DEVELOPMENTAL ABNORMALITIES OF THE EXTERNAL AND MIDDLE EAR (AURAL ATRESIAS) AND CRANIAL NERVE VII
KEY POINTS
- Computed tomography is critical to medical decision making in developmental abnormalities of the external and middle ear.
- Reports must be logically constructed and comprehensive, anticipating all anatomic and pathologic abnormalities that might lead to altered treatment plans.
Development of the inner ear from the primitive otocyst is separate from that of the middle and external ear, which come from the first and second branchial arches. The structures involved in each phase of development should be evaluated in the clinical context. Patients suspected of having congenital defects will usually present in two distinct groups: those with external canal atresia with obvious canal stenosis and/or a deformed pinna and those with potential inner ear anomalies with sensorineural hearing loss. A combined inner and external ear anomaly reflects injury to the otocyst and the branchial apparatus usually requiring a chromosomal insult, syndromic relationship (Chapter 107), or severe multicentric early process such as rubella infection during gestation.
The written report of findings in anomalies of the temporal bone and cochleovestibular nerve should reflect the developmental background of these anomalies. Such a report must include systematic documentation of the entire auditory pathway as seen on either computed tomography (CT) or magnetic resonance imaging (MRI), and a specific statement for each structure in this linkage should appear in every report. A reasonable approach to the general report format is to trace the sound in, essentially vibrating air, from the outside to the brain stem and then follow the facial nerve back out since the position of the latter might have a treatment impact. For the purposes of discussion, the suggested report content can be relatively conveniently divided into three basic categories:
- Those related to external auditory canal (EAC; aural) atresia/middle ear anomalies discussed in Chapter 105
- Those related to possible inner ear and cochleovestibular anomalies discussed in Chapter 106
- Those that might impact cochlear implant candidates discussed in Chapter 136
For the external canal, middle ear, and facial nerve, the report should emphasize the conductive part of the pathway but must also consider the remaining sensorineural pathway. Facial nerve development is at the interface of these two functional units of hearing, but consideration of its anomalous development is most linked to disorders of the external canal and middle ear, where it can dramatically affect treatment options.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The EAC arises from the first branchial groove as it accompanies the first branchial arch mesenchyme.1 The middle ear and eustachian tube are formed from the first branchial pouch arising from endoderm of the primitive foregut. They join at the tympanic membrane. Consequently, the epithelium of the external canal and outer layer of the tympanic membrane is squamous epithelium, while the middle ear is lined by respiratory epithelium. Ectodermal squamous tissue rests remaining within the middle ear account for the occasional formation of congenital middle ear cholesteatomas. First, branchial arch mesenchyme differentiates into both the cartilaginous and osseous portions of the EAC. The developing middle ear expands to surround the developing ossicular chain and creates “mesenteric” folds that can be abnormal, thick, and calcific in congenitally malformed ears. The cartilage anlage of the first branchial arch is called the Meckel cartilage and that of the second branchial arch is called the Reichert cartilage; these contribute to the formation of the mid face and mandible as well as the ossicles. Thus, branchial arch anomalies include a spectrum of developmental disorders ranging from ossicular fusion anomalies to severe deformities affecting the face and mandible, especially the formation and orientation of the temporomandibular joint.
Ossicular development is complex. The malleus head and neck, malleal ligaments, and tensor tympani muscles, as well as the incus body and short process, are all derived from the first branchial arch. The anterior or short process of the malleus develops in conjunction with the tympanic membrane and tympanic ring. The long processes of the malleus and incus, the stapes suprastructure, and the stapedius muscle are derived from the second branchial arch. The stapes foot plate arises from the primitive neural ectodermal otocyst along with the membranous labyrinth. Ossicular anomalies include a combination of malalignments, suspensory ligamentous thickening, and ossicular fusions to both adjacent ossicles and to middle ear walls. The malformed malleus and incus are most commonly fused to the atretic plate, where it forms the lateral epitympanic wall. Lesser anomalies include failure to form the normal diarthrodial joints of the malleoincudal and incudostapedial articulations and atretic, missing, or otherwise deformed components of the ossicles, particularly of the stapes crura.
EAC anomalies present as a spectrum of abnormalities ranging from focal canal stenosis to complete canal atresia. These may be isolated and are more frequently associated with anomalies extending to involve the tympanic ring, tympanic membrane, and ossicles. Fusion of the malleus to the atretic plate is common because the anterior process of the malleus differentiates from the primitive tympanic membrane. Pinna abnormalities that produce various degrees of microtia are frequently seen in conjunction with EAC anomalies.
CONGENITAL CHOLESTEATOMA
Congenital cholesteatoma (congenital epidermoid cyst) may be associated with congenital aural atresias likely beginning as embryonic rests of squamous epithelium misplaced during temporal bone development. In patients with total atresia, congenital cholesteatoma and mastoiditis or evidence of acute otitis media are probably the only sure indications for surgery. Congenital cholesteatomas are usually isolated findings of retrotympanic pearly masses. When associated with atresia, they are more common with the less severe forms of aural atresia. It is sometimes difficult to discern congenital from acquired cholesteatoma in some cases.
All aural atresias, in which the tympanic membrane cannot be visualized, should be imaged to exclude the presence of a congenital cholesteatoma. This should be done at some time during early childhood. If a soft tissue mass or apparent mucosal thickening is seen, a follow-up scan must be done in about 1 year on the presumption that such findings represent a cholesteatoma.
Applied Anatomy
A detailed and complete knowledge of normal temporal bone anatomy as presented in Chapter 104 is required for evaluation of congenital anomalies. The most common key elements in this evaluation include the following:
- Soft tissues: Parotid gland and capsule attachments to the EAC, mandible, and temporomandibular joint
- Temporal bone: EAC, roof of middle ear and mastoid, ossicles and inner ear, and internal auditory canal (IAC)
- Facial nerve: Brain stem to its stylomastoid foramen exit and beyond
- Cochleovestibular nerve: Brain stem nuclei to points of end organ innervation
- Vascular structures: Internal carotid artery, jugular vein and bulb, and major dural venous sinuses of the posterior fossa
IMAGING APPROACH
Techniques and Relevant Aspects
In general, CT and MRI for this indication always require the highest possible spatial resolution, sometimes needing to balance that against required low-contrast resolution. CT is used almost exclusively in anomalies of the external canal and middle ear and for this indication normally suffices to screen for inner ear anomalies and complicating factors such as congenital cholesteatoma or coincidental inflammatory middle ear and mastoid disease.
The foundational technical factors at work in developing appropriate high-resolution data sets for these purposes are discussed in detail in conjunction with general CT and MRI imaging parameters in Chapters 1 through 3.
General imaging parameters used in this region of interest are presented in Appendixes A and B and are discussed in Chapter 104.
Imaging in aural atresia is typically delayed until surgical auricular reconstruction is planned, usually after 5 years of age.
Pros and Cons
CT is used in the vast majority of cases because the critical information for medical decision making lies primarily in the bony anatomy.
MRI may be used in very complex cases when there may be associated inner ear abnormalities and the status of the proximal seventh and eighth cranial nerves is in question. MRI might also be useful to determine whether middle ear or mastoid soft tissue changes more likely are due to chronic inflammation or acquired or congenital cholesteatoma. In potentially syndromic disorders, it can also be used to look for associated anomalous brain development and other intracranial and cranial facial soft tissue abnormalities.
Ultrasound is not used in this anatomic area of interest.
Radionuclide techniques are not used in this area except in rare cases where cisternography might be used to confirm a cerebrospinal fluid leak, as discussed in Chapter 5 and elsewhere in this section.
Catheter angiography has essentially no role, with magnetic resonance (MR) angiography and CT angiography capable of defining vascular anatomy or anomalies whenever necessary.
SPECIFIC DISEASE/CONDITION
Developmental Abnormalities of the External Auditory Canal, Middle Ear, and Facial Nerve
Etiology
Aside from those due to known syndromes, developmental abnormalities of the EAC, middle ear (congenital aural atresias), and facial nerve are likely due to spontaneous chromosomal abnormalities that may be linked to gestational infections or toxicity but usually have no truly identifiable cause.
Prevalence and Epidemiology
Congenital aural atresia or stenosis occurs in about 1 in 11,000 births.2 Unilateral atresia is four times more common than bilateral atresia. Minor malformations involve fixations and isolated dysplasia of the ossicular chain and malformations of the round and oval window regions with a normal tympanic membrane and EAC. Their incidence is very small. These are largely sporadic conditions but may be syndromic.
Clinical Presentation
Patients will often present with various degrees of microtia. Those with a normal-appearing ear as well as more severe forms will present with conductive hearing loss.
Pathophysiology and Patterns of Disease
The spectrum of aural atresias presents myriad variations with regard to the specifics of the anomalous anatomy. No two patients have the same exact findings; when bilateral, the changes are usually asymmetric but generally involve the same structures, just to a different degree. In general, there will be some degree of the following findings in gross atresias, but not all will present:
- Deformity of the pinna (Fig. 105.1).
- Narrowing, foreshortening, or other distortion of the cartilaginous portion of the EAC (Fig. 105.1).
- Stenosis (≤4 mm) or atresia of the bony EAC with a fibrous or bony atretic plate of variable thickness (Fig. 105.2).
- Some reduction in size of one or more of the components of the middle ear space (Figs. 105.3 and 105.4).
An air-containing middle ear cavity with preserved function of the eustachian tube is favorable for hearing restoration. However, the size of the tympanic space is frequently diminished in aural atresia. Most often, the size of the hypotympanum is reduced, while the mesotympanum shows at least a small residual cleft. The epitympanum is affected least often. If the width of the middle ear cavity, as measured from the promontory to the lateral wall, is <3 mm, it is generally considered to be inadequate for surgery.3 The bony eustachian tube can either be dysplastic, narrow, or excessively enlarged.
- Anomalous development of the ossicles usually with some degree of incorporation into the lateral wall and/or roof of the tympanic cavity (Figs. 105.5–105.7).
Abnormalities of the manubrium are a constant finding. The manubrium is short and deformed in EAC stenosis. In aural atresia, the manubrium is absent and the neck of the malleus is often fused to the atresia plate. The most common ossicular anomaly is fusion of the malleus and incus in the attic. The long process of the incus usually shows axis rotation or may be dysplastic. If the malleoincudal articulation is affected, the incudostapedial articulation is often dysplastic. The stapes is not as frequently involved as the rest of the ossicular chain, but its development is a very important factor for successful operation. Since there is an intimate relationship in the embryologic development of the stapes foot plate, the tympanic segment of the facial nerve, and the oval window, the radiologist must have a high index of suspicion for a malpositioned or exposed horizontal facial nerve and congenital absence of the oval window.4
- Abnormal position of the facial nerve, most typically its descending segment that travels more anteriorly and laterally than usual, possibly with multiple branches, some free within the middle ear cavity, that may go through the atretic plate. The tympanic segment may be displaced inferiorly, overlying the oval window, and is often dehiscent. In some cases, the tympanic segment shows an extremely anterior course, straight down from the first genu. The labyrinthine segment rarely shows anomalies (Fig. 105.8).
- Abnormal height of the roof of the mastoid and lack of development in general (Figs. 105.9 and 105.10). The mastoid process is often hypoplastic or aplastic, in turn affecting the temporomandibular joint. The space between the facial nerve as it extends caudally through the atretic plate and the tegmen should be at least 1 cm for a safe surgical approach.
- Acquired middle ear disease is sometimes related to abnormal development of the protympanum and bony eustachian tube (Fig. 105.10).
- Congenital or acquired cholesteatoma (Fig. 105.11). Membranous atresia or a tight stenosis may prevent normal migration of keratinizing or squamous epithelium, resulting in a cholesteatoma.
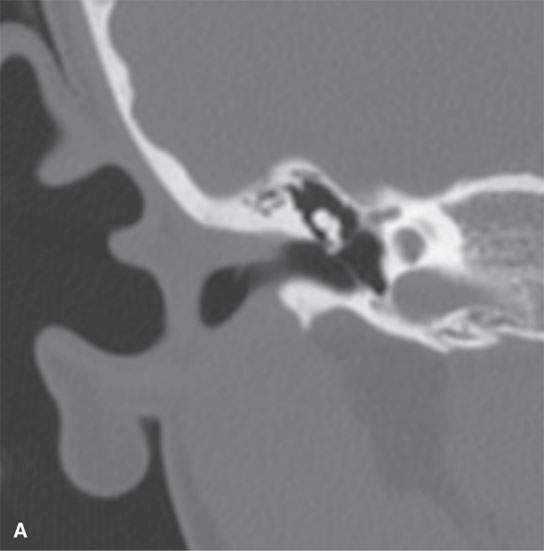

FIGURE 105.1. A,B: Unilateral deformity of the pinna and cartilaginous portion of the external auditory canal (EAC) as seen on coronal computed tomography. The left EAC shows a distinctly more angulated course, sloping upward, than on the normal right ear (A). Note also the widening of the petrotympanic fissure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








