Artery
Catheter
Comments
Left main
JL4
Most often used
JL3.5
Small aortic root
JL5, JL6
Enlarged aortic root
AL-1,2
Posterior takeoff, separate ostia
RCA
JR 4 or modified JR-4
Most often used
3D RCA
Anterior takeoff
AR-1,2
Distorted aortic root
AL-1,2
Anterior takeoff
Aorto-coronary bypass
JR4
Convenient, left- and right-sided grafts
LCB
Left-sided grafts, upward takeoff
MP, AL-1
Dilated aorta, longer reach
RCB
Right-sided grafts
MP, AR-1
Right-sided grafts, downward takeoff
LIMA
IMA
Acute caudal takeoff
IMA—special
Curved subclavian
RIMA
IMA
(c)
Engage coronary ostia.
(d)
Inject contrast (iso or low osmolar contrast) via hand injection or assist device.
(e)
Cine images are commonly recorded on 16 cm and 22 cm magnification. Ideally, images from multiple angulations are taken of each artery in order to visualize important segments in at least two, perpendicular planes (Table 35.2, Fig. 35.1)
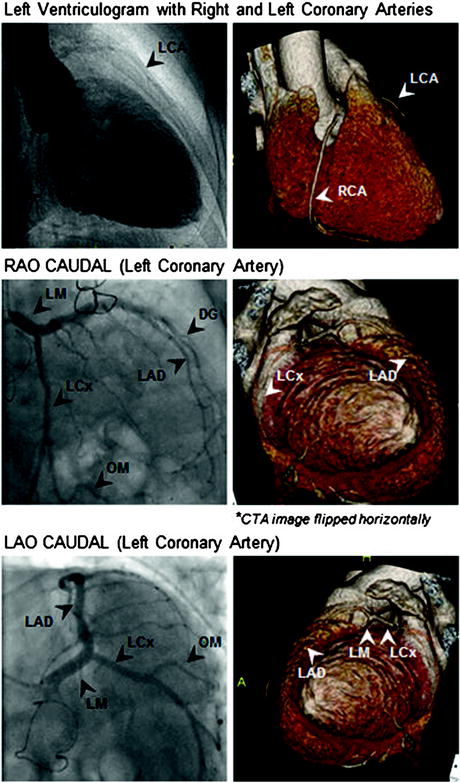
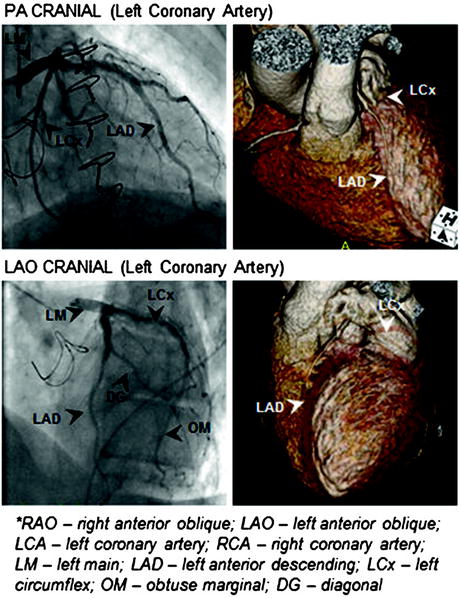
Table 35.2
Angiographic views for specific coronary segments
Vessel | Angulation | Segments |
|---|---|---|
LM | LAO 500/CAU 300 | Bifurcation of the LAD/LCx |
RAO 200/CAU 200 | Proximal and mid LM | |
LAD | LAO 500/CAU 300 | Proximal LAD |
PA/CRA 450 | Mid and distal LAD | |
RAO 300/CRA 300 | Diagonals | |
LAO 500/CRA 400 | Mid and distal LAD | |
LCx | LAO 500/CAU 300 | Proximal, mid, distal LCx, proximal OM |
RAO 200/CAU 200 | Mid and distal LCx, Mid/distal OM | |
PA/CAU 350 | Proximal, mid, and distal LCx, Proximal OM | |
RCA | LAO 300 CRA 200 | Proximal, mid, distal RCA |
RAO 300 | Mid, distal RCA, PDA | |
PA/CRA 300 | Bifurcation of PDA/PLV |
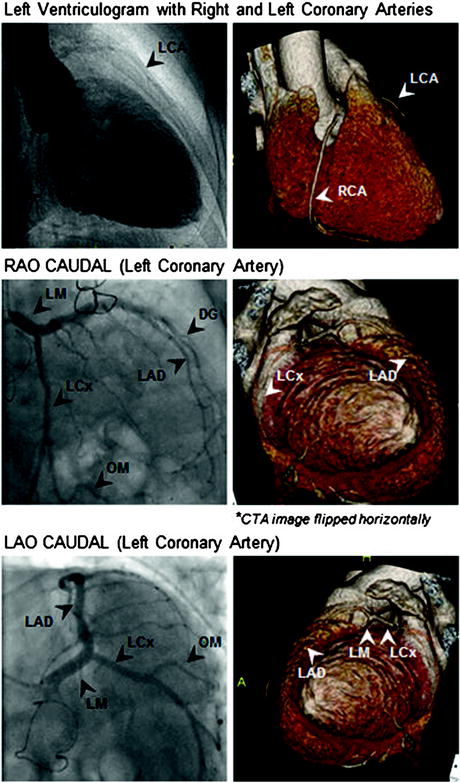
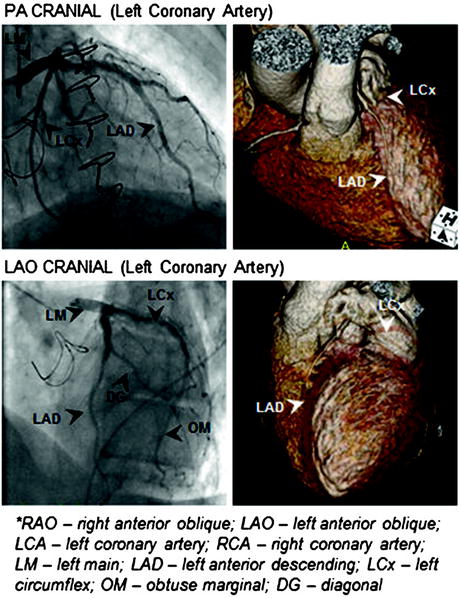
Fig. 35.1
Selected angiographic view with corresponding 3D CTA reconstructions
(f)
Repeat steps (a)–(e) for both right and left coronary arteries, aortocoronary grafts, and mammary grafts (when applicable).
The techniques of fractional flow reserve and intravascular ultrasound provide adjunctive information to diagnostic angiography:
(a)
Fractional Flow Reserve (FFR)—involves the use of a wire with a mounted pressure transducer. Measurements are taken proximal (within the guide catheter placed in the aorta) and distal to a coronary lesion. The fractional flow reserve is the ratio of the mean distal over the mean proximal pressure, taken during times of maximal hyperemia (i.e., adenosine administration). Flow-limiting stenoses have an FFR of ≤0.75–0.80.
