Degenerative disease of the spine is a definition that includes a wide spectrum of degenerative abnormalities. Degeneration involves bony structures and the intervertebral disk, although many aspects of spine degeneration are strictly linked because the main common pathogenic factor is identified in chronic overload. During life the spine undergoes continuous changes as a response to physiologic axial load. These age-related changes are similar to pathologic degenerative changes and are a common asymptomatic finding in adults and elderly persons. A mild degree of degenerative changes is paraphysiologic and should be considered pathologic only if abnormalities determine symptoms. Imaging allows complete evaluation of static and dynamic factors related to degenerative disease of the spine and is useful in diagnosing the different aspects of spine degeneration.
Degenerative disease of the spine is a definition that includes a wide spectrum of degenerative abnormalities. Degeneration involves bony structures and the intervertebral disc, although many aspects of spine degeneration are strictly linked because the main common pathogenic factor is identified in chronic overload. During life the spine undergoes continuous changes as a response to physiologic axial load. These age-related changes are similar to pathologic degenerative changes and are a common asymptomatic finding in adults and elderly persons. A mild degree of degenerative changes is paraphysiologic and should be considered pathologic only if abnormalities determine symptoms. Imaging allows complete evaluation of static and dynamic factors related to degenerative disease of the spine and is useful in diagnosing the different aspects of spine degeneration.
Physiopathology
The causes of age-related and pathologic spine degenerative changes are multiple: traumatic, metabolic, toxic, genetic, vascular, and infectious. Trauma is the main pathologic factor, however, including chronic overload, chronic multitraumatism, and sequelae of acute trauma . The concept of chronic duration trauma has the highest relevance, because degenerative disease of the spine is actually considered the consequence of overuse injury. Abnormal stresses, not sufficient to cause fracture, can be responsible for bone and disc damage if applied for long period. In most cases, the alterations involve the disc and the vertebral body because of the morphologic-functional relationship between these structures .
The distribution of axial load is responsible for the typical localization of spine degeneration. C5-6 and C6-7 levels are involved in most cases, because they are the sites of lordosis inversion. In the dorsal spine degeneration is rare, because this tract is less mobile and less involved in dynamic load. In the lumbosacral tract the most frequently degenerated levels are L4-5 and L5-S1, because they are the sites of the highest dynamic and static load . The functional integrity of spinal curves is involved in degenerative changes. Spinal curves allow optimal redistribution of axial load. When curves are preserved, the spine is 30 times more elastic than a straight structure. If correct spine alignment is lost, an asymmetrical load distribution may cause focal or diffuse spine degeneration.
Because of overlap of imaging findings in age-related changes and degenerative changes, it is usually difficult to define whether abnormalities are paraphysiologic or pathologic. Evaluation of the presence of congruous symptoms and the severity of abnormalities is mandatory for a correct diagnosis .
Progressive involution of the spinal structures begins after the second decade and invariably determines some degree of vertebral and discal degeneration. The first sign of degeneration is the appearance of intranuclear clefts, which are virtually present in 100% of discs after 40 years . Frequently in the adult population asymptomatic disc dehydration and radial fissures can be observed; in elderly persons a slight degree of osteochondrosis and other bony degenerative changes is normal and is considered paraphysiologic. The main difference between people with asymptomatic age-related changes and degenerative abnormalities is the presence of an abnormal axial load distribution in patients with degeneration. Overuse injuries develop pathologically at a younger age in these people than in the healthy elderly population .
Imaging methods: indications and techniques
Imaging plays an important role in the evaluation of degenerative spine. Indication for radiologic examination and technique should be evaluated in every case . When a patient complains of typical back or monoradicular pain, there is no statistical risk in waiting 4 to 6 weeks before performing any radiologic examination. In many cases there is a high possibility of spontaneous pain regression, especially in cases of small acute herniations and extraspinal disorders, such as neuritis and muscular or insertional inflammation. Patients with a history of neoplasm, atypical pain, neurologic deficit, and other local or systemic symptoms should be evaluated earlier.
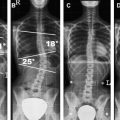
Plain films still play an important role in evaluation of the spine, because the examination is inexpensive and promptly available and gives a wide panoramic view of the spine. Direct information about bony structures can be obtained, and functional information about misalignment and vertebral stability can be obtained with upright dynamic films in flexion-extension and lateral bending .
When findings on plain films do not give sufficient explanation of symptoms, CT or MRI should be performed. If bony abnormalities are diagnosed or highly suspected, CT may be performed for a more complete evaluation. In elderly patients with low back pain or sciatica it is even more commonly accepted as a valid alternative to MRI .
Myelography is rarely performed and reserved for patients with contraindications to MRI or in whom subtle instability is suspected but not confirmed by other examinations. Discography is also reserved for selected patients before some interventional procedures or when the diagnosis of discogenic pain must be confirmed.
For accurate instability evaluation, plain films usually do not offer complete information. The main cause is absent direct visualization of cerebrospinal fluid and nervous structures. Weight-bearing CT and MRI are imaging alternatives. An axial loader is a hydraulic compressor that is placed below a patient’s feet and over the shoulders to apply a variable axial load on the spine. The device can be used with CT or MRI, and it simulates static mechanical forces acting on the spine in the upright position . More recently, dedicated MRI units that allow examination with the patient in the upright position have been realized. These systems have the advantage of determining axial load by gravity, a patient’s weight, and spine morphology without artificial simulation . With the same units, cervical dynamic flexion-extension evaluation is possible.
Imaging methods: indications and techniques
Imaging plays an important role in the evaluation of degenerative spine. Indication for radiologic examination and technique should be evaluated in every case . When a patient complains of typical back or monoradicular pain, there is no statistical risk in waiting 4 to 6 weeks before performing any radiologic examination. In many cases there is a high possibility of spontaneous pain regression, especially in cases of small acute herniations and extraspinal disorders, such as neuritis and muscular or insertional inflammation. Patients with a history of neoplasm, atypical pain, neurologic deficit, and other local or systemic symptoms should be evaluated earlier.
Plain films still play an important role in evaluation of the spine, because the examination is inexpensive and promptly available and gives a wide panoramic view of the spine. Direct information about bony structures can be obtained, and functional information about misalignment and vertebral stability can be obtained with upright dynamic films in flexion-extension and lateral bending .
When findings on plain films do not give sufficient explanation of symptoms, CT or MRI should be performed. If bony abnormalities are diagnosed or highly suspected, CT may be performed for a more complete evaluation. In elderly patients with low back pain or sciatica it is even more commonly accepted as a valid alternative to MRI .
Myelography is rarely performed and reserved for patients with contraindications to MRI or in whom subtle instability is suspected but not confirmed by other examinations. Discography is also reserved for selected patients before some interventional procedures or when the diagnosis of discogenic pain must be confirmed.
For accurate instability evaluation, plain films usually do not offer complete information. The main cause is absent direct visualization of cerebrospinal fluid and nervous structures. Weight-bearing CT and MRI are imaging alternatives. An axial loader is a hydraulic compressor that is placed below a patient’s feet and over the shoulders to apply a variable axial load on the spine. The device can be used with CT or MRI, and it simulates static mechanical forces acting on the spine in the upright position . More recently, dedicated MRI units that allow examination with the patient in the upright position have been realized. These systems have the advantage of determining axial load by gravity, a patient’s weight, and spine morphology without artificial simulation . With the same units, cervical dynamic flexion-extension evaluation is possible.
