Introduction
Transcranial ultrasound (US) is commonly used to evaluate complications of prematurity, in which case it may be used as a screening tool, or to evaluate infants with seizures, apnea, bradycardia, or falling hematocrit. When used to screen premature infants, it is often performed around day 5 of life, with further imaging performed as needed. Head US is also useful in older infants presenting with macrocephaly, seizures, or an abnormal neurologic examination. It is especially useful in infants suspected of having meningitis, intracranial hemorrhage, or hydrocephalus.
Technique and Normal Anatomy
Head US is a powerful tool for examining intracranial pathology until about age 12 months, at which time bone maturation limits visualization of intracranial contents. Most imaging is performed in the coronal and sagittal planes with a high-frequency (5–7.5 MHz) linear array transducer at the anterior fontanelle. The complete examination consists of six coronal images ( Fig. 7.1 ), beginning anterior to the frontal horns and ending posterior to the lateral ventricles ( Fig. 7.2 ). The sagittal exam ( Fig. 7.3 ) consists of a single midline image and three additional images on each side ( Fig. 7.4 ).




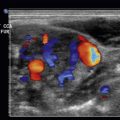
Grayscale and color Doppler interrogation assess the superficial midline structures, including superior sagittal sinus, gyri, and extraaxial spaces ( Fig. 7.5 ). Linear array 7- to 12-MHz transducers enable high-resolution imaging. In addition, axial images may be obtained through the mastoid and posterior fontanelles, which allow for evaluation of the posterior fossa and provide another plane of imaging. The additional dimension helps elucidate pathology and normal structures.

Normal Imaging Appearance
Surface anatomy changes with age. The brain before 24 weeks is smooth, having no sulci other than the Sylvian fissure. At about 24 weeks, the parieto-occipital fissure forms, and the cingulate gyrus develops at 28 weeks. Additional sulci develop until the term neonate’s gyral and sulcal pattern resembles that of an adult.
The lateral ventricles should measure less than 10 mm at the level of the atria, and the third ventricle should measure less than 5 mm transverse. Up to 40% of patients have mildly asymmetric lateral ventricles. The echogenic choroid plexus lies within both lateral ventricles, extending through the foramina of Monroe into the third ventricle. It is not normally seen anterior to the caudothalamic groove in the frontal horn. The choroid plexus may appear lobular or bulbous. However, it should be symmetrical to exclude pathology. Choroid plexus cysts are commonly encountered in normal children. If there are multiple cysts, or if they measure larger than 10 mm, chromosomal abnormalities may be present.
Normal white matter shows uniform, low-level, granular, mild hyperechogenicity predominately brighter than the relatively hypoechoic gray matter, and the transition between white and gray matter is gradual. Artifact or pathology may cause periventricular white matter to appear hyperechoic. When pathologic, the white matter is (1) more echogenic than the choroid plexus and (2) abnormal on both sagittal and coronal images, because an artifact is usually only evident in one plane. The normal cortex consists of three layers: echogenic pia (peripheral), hypoechoic gray matter, and hyperechoic white matter (central). Echogenic hemorrhage or ischemia may obscure these layers.
Midline cerebrospinal fluid (CSF) collections are common until about age 6 months, but residual fluid may be seen in adults. The cavum septum pellucidum is a fluid-filled space between the frontal horns bounded by the leaflets of the septum pellucidum. Fluid is found less often within the cavum vergae, between the bodies of the lateral ventricles. The most posterior (and least often encountered) potential fluid collection is at the level of the pineal gland, in the cavum velum interpositum.
In evaluating superficial para-midline extraaxial hemorrhage or other fluid collections, the configuration of bridging vessels is important. Vessels normally course through the subarachnoid space but do not traverse the subdural space, which is deep to the periosteum. Therefore if extraaxial fluid does not contain coursing vessels, subdural fluid, such as subdural hematoma, should be suspected.
Branching echogenic linear foci may be seen in the basal ganglia ( Fig. 7.6 ). This “lenticulostriate vasculopathy” is a common finding in normal patients and in multiple births. The finding may also be identified in infants with infection (especially cytomegalovirus [CMV]), intrauterine drug exposure, hypoxia, and congenital heart disease.

Pathology
Hemorrhage
Hemorrhage in the brain and in CSF spaces is initially hyperechoic. As blood evolves, it gradually becomes less echogenic as well as more contracted, septated, and nodular. The appearance of evolving hemorrhage depends on location. Intraventricular hemorrhage (IVH) initially layers within the affected ventricle and can eventually extend into the rest of the ventricular system. It may later adhere to the ventricular lining, resulting in ependymal irregularities. Alternatively, it may irritate the ependymal lining, resulting in ependymitis, which appears as smooth, echogenic thickening of the ventricular wall. Parenchymal hemorrhage may undergo necrosis, leading to porencephaly that often communicates with the adjacent ventricle, appearing as a fluid-filled outpouching from the ventricle. In some cases, parenchyma collapses around the space, resulting in focal volume loss. If identified late, it may be difficult to determine the etiology of the porencephaly. Extraaxial hemorrhage demonstrates similar evolution. Minimal hemorrhage may resolve entirely, decreasing in size and becoming anechoic, with subsequent resolution. However, more extensive hemorrhage often demonstrates residual abnormalities.
Hemorrhage in Preterm Infants
The premature infant’s inability to autoregulate cerebral blood flow may result in ischemia and/or hemorrhage in metabolically active areas of the brain. This problem is especially severe in infants weighing less than 1500 g (less than 28 weeks estimated gestational age [EGA]). Hemorrhage may also be encountered in term infants who undergo stress, such as hypoxia, hypothermia, and difficult delivery. Complex interplay between various factors determines the location of hemorrhage, which in premature infants is then graded according to a four-tier system.
Grade I IVH is confined to the germinal matrix, which generates neuronal and glial cells. The germinal matrix initially spans the length of the lateral ventricle, involuting by 35 weeks to occupy only the caudothalamic groove. Subependymal in location, it is hypervascular and therefore especially vulnerable to hypoxia. Larger grade I IVH distorts the contour of the floor of the lateral ventricle. It is initially echogenic ( Fig. 7.7 ) but eventually becomes cystic and then resolves. The presence of cystic foci in this area at birth implies evolution of fetal hemorrhage.

Grade II IVH is located within the ventricular system. It results from blood spreading from the germinal matrix across the delicate ependymal lining into the ventricle (or, in term infants, from the choroid plexus). IVH is initially echogenic ( Fig. 7.8 ), and it may be difficult to differentiate from normal choroid plexus. However, because choroid plexus does not extend into either the frontal horns or the occipital horns, echogenic material within these areas can be assumed to represent hemorrhage. Application of color Doppler is also helpful, because IVH is avascular—unlike choroid plexus. Hemorrhage may be confined to the dependent portion of the ventricle and may be identified as a fluid-filled level in the occipital horn. Like hemorrhage elsewhere, grade II IVH evolves, becoming hypoechoic, contracting, and eventually disappearing. Grade II IVH may be accompanied by ventricular dilatation, but the blood must fill less than 50% of the ventricular volume.

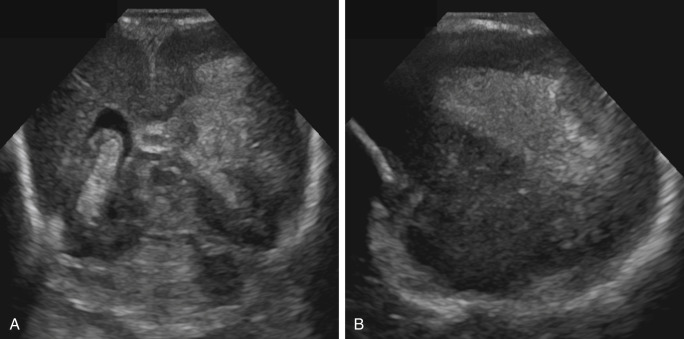
Grade III IVH is also intraventricular in location. However, the affected ventricles are dilated, and echogenic material fills at least 50% of the ventricular volume, almost forming a cast of the ventricle ( Fig. 7.9 ). Diagnosed in the acute phase, grade III IVH should not be confused with posthemorrhagic obstructive hydrocephalus, which may follow a grade II or grade III IVH. Cerebral palsy/developmental delay will be seen in approximately one-half of patients with grade III IVH.

Grade IV IVH extends beyond the germinal matrix into the brain parenchyma. It may result from venous occlusion that can occur if parenchymal draining veins are blocked by either severe grade I IVH or massive ventriculomegaly. It may also result from occlusion of other veins, including the dural venous sinuses. This form of hemorrhage is seen in the periventricular parenchyma ( Fig. 7.10 ). Masslike, it may distort normal structures. Head US may eventually show parenchymal loss at the site of hemorrhage, leading to porencephaly ( Fig. 7.11 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree