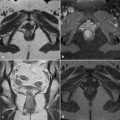
Fig. 24.1
A 56-year-old otherwise healthy male patient with perianal discharge and fistula who was clinically diagnosed by the general surgeon. Axial (a) and coronal (b) T2- weighted, and contrast-enhanced axial fat-saturated Tl-weighted (c) images show a linear T2-hyperintense tract corresponding to a simple intersphincteric fistula located posteriorly to the anal canal left from the midline. Its internal orifice was detected at the dentate line in the 5 o’clock position. Enhancement after intravenous gadolinium along the fistulous tract is consistent with active inflammation
Imaging signs that are generally consistent with inflammatory activity include fluid-like hyperintensity on T2-weighted images and the enhancement of granulation tissue in fistulous walls observed on post-gadolinium contrast T1- weighted sequences (Fig. 24.1). Similarly, abscesses are identified as strongly hyperintense collections on T2 and STIR sequences due to their purulent and debris content, with strong enhancement along the periphery best visualized on fat-suppressed T1-weighted images acquired after intravenous contrast. When present, the unusual gas content is better visualized on CT scans than by MRI (Fig. 24.2). Chronic, inactive fistulas show low signal intensity on T2-weighted and STIR images due to the progressive development of fibrosis [1–3, 7].
In our experience, cryptogenic fistulas, which are most often simple and predominantly located in close proximity to the anal canal, can be conveniently staged following the same classifications proposed for perianal Crohn’s disease, namely, the anatomic scheme of Parks (developed according to surgical findings) and the MRI-based system of St James’ University Hospital [1, 3, 8, 9].
After the initial report by Lunniss et al., in which MRI was shown to be the most accurate method for determining the presence and course of anal fistulas, other authors confirmed the relative inaccuracy of surgical exploration and, instead, the ability of MRI to identify clinically undetected perianal inflammation, thus leading to an altered surgical management of these patients and a reduction of postoperative recurrences [10–12]. Currently, there is overwhelming evidence that the additional value of MRI compared to clinical assessment allows correct surgical planning and improves the clinical outcome [4]. In patients with Crohn’s perianal inflammatory disease, this conclusion has been confirmed by a statistically significant difference, given that Crohn’s-related fistulas tend to be complex, with secondary tracts and multiple abscesses, and are therefore not easily assessed clinically. In these patients, an inaccurate preoperative evaluation often leads to treatment failure, since unrecognized lesions are more likely to be incompletely treated and thus to subsequently recur [1].
A similar benefit from preoperative MRI is not consistently obtained with cryptogenic fistulas since the majority of them are simple, without branching secondary tracts or abscesses [1, 3, 13]. In patients who do not have Crohn’s disease, MRI is therefore recommended to assess recurrent perianal inflammatory disease and clinical suspicion of complex fistulization and/or abscess [3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree