Chapter 4 Control of the fetal heart and NICE guidelines
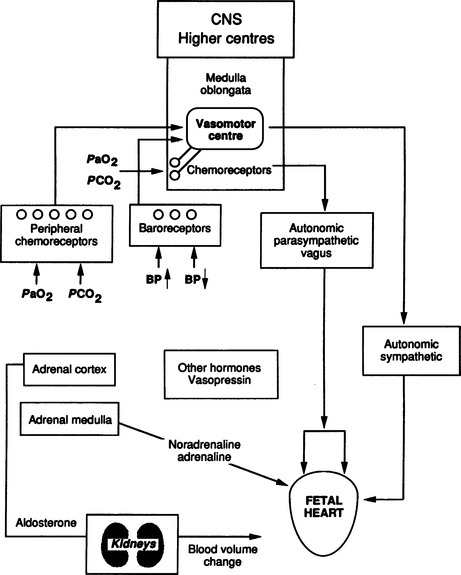
Control of the fetal heart is complex (Fig. 4.1). The fetal heart has its own intrinsic activity and a rate determined by the spontaneous activity of the pacemaker in the sinoatrial (SA) node in the atrium. This specialized area of the myocardium initiates the fastest rate and determines the rate in the normal heart. The atrioventricular (AV) node situated on the atrioventricular septum has a slower rate of activity and generates the idioventricular rhythm seen in complete heart block. Under the circumstances of complete heart block the ventricle beats at 60–80 beats per min (bpm).
The fetal heart rate (FHR) is modulated by a number of stimuli. Central nervous system influence is important with cortical and subcortical influences not under voluntary control. We cannot alter our heart rate at will. The cardioregulatory centre in the brain stem also plays a part. Other physiological factors regulate the heart rate such as circulatory catecholamines, chemoreceptors, baroreceptors and their interplay with the autonomic nervous system.14
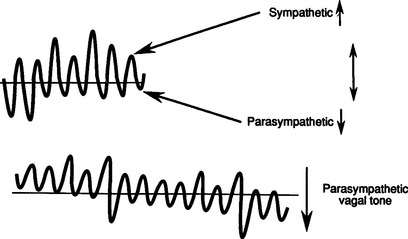
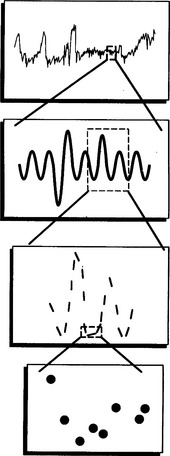
Electronic FHR monitors compute the heart rate based on averaged intervals between beats extrapolated to what the rate would be if that beat interval remained constant. The machine produces a rate recording after only being applied for a few seconds. However, autonomic impulses immediately and constantly take effect changing the beat intervals and immediately altering the heart rate. This is how baseline variability is generated and it indicates integrity of the autonomic nervous system (Fig. 4.2). Baseline variability is actually seen on the tracing. If it is greatly magnified, individual beats, beat-to-beat variation, can be seen with special equipment used for physiological studies (Fig. 4.3). In practice, baseline variability is the preferred term. The sympathetic nervous system and the parasympathetic or vagal system have the specific effect of generating baseline variability. Suppression of vagal impulses by a drug such as atropine causes tachycardia and reduces baseline variability. Physiological mechanisms are complex and incompletely understood. Fortunately the autonomic nervous system is sensitive to hypoxia at a critical level for the fetus and changes in this response are therefore used as important indicators of wellbeing. The sympathetic and parasympathetic systems mature at slightly different rates with respect to gestational age. The sympathetic system matures faster and this results in marginally faster baseline rates in the preterm period. It is of some interest that male fetuses have slightly faster heart rates than female fetuses, however this is of absolutely no diagnostic value. Before 34 weeks’ gestation a higher baseline rate is to be expected. Normal baseline variability suggests good autonomic control and therefore little likelihood of hypoxia.
PATHOPHYSIOLOGICAL MECHANISMS OF DECELERATIONS
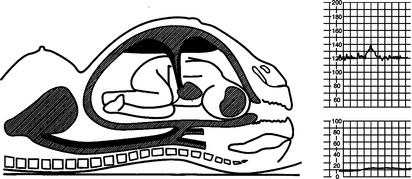
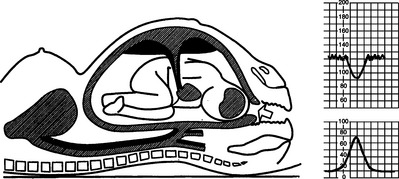
An understanding of the maintenance of autonomic control and the mechanisms of decelerations is important. The following illustrations show the effects of contractions on the fetus and blood flow in diagrammatic form (Figs 4.4–4.9).
Early decelerations are early in timing with respect to the uterine contractions and this is therefore a better term than type I dips. They are most commonly due to compression of the fetal head. A rise in intracranial pressure is associated with stimulation of the vagal nerve and bradycardia. This may be caused by a uterine contraction and the sequence of events in this situation is shown in Figures 4.5–4.9. Head compression decelerations are most frequently seen in the late stages of labour when descent of the head is occurring. Indeed, on some occasions the onset of the second stage of labour can be deduced from the tracing. Decelerations due to head compression are seen at the time of vaginal examination and also when artificial rupture of the membranes has been performed. Early decelerations with contractions are symmetrical and bell-shaped (Fig. 4.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree