23 Controversies in Venous Ultrasound
How Much is Enough?
The venous ultrasound technique is primarily dependent on compression of the vein lumen as the signature of normality. Assessment with color flow Doppler imaging and Doppler spectral waveforms add little value except in the few cases of proximal (iliac or vena cava) venous obstruction. What remains unanswered is, how much of the venous system needs to be interrogated? The minimalists advocate “two-point compression,” while the more compulsive examiners demand that every centimeter of the vein from the groin to the ankle be evaluated. Succinctly stated, there is no agreement regarding the extent of a lower venous ultrasound examination. Adding complexity to the imaging evaluation is the use of serum D-dimer1 tests, with their poor specificity and high false-positive rates. In addition, there is an increasing interest in incorporating clinical prediction tools for DVT such as the 10 items assessed by the Wells score for DVT (Table 23-1).2
TABLE 23-1 The Wells Score for DVT
| Clinical Characteristics | Points |
|---|---|
| Active cancer (patient receiving treatment for cancer within the previous 6 months or currently receiving palliative treatment) | +1 |
| Paralysis, paresis, or recent plaster immobilization of the lower extremities | +1 |
| Recently bedridden for 3 days or more or major surgery within the previous 12 weeks requiring general or regional anesthesia | +1 |
| Localized tenderness along the distribution of the deep venous system | +1 |
| Entire leg is swollen | +1 |
| Calf swelling at least 3 cm larger than that on the asymptomatic side (measured 10 cm below tibial tuberosity) | +1 |
| Pitting edema confined to the symptomatic leg | +1 |
| Collateral superficial veins (nonvaricose) | +1 |
| Previously documented DVT | +1 |
| Alternative diagnosis at least as likely as DVT | -2 |
| Total Score | Clinical Probability | Prevalence of DVT |
|---|---|---|
| <2 points | DVT unlikely | 5.5% (95% CI, 3.8%-7.6%) |
| ≥2 points | DVT likely | 27.9% (95% CI, 23.9%-31.8%) |
CI, confidence interval; DVT, deep venous thrombosis.
The Role of the Unilateral Venous Ultrasound Examination in the Patient With Unilateral Symptoms
In the era of venography, when the radiologist was requested to evaluate a patient for acute DVT, only the symptomatic leg was studied.3 Because of the risk for reactions to intravenous contrast material and the invasiveness of venography, the asymptomatic leg was not studied. Historically, noninvasive vascular laboratories employing impedance plethysmography or phleborheography routinely evaluated both the symptomatic leg and the asymptomatic leg. These laboratories, which are usually directed by surgeons, not radiologists, utilized the physiologic information obtained from the asymptomatic leg as a frame of reference to help diagnose any thrombus that might be present in the symptomatic leg. Following the introduction of venous ultrasound, some sonographers continued to evaluate only the symptomatic leg, while many vascular laboratories, which had developed a pattern of noninvasively evaluating both the symptomatic leg and the asymptomatic leg, continued to evaluate both legs.
Controversy had existed regarding the importance and frequency of finding thrombus in the asymptomatic leg.4,5 Historically, the literature indicated that the asymptomatic leg did not harbor thrombus. Articles were then published suggesting that thrombus could be found in the asymptomatic leg, but the frequency of this finding in a patient with a negative evaluation of the symptomatic leg was less than 1%.3,6–8 Certainly, finding thrombus in the asymptomatic leg of a patient with thrombus in the symptomatic leg would not have altered treatment. The likelihood of finding thrombus solely in the asymptomatic leg was estimated to be between 0% and 1% if the patient did not have any risk factors such as a malignancy.
Bilateral Symptoms: The Role of the Bilateral Venous Examination
As discussed previously, the situation of a patient presenting with bilateral lower leg swelling or bilateral leg pain would have been triaged in the era of venography with reevaluation of the patient or, more likely, with a contrast venogram of only one extremity. It has been suggested that most of these patients have cardiac disease or peripheral vascular disease as the dominant cause of their bilateral swelling.8 However, an alternative should be considered: a significant percentage of these patients harbor lower extremity venous thrombus.7
Certainly, the important factor to consider in the subgroup of patients with bilateral leg swelling would be the presence of risk factors.3 If the Wells score for DVT (see Table 23-1) indicates DVT is unlikely, then the bilateral ultrasound examination will, in my experience and that of others, always be negative. If a patient has a significant underlying risk for DVT, such as malignancy, then the bilateral examination should be performed. If there are no risk factors for DVT, the first assumption should be that the patient has heart disease or underlying peripheral vascular disease as the cause of the bilateral leg swelling. The probability of finding thrombus in the leg is related to the presence of risk factors for DVT. In the absence of any risk factors for DVT, it is unusual to find extremity thrombus. It has been stated that the majority of patients with DVT have one or more risk factors.9
The Extent of the Ultrasound Examination: How Much Needs to Be Studied?
Proper technique for ultrasound evaluation of the vein, as stated both in the American College of Radiology standards in 1993 (revised in 2006) and by the ICAVL, indicates that a patient with a symptomatic extremity should be evaluated from the level of the inguinal ligament to the popliteal fossa in as continuous a manner as possible (Figure 23-1).10 Evaluation of the calf veins is also done in most vascular laboratories.

FIGURE 23-1 Topographic delineation of the lower extremity venous system as examined in routine evaluation.
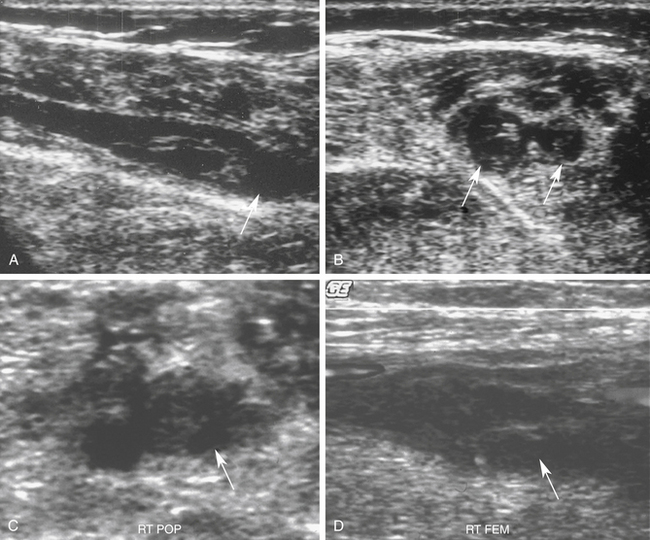
Symptomatic patients tend to have lengthy thrombi involving one or more venous segments.11,12 Symptomatic thrombus may involve multiple venous segments and is biologically different from thrombus that develops in the asymptomatic high-risk patients, where thrombus preferentially involves valve cusps in the calf.13 This observation was demonstrated on retrospective review of venograms and has been confirmed in our ultrasound laboratory. We demonstrated that in approximately 99% of symptomatic cases, evaluation of the femoral or popliteal vein, employing the two-point compression technique, would detect thrombus that extends above the knee. This two-point evaluation requires examination of only the common femoral and popliteal venous areas (Figure 23-2).14
This very abbreviated study detects a high percentage of cases with DVT. The overall decrease in the examination time is slightly in excess of 50%. The potential of the two-point technique has been confirmed by others who have demonstrated that approximately 90% to 95.4% of thrombus would be detected using a two-point compression technique.15 Obviously, there is some degree of compromise with the two-point technique, balancing simplicity versus accuracy. This limited-compression technique is not the accepted standard within the medical community in North America but may have utility in the emergency department and for evaluating the patient with extremely restricted mobility. As an alternative to evaluating the entire leg, this two-point technique provides an equivalent degree of certainty when combined with serial ultrasound examinations in patients with a negative ultrasound examination at baseline (Figure 23-3).16 From the point of view of outcomes, two two-point examinations separated by 7 days, in combination with a D-dimer test, are equivalent to a full-length examination of the lower extremity veins.17
Significance of a Negative Ultrasound Examination
Evidence exists that a negative compression ultrasound study of a symptomatic lower extremity, employing complete evaluation of both the femoral and popliteal veins, provides sufficient validation to withhold anticoagulation.6,18 The need for any follow-up studies in these cases is somewhat less well defined, but the evidence suggests that if the patient remains symptomatic, a repeat study of the lower extremity should be performed 3 to 5 days after the initial examination. An alternative proven technique to end the workup is to demonstrate a normal study of the proximal veins combined with a negative D-dimer. Such a negative combination obviates the need to reassess the leg.19 In 1% to 2% of cases,19 small focal calf thrombi might propagate upward into the popliteal vein and cause symptoms. As will be mentioned in the next section, the direct evaluation of the calf veins needs to be considered as a more direct approach to immediate diagnosis.
Calf Vein Thrombosis
The clinical acceptance of venous ultrasound as a diagnostic technique in the evaluation of the symptomatic patient occurred based on clinical series that did not attempt direct evaluation of calf veins. The initial reports and literature were based only on evaluation of the femoral and popliteal veins. It was with this examination format that the compression ultrasound examination was acknowledged as clinically useful.20 Although isolated calf thrombi are common, they often arise in the hospitalized postoperative or immobile bed-bound patient and, in this context, rarely cause acute clinical problems or clinical symptoms. The outpatient with localized calf symptoms and calf DVT may represent a more aggressive manifestation of thromboembolic disease.
Eighty-eight percent of calf thrombus occurs in the asymptomatic patient, and this accounts for 50% of thrombi in the asymptomatic population. Similarly, the presence of calf thrombus is unlikely to lead to clinically significant pulmonary embolus (PE).21 As pointed out by Moser and LeMoine,22 patients with calf thrombus are unlikely to have signs or symptoms of PE. PE that originates from the calf is usually asymptomatic because of the small clot load. Alternatively, patients with above-knee thrombus have PE in more than 50% of cases, despite the fact that they may not have any signs or symptoms of this phenomenon and evidence of PE is detected only on ventilation/perfusion scans, computed tomographic pulmonary arteriography (CTPA), or pulmonary arteriograms.23–25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree