusion scan.
- •
Particles are cleared from lungs by enzymatic hydrolysis (biologic half-life: 2–10 hours).
- •
Renal clearance of 99m Tc MAA is 30%–40% at 24 hours.
- •
Because the particle number/dose must be known at time of administration, all doses must be given within 6 hours of preparation.
- •
Technique
Indications
Common indications for pulmonary imaging include:
Elective V̇/Q̇ scan
- •
Chronic thromboembolic pulmonary HTN
- •
Baseline posttreatment scan
- •
R–L shunts
- •
Emergency V̇/Q̇ scan (e.g., at night)
- •
Clinical suspicion of acute pulmonary embolus in the setting of a normal chest X-ray (CXR)
- •
Contraindication to computed tomography (CT) contrast.
- •
Surgical applications
- •
Preoperative evaluation of lung function
- •
Follow-up postpulmonary thromboendarterectomy
- •
Contraindications
No absolute contraindications exist. Relative contraindications include:
- •
Pulmonary arterial hypertension (PAH)
- •
R–L shunts (particles end up in systemic circulation)
In both of these cases it is possible to perform the study with a reduced particle count
- •
Hypersensitivity to HSA
- •
Protocol
- 1.
Obtain history and risk factors.
- 2.
Ventilate patient with 133 Xe (370–740 MBq) and image in posterior projection: The gamma energy of Xe is 81 keV and will be attenuated by 1 cm of inflated lung and overlying breast tissue.
- •
Initial breath: single image
- •
Equilibrium: 2 × 90-second images
- •
Washout: 3 × 45-second images
- •
Retention: left posterior oblique (LPO), posterior, right posterior oblique (RPO) images of 45 seconds each
- •
- 3.
Injection of 99m Tc MAA (150 MBq) in supine position and image:
- •
6-standard views: posterior, RPO, LPO, anterior, right anterior oblique (RAO), left anterior oblique (LAO)
- •
Lateral views
- •
- 1.
Information that should be obtained in all patients includes:
CXR (within 12 hours of assessment)
- •
Normal or minimal lung abnormality on CXR is typical in pulmonary embolism (PE).
- •
Normal CXR does not exclude PE but facilitates interpretation of a V̇/Q̇ scan (i.e., absence of matched hypoventilated/hypoperfused consolidations).
- •
Lower extremity ultrasound (US) (optional)
- •
Sensitivity for detecting femoropopliteal deep vein thrombosis (DVT), 95%
- •
Only approximately 30% of patients with PE have documented DVT.
- •
Imaging
Normal Images
Xe Ventilation
Homogeneous distribution of activity occurs in the three phases ( Fig. 12.1 )
- •
Washin
- •
Equilibrium
- •
Washout; complete clearing should occur within 2–3 minutes.
- •

Trapping of Xe on washout is indicative of airway obstruction (e.g., bullae, chronic obstructive pulmonary disease [COPD]). Hallmarks of obstructive disease are decreased washin, slow equilibration, and delayed washout.
Perfusion ( Fig. 12.2 )
- •
Normal identifiable structures: heart, aortic arch, fissures
- •
Anterior indentation on lung on LPO represents the heart.
- •
Slight gradient of activity from posterior to anterior reflects greater perfusion to dependent portions of lung in supine patient.
- •
Activity at apex is usually less than at bases (less parenchymal volume at apex).
- •
Subsegmental perfusion defects occur in 7% of normal population.
- •

Pulmonary Embolism (PE)
V̇/Q̇ imaging requires the use of two sequential tracers: a ventilation (i.e., breathing) agent and a perfusion (i.e., intravascular) agent ( Fig. 12.3 ). Two tracers are used rather than one because altered pulmonary perfusion alone is a nonspecific finding that occurs in many pulmonary diseases, but V̇/Q̇ mismatches are fairly specific for PE. V̇/Q̇ mismatch refers to regions of decreased perfusion (“cold”) that have normal ventilation. If the perfusion part of the study is normal, PE is excluded and ventilation imaging is not required.

Recent use of V̇/Q̇ scanning with single photon emission computed tomography (SPECT) allows three-dimensional (3D) visualization of segments previously not identified by planar imaging, such as the medial basal segment of the right lower lobe (RLL). The lung segments are more clearly defined and can be viewed in any orthogonal plane, resulting in better detection and characterization of defects. SPECT also improves image contrast, thus decreasing the rate of intermediate scan reports.
Modified Prospective Investigation of Pulmonary Embolism Detection (PIOPED) Criteria for Scan Interpretation
High probability (≥80%)
- •
2 or more segments of V̇/Q̇ mismatch
- •
Intermediate (20%–79%)
- •
All other findings
- •
Multiple perfusion defects with associated x-ray opacities
- •
Greater than 25% of a segment and less than two mismatched segmental perfusion defects with normal radiograph
- •
Solitary moderate large matching segmental defect with matching X-ray
- •
Difficult to characterize as high probability or low probability
- •
Low probability (<20%)
- •
Nonsegmental perfusion abnormalities; enlargement of the heart/hilum, elevated hemidiaphragm, costophrenic angle effusion, and linear atelectasis with no other perfusion defect in either lung
- •
Perfusion defect smaller than corresponding radiographic lesion
- •
Matched ventilation and perfusion defects with normal CXR
- •
Small subsegmental perfusion defects
- •
Implications of Scan Results
- •
High probability: treat for PE
- •
Intermediate/indeterminate probability: CT pulmonary angiogram
- •
Low probability: unlikely to be PE. Consider other diagnoses. Obtain CT pulmonary angiogram if clinical suspicion remains very high.
- •
Normal perfusion study excludes PE
- •
V̇/Q̇ Scan to Monitor Sequelae/Resolution of PE
- •
Most PE perfusion abnormalities resolve within 3 months. Thus a baseline posttreatment scan should be obtained several months after initial diagnosis.
- •
Baseline scans are helpful to diagnose recurrent PE.
- •
Acute perfusion defects tend to be sharply defined; old or resolving perfusion defects tend to be less well defined.
- •
Pearls
- •
Small perfusion defects (“rat bites”) almost never represent PE.
- •
If ventilation abnormalities occupy >75% of lung, PIOPED criteria classify the abnormality as indeterminate or nondiagnostic for PE.
- •
If cause of matched V̇/Q̇ abnormalities and CXR abnormality is unknown, then scan is classified as indeterminate.
- •
Intermediate and indeterminate scans have the same diagnostic significance (i.e., a PE has not been ruled in or ruled out). Some radiologists use the terms interchangeably.
- •
Right upper quadrant uptake on ventilation images can be seen in fatty liver.
- •
Injection of Swan-Ganz catheter may lead to accumulation of activity in one lung on perfusion images.
- •
Heterogeneous perfusion of both lungs with perihilar hot spots may be seen when 99m Tc MAA is allowed to settle and aggregate before injection.
- •
R–L shunt: uptake in brain, kidneys, spleen
- •
Free 99m Tc pertechnetate: uptake in thyroid, kidneys, stomach, salivary glands
- •
Other Patterns
Stripe Sign ( Fig. 12.4 )
This sign refers to a perfusion abnormality with a zone of preserved peripheral perfusion. Because PE is pleural based, presence of this sign makes PE unlikely.

Reverse Mismatch
Normal perfusion with abnormal ventilation. Most commonly as a result of atelectasis.
Pulmonary Edema (PE)
- •
Redistribution of blood away from dependent portions of the lung
- •
Pleural effusions, fissural “highlighting”
- •
Bullae, Emphysema, COPD
- •
Delayed washout on ventilation images: air trapping
- •
Matched V̇/Q̇ defects
- •
Pulmonary Arterial Hypertension (PAH)
Diffusely heterogeneous perfusion with many small peripheral perfusion abnormalities, “contour mapping.”
Evaluation of Lung Function ( Fig. 12.5 )
Commonly performed in patients undergoing lung resection. Using a computer program, the overall ventilation and perfusion of each lung is determined.

Cardiac Imaging
Radiopharmaceuticals
201 Thallium (TI) Chloride
201 Tl (“perfusion marker”) is cyclotron-produced. It distributes proportionally to cardiac output in all tissues except brain (because of intact blood-brain barrier) and fat. Cellular uptake occurs in any tissue if the cellular Na + /K + pump is intact.
Pharmacokinetics
- •
Myocardial extraction: 3%–4% of total dose (at rest). Localization in myocardium occurs in two phases:
Initial distribution and cellular extraction based on blood flow, which is close to 90%
Delayed “redistribution” based on continued extraction of TI from blood and ongoing washout of previously extracted TI
- •
Unlike the reextraction of TI by myocardium, the washout component of redistribution strongly depends on coronary perfusion, with ischemic areas demonstrating much slower washout than normal regions.
- •
Blood half-life: ranges from 0.5 minutes (exercise) to 3 minutes (rest)
- •
Biologic half-life: 10 days ± 2.5 days
- •
Long biologic and physical half-life (73 hours) limit dose (1–2 mCi) that can be given.
- •
Renal clearance, 4%–8%
Use
- •
Imaging of myocardial ischemia and infarctions
- •
Parathyroid adenoma localization
- •
99M tc Sestamibi ( Fig. 12.6 )
99m Tc sestamibi is an isonitrile (hexakis-2-methoxy-isobutyl isonitrile) containing six isonitrile components. Sestamibi has a high first-pass extraction, a distribution proportional to blood flow, and few or no metabolic side effects. Advantages over 201 Tl include:
- •
Better dosimetry: higher dose can be given, resulting in higher photon flux
- •
Preferred agent for SPECT imaging (more photons)
- •
Higher energy, less tissue attenuation
- •
Preferred for obese patients
- •
Good correlation between 201 Tl and 99m Tc methoxyisobutyl isonitrile (MIBI) in terms of imaging characteristics
- •

Pharmacokinetics
- •
Passive diffusion into myocyte. Myocardial uptake is proportional to diffusion.
- •
99m Tc sestamibi is retained in myocardium because of binding to a low molecular weight protein in the cytosol complex.
- •
Hepatobiliary excretion: prominent liver activity (may interfere with evaluation of inferior wall)
- •
Wait 30–60 minutes before imaging to allow some hepatic clearance.
- •
There is no myocardial redistribution; thus imaging can be performed 1–2 hours after injection.
Tetrofosmin (UpToDate)
Tetrofosmin (Myoview) is a liophilic, cationic diphosphine compound. It has a good myocardial uptake with rapid clearance from the liver, lungs, and blood. The exact mechanism of action has not been well defined; however, it appears to involve potential driven diffusion across the sarcolemmal and mitochondrial membranes.
Pharmacokinetic
- •
Myocardial uptake is proportionate to flow
- •
Minimal redistribution occurs
- •
There may be more rapid washout from the liver than with sestamibi, allowing earlier imaging after injection.
- •
Although there is less experience with tetrofosmin compared with other available agents, the diagnostic accuracy of stress 99m Tc tetrofosmin appears to be similar to that of 201 Tl and 99m Tc sestamibi. Given the many similarities between tetrofosmin and sestamibi, these agents can be used in clinically similar situations.
| 201 Thallium | 99m Tc Sestamibi | Tetrofosmin | |
|---|---|---|---|
| Dose | 74–111 MBq | 740–1850 MBq | 185–1221 MBq |
| Imaging time | Immediate | 60 min | At 15 min during stress, at 30–60 min during rest |
| Cardiac half-life | 3–5 hr | 5 hr | 6 hr |
| Cardiac uptake | 3%–4% | 2% | 1% |
| Redistribution | Yes | Slight | No/minimal |
99M TC Red Blood Cell (RBC) Labeling
Autologous RBC labeling is best performed by one of three methods of pertechnetate incorporation into RBC. RBC labeling is based on the principle that (+7) TcO 4 crosses the RBC membrane but reduced (+4) Tc does not. TcO 4 can be reduced intracellularly to (+4) Tc with tin (Sn 2+ ); reduced Tc binds to the beta chain of hemoglobin.
Uses
- •
Cardiac-gated blood-pool studies
- •
Bleeding studies
- •
Hemangioma characterization
- •
Spleen imaging (alternative to sulfur colloid)
- •
Methods of Labeling Autologous RBCs
In vivo labeling
- •
1 mg of stannous pyrophosphate injected IV
- •
After 20 minutes, 740 MBq of 99m TcO 4– is injected.
- •
Disadvantage: labeling efficiency <85%; low target-to-background ratio
- •
Modified in vivo labeling (in vitro)
- •
1 mg of stannous pyrophosphate injected IV
- •
After 20 minutes, 5 mL of blood is withdrawn and incubated in a syringe with 740 MBq of 99m TcO 4– for 10 minutes
- •
Incubated RBCs are reinjected.
- •
Advantage of this method is a higher labeling efficiency: 30 minutes after injection 90% of administered radioactivity remains in the intravascular space.
- •
In vitro labeling
- •
Entire labeling procedure is performed outside patient.
- •
Requires 30 minutes
- •
Best labeling efficiency
- •
Using commercial kit (UltraTag; Mallinckrodt Pharmaceuticals, Staines-upon-Thames, UK), blood is aspirated in anticoagulant and mixed in vial with stannous ion for 5 minutes.
- •
Subsequently mixed with sodium hypochlorite, then citrate buffer with dextrose
- •
99m TcO 4– is added and reinjected after incubation for 20 minutes.
- •
Causes of Poor RBC Labeling
- •
Drug interactions (e.g., heparin, doxorubicin, contrast agents)
- •
Antibodies: transfusions, transplantation
- •
Short incubation time
- •
Too much or too little stannous ion
- •
Pearls
- •
In vitro methods used in clinical practice.
- •
Heat-damaged RBCs are used for selective spleen imaging.
- •
99m Tc-labeled HSA is an alternative agent for blood-pool imaging but provides less target-to-background because of extracellular diffusion.
- •
New long circulating polymers are being developed that may obviate the need for RBC labeling.
- •
Myocardial Perfusion Scintigraphy
General ( Figs. 12.7 – 12.8 )
99m Tc-labeled perfusion agents ( 99m Tc sestamibi and 99m Tc tetrofosmin) are the most commonly used radioisotopes for SPECT myocardial perfusion imaging. The physical half-lives of 99m Tc and 201 Tl are 6 and 72 hours, respectively, allowing larger doses of 99m Tc -labeled tracers to be administered compared with 201 Tl while maintaining lower radiation exposure. 99m Tc also has higher energy, less scatter, and less attenuation of photons compared with 201 Tl and is therefore used with greater frequency in the United States.


Techniques
There are three techniques of nuclear cardiac perfusion imaging:
Physical exercise test (significant increase in myocardial workload). This is the preferred technique:
- •
Treadmill test (standard Bruce protocol or modified Bruce protocol)
- •
Bicycling
- •
Pharmacologic “stress” test (no significant increase in myocardial workload)
- •
Coronary flow increases after administration of vasodilators; stenotic vessels do not respond as much and areas of hypoperfusion are accentuated.
Workload is not increased; ischemia seldom occurs.
Agents used: dipyridamole (acts indirectly by reducing the degradation of endogenous adenosine)
Adenosine (Adenocard): direct vasodilator with short duration
Regadenoson (Lexiscan): direct vasodilator with slightly longer duration than adenosine
- •
Dobutamine: chronotropic and inotropic agent (not a vasodilator)
- •
Rest study
- •
Use: patients for whom exercise or vasodilators are contraindicated (intraaortic balloon pump, coronary artery bypass graft)
- •
Cannot detect ischemia
- •
Used mainly to determine myocardial viability
- •
Treadmill Test
- 1.
Patient nil per os (NPO) to decrease splanchnic activity
- 2.
Patient is exercised on treadmill to maximum stress (i.e., completion of protocol) or other endpoint
- •
85% predicted maximum heart rate (PMHR) = 220 – age in years)
- •
Unable to continue secondary to fatigue or dyspnea
- •
Cardiovascular signs/symptoms: severe angina, hypotension, arrhythmias, ischemic electrocardiogram (ECG) changes
- •
- 3.
First dose of radiotracer should be injected at peak exercise. Continue exercise for 1 minute to allow the radiotracer to circulate before the termination of exercise.
- 4.
Depending on the radiotracer, image acquisition may begin almost immediately following termination of exercise, or it may be delayed up to several hours after exercise.
- 1.
Factors that limit exercise stress test:
- •
Inadequate stress decreases diagnostic sensitivity.
- •
Heart rate should increase to at least 85% of PMHR.
- •
Drugs that limit heart rate (HR) response decrease sensitivity of the stress test (beta-blockers, calcium-channel blockers, digoxin).
- •
Nondiagnostic ECG: left ventricular hypertrophy (LVH), left bundle branch block (LBBB), baseline ST-T abnormalities
- •
Dipyridamole Test
- 1.
Patient NPO (no coffee, caffeine, or other xanthine products for 12 hours)
- 2.
Dipyridamole IV infusion (0.6 mg/kg over 4 min): HR increases 20%, blood pressure (BP) decreases 10 mm Hg
- 3.
201 Tl (3 mCi) is given 10 minutes after the dipyridamole is started (peak blood dipyridamole level).
- 4.
Image immediately
- 5.
Administer aminophylline (50–100 mg) to reverse side effects (flushing, headaches) of dipyridamole.
- 6.
Reinject 201 Tl (1.5 mCi) for redistribution images.
- 1.
Adenosine Test
- 1.
Patient NPO for 3 hours (no coffee, caffeine, or other xanthine products for 24 hours)
- 2.
Adenosine IV infusion (0.14 mg/kg per min over 4–6 min)
- 3.
201 Tl (3 mCi) is given 3 minutes after the adenosine infusion is started.
- 4.
Begin imaging 3 minutes after completion of adenosine infusion.
- 5.
Stop infusion if side effects encountered (atrioventricular [AV] block), given short half-life (10 s)
- 6.
Reinject 201 Tl for redistribution images.
- 1.
Regadenoson Test (From the Massachussetts General Hospital [MGH] Protocol)
- 1.
Patient NPO for 3 hours (no coffee, caffeine, or other xanthine products for 12 hours)
- 2.
Regadenoson rapid IV injection (over 10–20 s)
- 3.
Administer a 5 mL saline flush immediately following bolus completion.
- 4.
Radiopharmaceutical is given 60 seconds after the saline injection and again flush with saline to make sure the dose is in.
- 5.
Begin imaging at least 30 minutes after stress injection, at least 60 minutes after rest injection. If hepatic activity exceeds myocardial activity, imaging should be delayed an additional 30 minutes, whenever possible.
- 6.
Stop infusion if side effects encountered (AV block), given short half-life
- 1.
Dobutamine Test
- 1.
Hold beta- and calcium-channel blockers
- 2.
Begin dobutamine IV infusion at 0.005 mg/kg per minute and increase by 0.005 mg/kg per minute every 3 minutes to maximum of 0.04 mg over 4 minutes: HR increases 20%, BP decreases 10 mm Hg
- 3.
201 Tl is given 1 minute after the maximum dose achieved and infusion continued for at least 1 additional minute
- 4.
Beware of arrhythmias; consider atropine 0.5 mg to raise HR and reduce needed dobutamine dose; beta-blocker (esmolol, metoprolol) for reversal
- 1.
Rest and Redistribution Study
- 1.
Injection of first dose of 201 Tl (74 MBq)
- 2.
Image immediately
- 3.
No reinjection of second dose
- 1.
99M tc Sestamibi Imaging
1-day protocol:
- 1.
Rest and stress studies are performed on same day.
- 2.
May begin with rest or stress study first
- 3.
Rest-stress: Administer 8–10 mCi 99m Tc sestamibi and image 30–60 minutes. 2–4 hours later, inject larger dose (25–30 mCi) and image at 15–60 minutes.
- 4.
Stress-rest: Administer 8–10 mCi 99m Tc sestamibi at peak stress and image in 15–60 minutes (longer delay is selected in pharmacologic stress because of liver/splanchnic uptake). Wait 2–4 hours and administer a larger dose (25–30 mCi) and image at 30–60 minutes.
- 1.
2-day protocol:
- 1.
Performing rest and stress studies 1 day apart allows use of full dose (25–30 mCi) of 99m Tc sestamibi.
- 2.
Stress study performed first and if normal may obviate need for rest study.
- 3.
Stress: inject 25–30 mCi at peak stress and image at 15–60 minutes.
- 4.
Rest: inject 25–30 mCi and image at 30–60 minutes.
- 1.
Dual isotope protocol:
- 1.
Rest study with 201 Tl (3 mCi) is performed first, followed immediately by stress study with 99m Tc sestamibi (25–30 mCi).
- 2.
Quicker to perform than other protocols
- 1.
Best performed with multidetector camera
- •
Images are obtained over a 180-degree arc at 6-degree intervals: 45-degree RAO to 45-degree LPO
- •
The slice thickness is approximately 1 cm.
- •
Total imaging time: single detector 20–30 minutes; multidetector 10–15 minutes
- •
Contraindications for Nuclear Cardiology Stress Test
Absolute
- •
Acute myocardial infarction (AMI)
- •
Severe aortic stenosis (AS)
- •
Severe reaction to stress agent
- •
Severe pulmonary HTN
- •
Obstructive hypertrophic cardiomyopathy
- •
Combination of low ejection fraction (EF) (20%) and documented recent ventricular fibrillation (VF) or ventricular tachycardia (VT)
- •
Cocaine within 24 hours
- •
Pregnancy
- •
Unstable angina
- •
Relative
- •
Severe mitral stenosis
- •
HTN (>180/100 mm Hg)
- •
Hypotension (<90 mm Hg, systolic)
- •
Tachycardia (>120/min)
- •
Wheezing, bronchospasm
- •
Inability to communicate
- •
Acute illness such as pericarditis, pulmonary embolus, infection, fever
- •
Normal Images and Variants ( Fig. 12.9 )
Uniform distribution of activity should be present in the myocardium.

Variations
- •
Diaphragmatic attenuation: inferior myocardial wall may be attenuated ( Fig. 12.10 )

FIG. 12.10
- •
Thin basal myocardium: decreased activity along the most superoposterior aspect of images (cardiac valve plane)
- •
Nonuniform activity may be seen in the proximal septum.
- •
Splanchnic uptake may be seen after a recent meal, with inadequate exercise, and in dipyridamole and sestamibi studies.
- •
“Hot” papillary muscles may make adjacent myocardium appear hypoperfused.
- •
Apical thinning refers to decreased activity in the cardiac apex (common in dilated hearts) ( Fig. 12.11 ).

FIG. 12.11
- •
Image Interpretation
- 1.
Adequacy of study
- •
Did patient achieve 85% PMHR?
- •
Splanchnic uptake (minimal exercise, not NPO)
- •
- 2.
Heart size and wall thickness
- •
Subjective assessment
- •
Transient ischemic dilatation (on stress, not rest) is a sign of left ventricle (LV) dysfunction, and may indicate relatively balanced multivessel disease (much of this needs to be changed over to sestamibi)
- •
- 3.
Distribution defects
- •
Full-thickness defect
- •
Partial-thickness defects
- •
Reversible versus irreversible defects
- •
- 4.
Standard image reconstruction planes (cardiac axes: short, horizontal long, and vertical long) ( Fig. 12.12 )
- •
Quantitative polar maps are adjunct to qualitative visual analysis.

FIG. 12.12
- •
- 1.
Abnormal Scan Patterns
Three patterns ( Fig. 12.13 ):
Reversible perfusion pattern
- •
Perfusion defect is present in the stress image with partial or complete fill-in on rest images.
- •
Indicative of ischemia
- •
Rare conditions with this pattern causing false-positive results for ischemia: Chagas disease, sarcoid, hypertrophic cardiomyopathy
- •
Irreversible, fixed perfusion pattern
- •
Perfusion defect persists
- •
Much less specific for ischemia than reversible defects
- •
Often seen with scars (old myocardial infarction), cardiomyopathies, idiopathic hypertrophic subaortic stenosis, coronary spasm, infiltrative or metastatic lesions
- •
Note that three-vessel disease can produce balanced ischemia
- •
No regional perfusion defect identified
- •
May see transient ischemic dilatation, wall motion abnormalities, ECG abnormalities on exercise
SENSITIVITY AND SPECIFICITY
Exercise ECG (%)
201 Tl Stress Test (%)
SPECT
Sensitivity
60
85
Marginal improvement over 201 Tl
Specificity
85
85
Possibly lower
ECG , Electrocardiogram; SPECT , single photon emission computed tomography; Tl , thallium.
- •
Sensitivity of 201 Tl varies with extent of disease:
- •
80% sensitivity for single vessel disease
- •
95% sensitivity for triple vessel disease
- •

Dipyridamole 201 Tl scan appears to have similar sensitivity/specificity as exercise 201 Tl.
Hibernating Myocardium
Refers to chronic ischemia: poorly perfused heart at rest has loss of functional wall motion but is still viable.
- •
Image 10–15 minutes postinjection of Tl and 3–4 hours later
- •
Rest perfusion defects
- •
Normalize on delayed images
- •
Diminished wall motion
- •
Requires revascularization procedure
- •
Stunned Myocardium
- •
Acute event that results from ischemic injury
- •
Normal or near-normal perfusion with decreased contractility
- •
Acute coronary artery occlusion
- •
Positron Emission Tomography (PET) Imaging
82 Rubidium
- •
Myocardial perfusion agent
- •
Generator produced, potassium analog taken up by myocardium via Na/K pump, half-life 76 seconds
- •
Imaging within 5 minutes of injection
- •
13 N-ammonia
- •
Myocardial perfusion agent
- •
13 N is cyclotron-produced, diffuses into myocardium and is trapped, half-life 10 minutes
- •
18 F-Fluorodeoxyglucose (FDG)
- •
Myocardial metabolism
- •
Glucose loading to promote myocardial uptake
- •
Used in combination with perfusion SPECT or PET imaging to assess hibernating myocardium: 18 F-FDG uptake in a region of perfusion deficit indicates viable myocardium whereas matched 18 F-FDG and fixed rest-stress defect are indicative of infarct.
- •
| Myocardium | Perfusion (NH 3 ) | Metabolism (FDG) |
|---|---|---|
| Normal | + | + |
| Ischemia | – or decreased | + |
| Necrosis | – | – |
Indications for PET
- •
Resting and adenosine, or dipyridamole, or dobutamine stress myocardial perfusion PET:
SPECT study equivocal
Obesity (>400 lb)
- •
Ventricular Function Imaging
General
There are two different approaches to studying ventricular function:
- 1.
First-pass studies
- •
Immediately after IV injection of a radiotracer (e.g., 99m Tc DTPA) the bolus is imaged as it passes through heart, lungs, and great vessels. The acquisition ends before the agent recirculates.
- •
A multidetector camera (multiple crystals and photomultiplier tube) for rapid data acquisition is required.
- •
Advantages: fast determination of transit time, intracardiac shunts detectable, right ventricular ejection fraction (RVEF) can be obtained.
- •
Disadvantages: imaging time and count density are limited.
- •
- 2.
Equilibrium studies (gated blood-pool study [GBPS])
- •
The blood pool is currently best imaged with 99m Tc-labeled RBCs.
- •
Gating to the cardiac cycle (frame mode, list mode)
- •
Allows evaluation of segmental wall motion
- •
- 1.
Indications
- •
Evaluation of cardiac drug toxicity (doxorubicin [Adriamycin])
- •
Assessment of ventricular function in coronary artery disease (CAD) and cardiomyopathies
- •
Protocol
- 1.
Inject 99m Tc RBC (740 MBq).
- 2.
Gated images are triggered to the R-wave. Arrhythmias have R-R interval variability and cause distortion of images. Arrhythmia filtering should therefore be performed.
- 3.
Acquire images in two views: anterior, shallow LAO (45 degree).
- 4.
Calculate EF and evaluate wall motion.
- 1.
Image Interpretation
Qualitative Image Assessment
- 1.
Adequacy of study
- •
Determine if labeling of RBC is adequate (free TcO 4- uptake in stomach, thyroid, cardiac-to-background activity)
- •
Determine if gating is adequate (jumps, count dropoff at end of cycle)
- •
- 2.
Heart ( Fig. 12.14 )
- •
Size of cardiac chambers
- •
Thickness of myocardial walls and septum
- •
Ventricular wall motion is graded segmentally. Segments should contract simultaneously; anterior, posterior, lateral walls move to a greater extent than septum or inferior wall; septum should move toward the LV. Atypical motion:
Hypokinesis: minimal wall movement (e.g., injured myocardium)
Akinesis: no wall movement (e.g., scarred myocardium)
Dyskinesis: paradoxical wall movement (e.g., aneurysm)

FIG. 12.14
- •
- 3.
Lung
- •
Lung activity should be similar to liver activity.
- •
Evaluate for areas of oligemia.
- •
- 4.
Great vessels
- •
Determine course and caliber
- •
Aorta should be two-thirds the diameter of pulmonary artery (PA)
- •
- 1.
Quantitative Image Assessment
The LV volume is graphed over time by edge tracing algorithms ( Fig. 12.15 ). The most common quantitative parameters are EF and peak filling rate. Stroke volume or index and cardiac index can also be obtained. Quantitative data are obtained from shallow LAO (45 degree) projection:
EF (systolic function)
- •
LVEF = (end-diastolic volume [EDV] – end-systolic volume [ESV])/(EDV – background).
- •
Normal values: LVEF 50%–65%
- •
Normal variability: 5%
- •
Peak filling rate (diastolic function)
- •
Index of early ventricular filling
- •
Abnormalities in peak filling rates may precede EF changes (diastolic dysfunction may be present with normal LV systolic function).
- •

Pearls
- •
GBPS is the preferred and most accurate imaging technique for LVEF determination.
- •
The LVEF can be falsely elevated if background range of interest includes spleen.
- •
Motion artifact may be assessed on review of sinogram and unprocessed images.
- •
LVEF calculations by echocardiography are often less accurate than by nuclear imaging because:
Cardiac visualization is incomplete, making quantitation difficult.
US is operator dependent.
- •
Gastrointestinal Imaging
Radiopharmaceuticals
General
| Radiopharmaceutical | Target | Main Use |
|---|---|---|
| 99m Tc sulfur colloid | RES distribution | Confirmation of splenic tissue |
| 99m Tc HIDA | Biliary excretion | Acute cholecystitis |
| 99m Tc RBC | Blood pool | Bleeding, |
| 99m TcO 4– | Mucosal secretion | Meckel scan |
99M tc Sulfur Colloid
Pharmacokinetics
- •
Blood half-life is 2–3 minutes. 90% extraction during first pass.
- •
Complete clearance by reticuloendothelial system (RES) of liver (80%–90%), spleen (5%–10%), and bone marrow. Localization of the agent in these tissues is flow dependent and requires functional integrity of RES cells.
- •
Pearls
- •
Overall hepatic function can be assessed by the pattern of uptake.
- •
Accumulation of 99m Tc sulfur colloid in renal transplants indicates rejection.
- •
In severe liver dysfunction, an increase in activity can be seen in marrow, spleen, lungs, and even kidneys (“colloid shift”).
- •
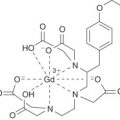
99M tc Hepatobiliary Agents ( Fig. 12.16 )
All newer hepatobiliary agents are Tc-labeled iminodiacetic acid derivatives (abbreviated HIDA where H stands for hepatic). Commonly used compounds are the diisopropyl derivative (disofenin, diisopropyl iminodiacetic acid [DISIDA]), which has the highest biliary excretion, and mebrofenin (BROMIDA), which has the fastest hepatobiliary extraction.

Pharmacokinetics
- •
Blood half-life is short (10–20 min depending on compound)
- •
95%–99% biliary excretion into small bowel (SB)
- •
Urinary excretion may be higher in patients with impaired liver function or common bile duct (CBD) obstruction
- •
Res Colloid Imaging
Indications
Define functioning splenic tissue.
- •
Determine if a primary liver mass has RES activity.
- •
Bone marrow imaging (rare and usually in combination with indium [In] white blood cell [WBC] imaging)
- •
Image Interpretation
- •
Normal liver uptake > spleen uptake.
- •
Colloid shift occurs in cirrhosis: spleen, bone marrow uptake > liver uptake.
- •
Other causes:
Hepatic cirrhosis
Alcoholic liver disease
Portal HTN
Diffuse metastases with severely impaired liver function
Fatty infiltration of liver
Diffuse hepatitis
Hemochromatosis
Amyloidosis
Lymphoma
Leukemia
Sarcoidosis
- •
All hepatic mass lesions are cold except for focal nodular hyperplasia (FNH), which may have RES activity.
- •
Nonvisualization of spleen on colloid scan
Splenectomy
Sickle cell disease
Congenital absence of spleen (Ivemark syndrome)
Tumor replacement
Infarction
Traumatic avulsion or volvulus
Functional asplenia
- •
Postsurgical hypoxia
- •
Graft-versus-host (GVH) disease
- •
Chronic hepatitis
- •
Systemic lupus erythematosus (SLE)
- •
- •
- •
Hepatobiliary Imaging
Normal Scan
Protocol
- 1.
Inject 185–300 MBq of 99m Tc-labeled iminodicetic acid (IDA) (higher dose if bilirubin elevated).
- 2.
Static images every 5 minutes until the gallbladder (GB) and SB are identified (usually at <1 hour); when GB and intestines are visualized, the study is complete.
- 3.
Delayed imaging is necessary, for up to 4 hours or administration of morphine is performed, if the GB is not visualized.
- 1.
Interpretation ( Fig. 12.17 )
- 1.
Hepatic activity can be
- •
Normal
- •
Delayed (reduced hepatic extraction in hepatocellular disease). With bilirubin levels >20 mg/dL, study results are usually equivocal.
- •
- 2.
GB activity
- •
Present (normal)
- •
Nondemonstration of GB at 1 hour after injection may be due to:
Prolonged fasting (>24 hours; GB is filled with bile)
Recent meal (GB is contracted)
Acute cholecystitis
- •
- 3.
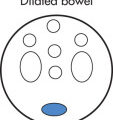
Bowel activity
- •
Present (normal)
- •
Absent (abnormal)
- •
4. Cardiac/blood-pool activity
- •
Delayed clearance of cardiac activity: hepatocellular dysfunction, hepatitis
- •
- 1.

Pharmacologic Intervention if GB Is Not Visualized ( Fig. 12.18 )
There are two pharmacologic maneuvers that can be performed in an attempt to visualize the GB if it has not become apparent after 1 hour of imaging:
- •
Morphine is often given before 4 hours to make the diagnosis of acute cholecystitis.
Dose is 0.04 mg/kg given slowly
Causes spasm of sphincter of Oddi
- •
Sincalide (cholecystokinin [CCK]-8)
Used to contract the GB to avoid false-positive results
Dose is 0.02 to 0.04 µg/kg in 10 mL of saline; given slowly to avoid discomfort and spasm of GB neck
This drug may obscure the diagnosis of chronic cholecystitis by speeding up the visualization of the GB. One way around this it to give CCK only if the GB is not visualized at 30–60 minutes; CCK is followed by an injection of IDA 15–30 minutes later.
- •

Acute Cholecystitis ( Fig. 12.19 )
Acute cholecystitis usually results from acute obstruction of the cystic duct (CD). This is commonly caused by:
- •
CD calculus (most common)
- •
Other causes (acalculous cholecystitis) usually related to inspissated bile in CD
- •
Trauma
- •
Burn
- •

Indications for Scintigraphic Imaging
- •
Normal US but high clinical suspicion for CD calculus
- •
Normal US and suspicion for acalculous cholecystitis
- •
Imaging Findings
- •
Nonvisualization of GB because of CD obstruction. Prerequisites for establishing the diagnosis:
Prolonged imaging (performed for at least 4 hours) or pharmacologic intervention has to be performed: CCK or morphine
- •
Pericholecystic rim of increased activity (hyperemia, local inflammation) in 60% (the “rim sign”).
- •
Visualization of GB excludes acute cholecystitis
- •
False-positive results
Recent meal within 4 hours of imaging
Prolonged fasting for 24 hours of hyperalimentation
Alcoholism
Pancreatitis
Chronic cholecystitis
Hepatocellular dysfunction
Cholangiocarcinoma of CD
- •
False-negative results
Acalculous cholecystitis
Duodenal diverticulum simulating GB
Accessory CD
Biliary duplication cyst
- •
Chronic Cholecystitis
- •
Delayed visualization of GB (can occur with acute cholecystitis)
- •
GB showing a blunted response to CCK is more likely to be chronically inflamed.
- •
Delayed biliary to bowel time in presence of normal GB
- •
Liver Tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree