Abstract
Cystic hygroma is the most frequent fetal neck mass in first-trimester ultrasound (US).
It consists of fluid-filled posterior or posterolateral cavities in the neck.
The overall prognosis is poor as there is a high association with chromosomal and structural anomalies, and progression to hydrops and fetal demise.
Rare cases may resolve and show a good outcome.
Keywords
Cystic hygroma, chromosomal abnormalities, fetal neck tumors
Disease
Definition
CH is an abnormality of the vascular lymphatic system, characterized by the development of distended fluid-filled spaces, typically affecting the fetal neck (80% of cases). Based on the presence of septations, it can be classified into septated or nonseptated CH .
Prevalence and Epidemiology
The true incidence of CH is unknown. It has been reported to be 1 : 6000 at birth and 1 : 750 among spontaneous abortions. Data from the FASTER (First and Second Trimester Evaluation of Risk) trial showed an overall prevalence of CH at about 1 : 100, whereas septated CH affects 1 : 285 fetuses in the first trimester.
Etiology and Pathophysiology
CH is frequently associated with other malformations, particularly congenital heart defects (CHD) and chromosomal abnormalities (75% of cases). Some studies suggest that septations predict an increased likelihood of aneuploidies, but this notion has not been confirmed by others. Turner syndrome is the most common associated chromosomal abnormality, affecting approximately 60% of cases. More recent studies suggest a higher prevalence of Down syndrome. Other chromosomal abnormalities include autosomal trisomies, Klinefelter syndrome, partial trisomies, partial monosomies, translocations, and mosaicisms. Genomic microarray analysis may lead to a decrease in the number of undiagnosed genetics disorders when compared with conventional karyotype. Microarrays enable higher resolution, with 22q11.2 microdeletion being one of the most frequently detected imbalance overlooked by conventional karyotype. CH has been related to inherited disorders and malformation syndromes in euploid fetuses ( Table 70.1 ), maternal infection, and drug intake including alcohol, aminopterin, and trimethadione.
|
CH is normally caused by aberrant development of lymphatic vessels, as a consequence of an abnormal or absent connection with the venous system, leading to lymphatic stasis and enlargement of the jugular sacs ( Fig. 70.1 ). Progressive obstruction may lead to thoracic, pericardial, and abdominal effusions. However, if an alternative route of lymphatic flow is established, the distended lymphatic sacs collapse, and the hygroma resolves either completely or showing distended jugular lymph sacs on either side of the fetal neck ( Fig. 70.2 ).

Manifestations of Disease
Clinical Presentation
The prenatal presentation and course of CH is variable. It can resolve spontaneously or progressively affect other fetal structures separate from the neck, such as the pleura, the pericardium, or the abdomen, leading to hydrops fetalis in 75% of cases, which frequently results in fetal demise. In fetuses progressing to term, a large CH may complicate obstetric and perinatal management. A cesarean section may be required to avoid birth dystocia and injury; ex utero intrapartum treatment may be helpful to prevent neonatal asphyxia secondary to difficult airway access. CH rarely regresses spontaneously after birth, and growth of the CH is generally proportional to the growth of the child. Spontaneous infection is present in one-third of cases.
Imaging Technique and Findings
Ultrasound.
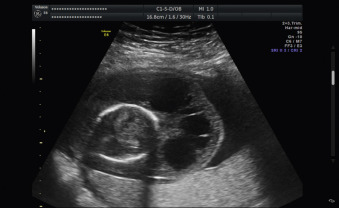
CH develops typically late in the first trimester and is characterized by the presence of posterior or posterior-lateral, fluid-filled cavities in the fetal neck. These cavities are quite variable in size. Nuchal hygromas are frequently bilateral, separated by the nuchal ligament, resembling a complex mass with one or more septa in the center. An axial view of the fetal neck is usually required to make the diagnosis.
Oligohydramnios is present in about two-thirds of cases, thought to be the consequence of hypovolemia and renal hypoperfusion. Amniotic fluid volume can also be increased, especially in cases associated with hydrops fetalis.
CH is associated with other malformations in 60% of cases, including cardiac defects, skeletal dysplasias, genitourinary system abnormalities, congenital diaphragmatic hernia, and central nervous system abnormalities.
Cystic Hygroma Versus Nuchal Translucency.
There is an ongoing debate regarding the differentiation between increased nuchal translucency and CH in the first trimester. It is argued that septations can be seen in all fetuses with increased nuchal translucency, and CH should not constitute a distinct entity in the first trimester.
Magnetic Resonance Imaging.
In late pregnancy, magnetic resonance imaging (MRI) can be useful in prenatal evaluation of airway access and extension of the lymphatic abnormalities to plan an adequate delivery and perinatal management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