Radiologic semiotic
Bone structures
Vertebral osteochondrosis
Vertebral endplates bone marrow alterations are a common finding in patients with degenerative spine disease and are strictly associated with disc degeneration. To describe these changes, in 1985, Resnick introduced the concept of vertebral osteochondrosis. This concept is considered an evolutionary process characterized by six phases: (1) disc thinning and hyaline degeneration, (2) chondral microfractures, (3) chondroblastic activation, (4) subchondral reactive neovascularization, (5) bony trabeculae demineralization, and (6) osteosclerosis.
Osteochondrosis is present in 19% of asymptomatic people . It has been found in 50% of people who complain of low-back pain, however . Reversible symptoms can be determined by acute inflammation in type I osteochondrosis, whereas other types are usually asymptomatic. Osteochondrosis is more frequent at levels at which the axial load is higher, such as L4-5 and L5-S1. The relationship with degenerative disc disease is probably caused by multiple factors, including common biomechanical factors, raised mechanical stresses on the endplates induced by disc dehydration, and disc metabolism changes. Other theories consider that the disc is an avascular structure supplied by diffusion from endplate cartilage; therefore, endplate alterations can induce disc trophism defects.
In 1988, Modic et al. proposed a simple classification of vertebral osteochondrosis based on pathologic and imaging aspects. Modic type I (vascular pattern) is a discovertebritis or aseptic spondylodiscitis with bone inflammatory reaction associated with disc degeneration. In this phase, MRI signal of the endplates is low on T1-weighted and high on T2-weighted sequences ( Fig. 1 ). Modic type I can be reversible or can progress . Modic type II (fatty pattern) is characterized by subchondral bone marrow changes with fatty marrow prevalence and demineralization. Endplate MRI signal is high on T1- and T2-weighted sequences ( Fig. 2 ). Modic type III (sclerotic pattern) is the final subchondral osteosclerotic evolution and is characterized by low signal on T1- and T2-weighted sequences ( Fig. 3 ). In this last case, plain films and CT clearly show endplate sclerosis. In almost all cases of vertebral osteochondrosis, MRI shows clear signs of disc degeneration. Sometimes more types are simultaneously found at the same level. In advanced cases, marginal traction osteophytes are frequently found. With MRI, differentiation between Modic types is usually possible. Diagnostic problems can be encountered in differential diagnosis between type I and infectious spondilodiscitis, however. In this case, gadolinium administration is useful, because in type I osteochondrosis disc enhancement is usually absent. In both cases subchondral enhancement can be registered.
Spondylosis
The most typical consequence of age- or load-related degeneration of the vertebral bodies is spondylosis deformans . Spondylosis is found in 60% of women and 80% of men after the age of 50. In elderly people some degree of spondylosis is almost always found and can be considered paraphysiologic. When degenerative alterations are severe or symptomatic, they should be considered pathologic.
The classic sign of spondylosis is osteophytosis. Osteophytes are bony spurs that originate on the anterolateral aspect of the vertebral bodies a few millimeters from the margins of the disc space. They result from weakening and radial degeneration of the fibers of the annulus, with increased vertebral mobility and traction on Sharpey’s fibers determining subsequent osteogenic stimulation. Osteophytes usually follow Sharpey’s fibers. At the beginning they have a triangular shape and extend on the horizontal plane; in the more advanced phase they become hooked and grow vertically. Sometimes osteophytes develop on both sites of a disc space and grow until they fuse together to form a “bridge osteophyte” . Although the most frequent site of osteophytosis is the anterolateral aspect of the vertebra, posterior osteophytes have higher clinical significance because of the possible compression of neural structures. Posterior osteophytes more frequently accompany osteophytes associated with osteochondrosis, microinstability, and disc degeneration. They are characterized by a bulky triangular shape and have a marginal location .
Plain films are adequate for the diagnosis of spondylosis and are helpful for the differential diagnosis between osteophytosis and other bony excrescences with different origin ( Fig. 3 A). CT and MRI can show the osteophytes, but they are useful for identifying other associated degenerative changes and establishing the relationship between bone and neural structures ( Fig. 3 B) .
Schmorl’s node is a common sign of spinal degeneration that is often included in the spectrum of spondylosis, although it has a distinct pathogenesis. A Schmorl’s node is a herniation of the intervertebral disc through the endplate in the vertebral body and is a frequent incidental finding. Schmorl’s nodes are usually asymptomatic; however, in the acute phase they can determine temporary back pain. Imaging shows a central defect of the upper endplate of the vertebral body, often with a clear sclerotic rim. MRI best depicts the relationship between the herniated material and the disc, which is often dehydrated. Acute nodes can be hyperintense on T2-weighted sequences and can enhance after gadolinium administration.
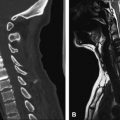
Degenerative changes of the cervical spine typically involve the uncovertebral processes with formation of posterior osteophytes. Associated abnormalities are disc height decrease and disc bulging or protrusion. Plain films are useful for the evaluation of cervical uncoarthrosis; the examination should be completed with oblique projections because osteophytes often determine stenosis of the neural foramina and otherwise could be missed ( Fig. 4 ). MRI is required to identify disc herniations that can determine spinal canal stenosis and possible compressive myelopathy ( Fig. 5 ).
Facet joints
Facet joints are frequently involved in osteoarthritis. The typical imaging findings are joint space narrowing, subchondral sclerosis and cysts, osteophytosis, ligament thickening, intra-articular vacuum and joint fluid. Osteophytes can involve the whole facet that appears hypertrophic; however, they more often involve the articular surface of the superior facet of the lower vertebra, because the inferior is covered by the ligamentum flavum. Plain films can show the presence of degenerative changes; however, the anatomic complexity of this region requires CT or MRI for a complete evaluation of the degenerative process. Severe facet osteoarthritis can determine lateral recess and neural foramen stenosis; less frequently, canal stenosis can be observed. CT is more accurate for determining bony abnormalities, but MRI more clearly shows neural structures and soft tissues ( Fig. 6 ).
Facet joint osteoarthritis often leads to vertebral instability because of sagittal orientation of the articular rim and degenerative weakening of the capsule and the periarticular structures . Abnormal orientation of the articular rim can be sometimes congenital and rarely asymmetric. In these cases facet joint osteoarthritis and instability develop earlier. Facet instability leads to anterior subluxation of the inferior facet of the upper vertebra or degenerative spondylolisthesis. Weight-bearing MRI can be useful in selected cases to diagnose facet joint instability, which appears as joint space widening and anterior slippage of the lower facet. Weight-bearing MRI also can show increased thickening of the ligamentum flavum during axial load caused by ligament laxity. This process can determine appearance of a stenosis only during axial loading . The role of facet joints in back pain is often difficult to assess, because symptoms can be unspecific and imaging findings of degeneration are common . In selected cases, nerve block or facet joint steroid and anesthetic injections are useful for diagnostic and therapeutic purposes, because they reduce pain for patients who have facet syndrome .
Rarely, patients with hyperlordosis and severe degenerative changes of the facet joints can develop Baastrup disease. This condition is characterized by interspinosus contact, with resulting inflammatory reaction and possible formation of pseudoarticulation.
Sometimes facet joint degeneration is complicated by synovial cysts. These formations originate from the joint and can keep or lose the connection with the joint. When they develop on the intracanalicular side of a joint, they can have compressive effects ( Fig. 6 B). Cysts can contain synovial serous fluid, more gelatinous material, air, or blood. The diagnosis and the connection with the joint can be confirmed by percutaneous CT or fluoroscopic-guided aspiration. After aspiration, the cyst can be filled with steroid and anesthetic and can be broken for curative purposes.
Facet joint synovitis has been recognized as a possible cause of facet syndrome. Typical MRI findings are intra-articular or pericapsular high signal on T2-weighted sequences and enhancement after contrast agent administration ( Fig. 7 ) .