(b)
Intravascular Imaging Modalities—involves the use of a catheter mounted with various imaging elements, which allow for interrogation of the vessel and its wall from within the lumen. These technologies include the following:
1.
Intravascular ultrasound (Gray scale IVUS)—uses a catheter mounted with an ultrasound transducer. The tissue resolution is able to differentiate the three layers of a normal artery as well as detect changes related to atherosclerotic plaque. Its use includes determination of reference vessel diameter, cross-sectional area of a stenosis, plaque morphology, adequacy of stent deployment, presence of dissection, etc.
2.
Virtual Histology—adjunct to IVUS, which uses analysis of radiofrequency scatter to determine plaque composition. The various components are given a color coding: fibrous tissue (green), fibro-fatty tissue (light green), necrotic core (red), dense calcium (white).
3.
Optical Coherence Tomography—creates tomographic images using fiberoptics and reflection of infrared light. Produces pictures with better spatial resolution than IVUS, although the depth of penetration is limited. Requires continuous displacement of blood in order to produce images.
4.
Spectroscopy—analyzes plaque composition by using differential tissue absorption of wavelengths of light.
5.
Thermography—detection of “vulnerable” plaque by the increase in temperature associated with macrophage-rich plaque. May be detected by direct measurement of temperature or by infrared imaging.
6 Management Paradigm and Indications as Well as Timing of Treatment
(a)
Acute Coronary Syndrome
1.
ST elevation MI—immediate revascularization, either by the administration of systemic thrombolytics or percutaneous coronary intervention, when available.
2.
Unstable angina/NSTEMI
High risk—early invasive management with diagnostic angiography ± revascularization
Low risk—conservative management, with diagnostic angiography ± revascularization only if recurrent ischemic symptoms or positive stress testing.
(b)
Chronic Stable Angina
1.
Revascularization after failure of optimal medical therapy.
7 Open Operative Choices
Coronary artery bypass and percutaneous coronary intervention are the two major modalities of revascularization. Coronary artery bypass has the advantage of durability, while PCI represents a less invasive modality. In general, CABG is preferred for: