KEY WORDS
Acetabular Dysplasia. Abnormal development of the acetabulum tissue.
Acetabular Labrum (Limbus Cartilage). Cartilaginous ring surrounding the periphery of the acetabulum that aids in stabilizing the femoral head within the acetabulum.
Acetabulum. Cup-shaped bony structure formed by the ilium, ischium, and pubis that articulates with the femoral head.
Clicky Hip. As the hip joint is dislocated and reduced, a “click” is heard as the femoral head passes over the posterior labrum of the acetabulum.
Congenital Hip Dislocation. Displacement of the hip joint existing from or before birth. The term is interchangeable with developmental dysplasic hip.
Developmental Dysplastic Hip. Displacement of the hip joint caused by the femoral head moving out of the socket, or the socket not having formed properly. The term is interchangeable with congenital hip dislocation, although developmental dysplasic hip is more commonly used at the present time.
Dislocatable Hip. The femoral head displaces from the acetabulum during certain stress maneuvers of the leg but returns to its normal position spontaneously once the pressure is released.
Fovea. Indentation (pit) on the femoral head, which provides attachment for the ligamentum teres.
Gluteus Medius Muscle. This muscle originates from the ilium and inserts at the greater trochanter. It stabilizes the hip.
Greater Trochanter. Bony process arising from the superolateral portion of the proximal femoral shaft.
Ilium. Bone that forms the superior portion of the acetabulum.
Intertrochanteric Crest. Prominent ridge between the greater and lesser trochanters on the posterior portion of the proximal femoral shaft.
Ischium. Forms the inferoposterior portion of the acetabulum.
Lesser Trochanter. Bony process located at the posteromedial portion of the proximal femoral shaft.
Ligamentum Teres. Ligament that extends from the edges of the fovea on the femoral head to the edges of the acetabular notch; it contains a branch of the obturator artery.
Ossific Nucleus or Ossification Center. Bony formation appearing as early as 4 weeks of age in the center of the femoral head.
Pavlik Harness. Corrective harness that supports the hips in flexion and abduction without force.
Pubis. Bone that forms the inferoanterior portion of the acetabulum.
Subluxation. Incomplete displacement of the femoral head from the acetabulum during certain stress maneuvers of the leg.
Triradiate Cartilage. Cartilaginous connection between the ilium, ischium, and pubis of the acetabulum.
The Clinical Problem
Ultrasound is widely used for assessing developmental dysplasia of the neonatal hip because it effectively depicts the soft tissue and cartilaginous structures and has the advantage that dynamic movement of the hip joint can be examined. Alternative imaging techniques include:
![]() Radiography: The traditional diagnostic modality used for developmental hip dysplasia. It is not reliable in neonates, as the hip is still a cartilaginous structure that has not yet ossified.
Radiography: The traditional diagnostic modality used for developmental hip dysplasia. It is not reliable in neonates, as the hip is still a cartilaginous structure that has not yet ossified.
![]() Arthrography: Demonstrates hip anatomy; it is rarely used because it is invasive and sedation or a general anesthetic are needed.
Arthrography: Demonstrates hip anatomy; it is rarely used because it is invasive and sedation or a general anesthetic are needed.
![]() Computed tomography: Is helpful in infants confined to a cast; it is not routinely used in diagnosing congenital hip dislocation because it is nondynamic, results in gonadal radiation exposure, and requires sedation.
Computed tomography: Is helpful in infants confined to a cast; it is not routinely used in diagnosing congenital hip dislocation because it is nondynamic, results in gonadal radiation exposure, and requires sedation.
![]() Magnetic resonance imaging: Provides exquisite anatomic detail of the soft tissue, cartilage, and bony structures with no radiation exposure,but requires sedation, has a long scanning time, is expensive, and is not dynamic.
Magnetic resonance imaging: Provides exquisite anatomic detail of the soft tissue, cartilage, and bony structures with no radiation exposure,but requires sedation, has a long scanning time, is expensive, and is not dynamic.
Ultrasound is the first tool used because:
1. One can differentiate the cartilage components of the acetabulum and femoral head from other soft-tissue structures.
2. The relationship of the femoral head position to the acetabulum can be seen.
3. A dynamic study of the hip position including the application of stress maneuvers to assess joint laxity can be performed.
4. Fluid in the joint space can be assessed.
5. No ionizing radiation is used.
6. No contrast media is required.
7. It is inexpensive.
8. No sedation is required.
9. The infant hip is easily accessible, and comparable follow-up studies can be performed even when corrective devices such as traction, a cast, or a Pavlik harness are in place.
The cause of developmental hip dysplasia unknown, but:
1. Females are affected substantially more frequently than males (5:1). This gender difference is thought to be due to the maternal hormonal effect of estrogen, which increases muscle laxity (helping with childbirth). This effect is reduced by male hormones.
2. The left hip (60%) is more often involved than the right hip (20%) or both hips (20%).
3. Developmental hip dysplasia is more common in breech presentations; this is thought to be due to extension of the fetal knees and hyperflexion of the fetal hip while the fetus is in the breech position.
4. Developmental hip dysplasia is more common when there has been oligohydramnios.
5. Hip dysplasia is more common in children with a family history of developmental dysplasia of the hip (e.g., a parent or sibling).
6. Firstborns are affected more often.
7. Neuromuscular abnormalities (e.g., spina bifida and arthrogryposis), congenital torticollis, skull-molding deformities, and certain congenital foot deformities have a higher incidence of developmental hip dysplasia.
8. Caucasians, certain Native American tribes, Scandinavians, and people from some regions of Japan appear to have a higher incidence of congenital dislocation of the hip as compared to people of African or Asian descent.
Clinical Examination Technique
The clinical examination remains the principal screening tool for detecting developmental hip dysplasia and is most valuable when performed with experienced hands on a passive infant. The clinical examination usually consists of the Ortolani and Barlow maneuvers.
1. The examiner holds the infant’s thigh and positions his or her middle finger over the greater trochanter.
a. The Ortolani test is performed by abducting and lifting the thigh to bring the femoral head into the acetabulum. The examiner will sense reduction by a palpable “click” if the hip was in fact, dislocated.
b. The Barlow test is performed by adducting the hip with gentle downward pressure. Dislocation is felt by the examiner as the femoral head slips out of the acetabulum over the posterior labrum. The diagnosis can be confirmed with the Ortolani test.
Certain ancillary signs may be seen with congenital hip dislocation, although they are not conclusive:
1. Asymmetric skin folds, both gluteal and thigh
2. Limited abduction of less than 45 to 60 degrees often noticed during a diaper change
3. Poor movement of the affected limb
4. Limb maintaining a position of outward rotation
5. Shortening of the femur
Early diagnosis and treatment of congenital hip dislocation is essential for proper hip joint development. The most favorable time for sonographic screening evaluation appears to be 6 weeks of age, for the following reasons:
1. Newborns may have minimal subluxation, which corrects itself without intervention by 4 weeks of age.
2. Orthopaedic surgeons like to begin treatment by 2 months of age.
3. Some dysplasia may not occur until after the newborn period.
An ultrasound examination of both hips will be requested in the following circumstances:
1. When the clinical examination is indeterminate
2. To confirm a clinical impression of dislocation or “clicky hip” and to quantitate severity
3. As follow-up to show proper migration of the femoral head with treatment
Anatomy
ACETABULUM
![]() The newborn pelvic girdle is made up of two coxal bones, each with three components: the ilium, pubis, and ischium. The ilium is the superior component, the pubis is located in the inferoanterior position, and the ischium is inferior and posterior. The triradiate cartilage is a useful landmark that connects the ilium, ischium, and pubis (Figs. 38-1 and 38-2). Sonographically, this cartilage appears hypoechoic and allows penetration of the sound beam. The triradiate cartilage becomes ossified in adulthood and fuses with the ilium, ischium, and pubis to form the acetabulum. Sonographically, these bony segments appear echogenic and cast an acoustic shadow.
The newborn pelvic girdle is made up of two coxal bones, each with three components: the ilium, pubis, and ischium. The ilium is the superior component, the pubis is located in the inferoanterior position, and the ischium is inferior and posterior. The triradiate cartilage is a useful landmark that connects the ilium, ischium, and pubis (Figs. 38-1 and 38-2). Sonographically, this cartilage appears hypoechoic and allows penetration of the sound beam. The triradiate cartilage becomes ossified in adulthood and fuses with the ilium, ischium, and pubis to form the acetabulum. Sonographically, these bony segments appear echogenic and cast an acoustic shadow.
![]() The acetabulum is a cup-shaped structure that articulates with the femoral head as a ball-and-socket joint. The articular surface in the acetabulum is horseshoe shaped and smaller than the articular surface of the femur.
The acetabulum is a cup-shaped structure that articulates with the femoral head as a ball-and-socket joint. The articular surface in the acetabulum is horseshoe shaped and smaller than the articular surface of the femur.
![]() The acetabular labrum, sometimes called the limbus cartilage, is a cartilaginous ring that surrounds the periphery of the acetabulum and forms an extension of the acetabular roof. The labrum is rounded off at the superior and posterior positions of the acetabulum. It narrows the acetabulum and increases its depth, thus supporting and stabilizing the femoral head within the acetabulum. The labrum is best seen in the coronal view as a triangular structure adjacent to the ilium and superolateral to the femoral head. The acetabular labrum is composed of hyaline cartilage with a fibrocartilaginous tip; sonographically, it appears mainly hypoechoic except for the echogenic fibrocartilaginous tip.
The acetabular labrum, sometimes called the limbus cartilage, is a cartilaginous ring that surrounds the periphery of the acetabulum and forms an extension of the acetabular roof. The labrum is rounded off at the superior and posterior positions of the acetabulum. It narrows the acetabulum and increases its depth, thus supporting and stabilizing the femoral head within the acetabulum. The labrum is best seen in the coronal view as a triangular structure adjacent to the ilium and superolateral to the femoral head. The acetabular labrum is composed of hyaline cartilage with a fibrocartilaginous tip; sonographically, it appears mainly hypoechoic except for the echogenic fibrocartilaginous tip.
![]() The superior portions of the femur—the femoral head, femoral neck, and greater and lesser trochanters—are cartilaginous in the neonate and can be well visualized by ultrasound.
The superior portions of the femur—the femoral head, femoral neck, and greater and lesser trochanters—are cartilaginous in the neonate and can be well visualized by ultrasound.
1. The femoral head appears as a hypoechoic circle with smooth borders containing fine-stippled echoes spread evenly throughout. The fovea (pit) of the femoral head provides attachment for the ligamentum teres.
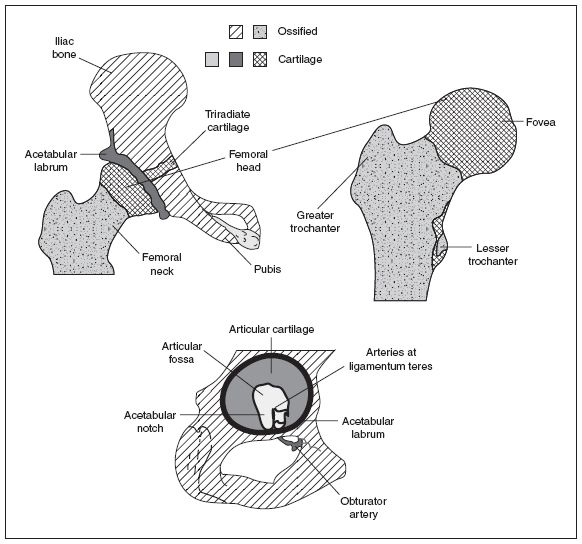
Figure 38-1. ![]() Anatomic drawing of the acetabulum and femur.
Anatomic drawing of the acetabulum and femur.
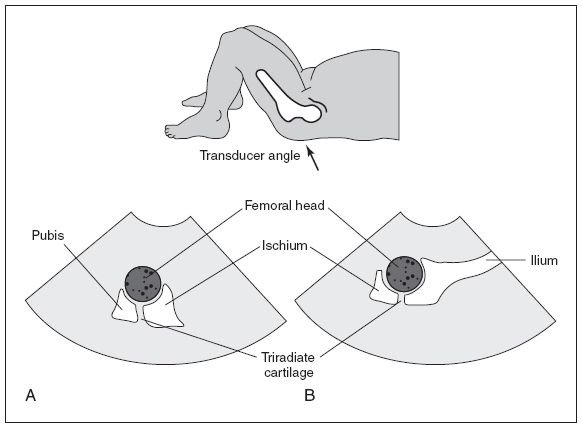
Figure 38-2. ![]() Sketch of an infant showing the transverse (A) and coronal (B) approach.
Sketch of an infant showing the transverse (A) and coronal (B) approach.
2. The ligamentum teres runs from the edges of the fovea on the femoral head to the edges of the acetabular notch. It contains the branch of the obturator artery, which supplies blood to the femoral head.
3. The echogenic femoral neck angles medially, superiorly, and anteriorly as it tapers toward the femoral head.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


