Fig. 19.1
MR-US correlation of a solid, indeterminate hepatic mass. a Demonstrates a T2-hyperintense mass (arrow) in the left lobe of the liver. Ultrasound examination of the same area demonstrates an approximately 3 cm echogenic lesion (arrow) as seen in (b). Given the adequate visualization and lack of intervening large vasculature (Doppler image not provided), this mass was successfully biopsied percutaneously using an 18G needle (arrow)
Prior to the procedure, a discussion with the pathologist may be needed to determine the appropriate biopsy type and specimen handling. The specimen can be obtained either by fine needle aspiration (FNA) or core needle biopsy. Traditionally, core needle biopsies (as well as surgical biopsies) have been preferred over FNA due to the perceived limitation of the FNA in obtaining adequate sample sizes. This limitation may delay care in cases of suspected small blue round cell tumors such as neuroblastoma, Wilms’ tumor, hepatoblastoma, or Ewing’s sarcoma since the small sample sizes preclude the use of histopathological studies [6]. However, some have argued that even in these cases, FNA can be useful as it can either “rule in” or “rule out” round-cell diagnostic categories [7]. If the decision is made to perform an FNA, presence of an on-site pathologist should be requested to ensure adequate cellularity of the sample. Specimen handling techniques such as formalin fixation, paraffin block, or sterile saline media should also be discussed.
Informed consent should be obtained in all cases from the legal guardian. The consent should at least explain the indications, alternative options, expected risks and benefits, possibility of a non-diagnostic sample, and the post-procedural care [8, 9]. There may be additional factors to consider depending on the individual case. As with most adult interventional procedures, pediatric patients require some level of anesthesia ranging from sedation to general endotracheal anesthesia [10]. While a trained anesthesiologist provides general anesthesia, any privileged provider may administer sedation. The institution and local trends usually determine the type of anesthesia given and who provides it. In the hands of a capable provider, sedation-related complications remain exceeding low [11]. A preoperative consultation with anesthesia can alleviate some of the parents’ and patient’s anxiety and improve patient satisfaction [12, 13].
Indications
Solid Masses
The majority of solid mass and tumor biopsies in children not associated with the liver or kidney are related to abnormal lymph nodes or suspected hematologic and musculoskeletal tumors. Historically, open surgical biopsy has been the primary way of obtaining biopsies in children in order to obtain larger samples. Minimally invasive surgical approaches have also been tried [14–16]. However, many laparoscopic cases have to be converted to “open” due to poor visibility or bleeding. Similar concerns may also hinder a percutaneous approach; but in most cases, the benefits of the percutaneous approach outweigh the hypothetical risks. Research on ultrasound-guided biopsies of solid pediatric masses so far is relatively scant [17–22], but promising.
Liver Abnormalities
Common indications for liver biopsy include cholestasis, hepatomegaly, liver mass, suspected infection, portal hypertension, or biomarker abnormalities [23–25]. In patients with liver transplantation, additional indications may include suspected graft dysfunction, staging and grading of graft dysfunction, or suspected recurrent malignant disease. Options for obtaining liver specimens include the percutaneous approach with or without image guidance, transjugular approach, and surgery. Samples obtained from the percutaneous approach are usually adequate for making the diagnosis. Core needle biopsies are almost always preferred over the FNA.
As in adults, severe coagulopathy is an absolute contraindication to obtaining a liver biopsy. Other liver-specific contraindications include extrahepatic biliary obstruction or cholangitis [25]. Extremely small sizes of premature children and Morbid obesity are also considered relative contraindications for some, although in our experience, they are not usually an issue when using an ultrasound-guided percutaneous approach. Some practitioners may also consider ascites as a contraindication due to the increased risk of peritonitis and bleeding be further subdivided. However, a paracentesis can be performed prior to performing the biopsy. In these cases, the liver should be scanned again after the paracentesis to confirm a safe window. Alternatively, referral to an interventional radiologist for a transjugular biopsy may be used in cases of refractory ascites . The transjugular route may also be used in cases where there is uncorrectable coagulopathy or if indirect portal manometry measurments are required.
Renal Abnormalities
Some of the common indications for renal biopsy in native kidneys include nephrotic syndrome, hematuria, proteinuria, or renal failure [26–29]. Graft dysfunction-related indications may also be present in patients with renal transplant. It is important to note that many believe that percutaneous biopsy in renal masses, especially in suspected Wilms’ tumor, is contraindicated due to potential tumor spread [30]. Recent research, however, remains controversial on this topic.
Percutaneous renal biopsies are likely not as common as liver biopsies in most practices; however, they still remain one of the more relevant procedures for a pediatric interventionalist. Similar to liver biopsies, options for obtaining renal specimens include the percutaneous approach, transjugular approach, and surgery [29]. The transjugular approach is far less common, however, and is reserved for the patients with contraindications to the percutaneous approach (i.e., coagulopathy).
Instruments and Techniques
In the procedure suite, the patient should be placed in the positioning that will allow for the best access to the location of interest. For liver biopsies, the patient’s should be supine and the right arm may need to be abducted. For renal biopsies, the patient may be placed in a prone, lateral or lateral oblique position. Subsequently, the area of interest should be rescanned to confirm the continued presence of the suspected abnormality and presence of a safe biopsy window. Infrequently, such as in the cases of reactive lymph nodes, the previously seen abnormality may no longer be present. Additionally, small, tortuous adjacent vasculature may have been missed on other imaging modalities. Doppler interrogation can help detect these vasculature. This pre-procedural scan can also be used to measure the distance from the skin surface to the lesion.
It is also important to predetermine the needle type and size before the procedure. For FNA, smaller needles, 21 gauge or less, are commonly utilized. For core biopsies, the main types of needles are cutting needles and suction needles . Cutting needles can be further subdivided into spring loaded and non-spring loaded varieties. Suction needles include Menghini, Jamshidi or Klatsin needles [25, 31, 32]. Cutting needles are generally preferred over the suction needles due to decreased fragmentation of the tissue, supposed bigger specimen size, and increased diagnostic yield. Tru-Cut is the most commonly used non-spring loaded cutting needle. Some operators prefer the spring-loaded type of cutting needles, which may be further subdivided into controlled-fire or noncontrolled fire. Spring-loaded cutting needles essentially automate the cutting movement once triggered. If you choose to use the spring-loaded cutting needles , it is also important to understand the “throw length.” This is a measurement of how much the needle will be advanced from the device once it is triggered. As such, if the abnormality is sized only 1 cm, a needle with a 2 cm throw may not be optimal. Similarly, if there is vasculature abutting the lesion at its posterior acoustic wall, a longer throw may lead to unnecessary complications. The controlled-fire variety allows the practitioner to control the length of the throw.
The proceduralist should also understand the difference between coaxial and noncoaxial methods [33]. The coaxial method employs a larger needle (introducer needle) that creates a tract to the lesion and has another needle that passes through it to obtain the actual specimen while the outer larger needle remains in place (Fig. 19.2). The advantages include creation of only a single skin puncture wound and a single trans-capsular puncture in the case of an organ biopsy. Introducer needles also allow for multiple samples at different angles from the single insertion site. Hemostatic agents can also be delivered to the lesion or the capsule of the organ through the introducer needle. The major disadvantages are that the puncture wound is larger than the size of the core specimen and a needle remains within the patient for nearly the entire procedure. As such, patient cooperation or immobilization is essential. Non-coaxial systems, on the other hand, create smaller puncture wounds and remain within the patient a shorter period of time. However, multiple punctures may be needed to obtain sufficient samples. Since pediatric biopsies require multiple samples (upwards of 10–15 samples per lesion in some cases), coaxial systems are preferred.
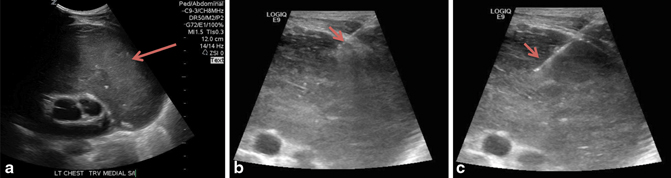
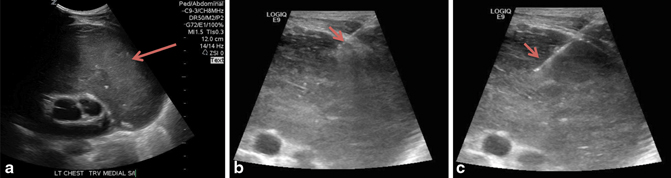
Fig. 19.2
Using a coaxial method for the biopsy of a mediastinal mass. a Demonstrates a large, echogenic mass in the anterosuperior mediastinum (arrow). Given the location of the lesion adjacent to vascular organs and need for multiple samples, the coaxial system was preferred. b Demonstrates placement of an initial 17G introducer needle (arrow) with the distal tip just traversing the outer margin of the lesion. c An 18G biopsy needle (arrow) is seen traversing the lesion further obtaining a sample
For superficial lesions, scanning should be attempted with high-frequency linear transducers (5–15 MHz). Higher frequency waves are easily attenuated and produce a degraded image of the deeper lesions. Conversely, the image quality of the superficial lesions is much better. For deeper lesions, lower frequency curved transducers (2.5–5 MHz) should be used. Additionally, color Doppler examination may be useful for real-time evaluation of any nearby vasculature (Fig. 19.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree