DEVELOPMENTAL LESIONS: EPIDERMOID, DERMOID, TERATOMAS, HAMARTOMAS, AND ABERRANT TISSUE
KEY POINTS
- Developmental abnormalities should be referred to by their proper names.
- A correct understanding of these conditions leads to better imaging reports and medical decision making.
- The imaging morphology of these developmental conditions is often explained by their tissue of origin.
- These conditions are generally found both intracranially and extracranially throughout the head and neck regions as well as in other parts of the body.
- While more common in children, these conditions frequently initially manifest clinically well into adult life.
- When a developmental anomaly is encountered, one must always consider that there might be others and that they may be syndromic.
Understanding the normal variations seen in growth and development of the head and neck region helps in interpreting any study. In each region of the head and neck, there are conditions that result from disordered development. These include dysplasia, dysraphism, heterotopic tissue, and syndromes with one or more of these elements. Congenital cysts such as those of the branchial and thyroglossal apparatus, dermoid cysts, and venolymphatic malformations all present as masses most of the time. The same is true of tissues or structures located abnormally, such as a nasal encephalocele or an aberrant carotid artery. All of these result from disordered development.
The problem caused by congenital abnormalities and anatomic variations can range from insignificant, such as a high jugular bulb, to catastrophic when a severe craniofacial dysplasia is encountered. Some knowledge of their cause, natural history, and associated lesions is necessary for interpretation of imaging studies and decisions for further imaging and other clinical evaluation. The basic embryology of these disorders provides insights that may lead to better image interpretation and an improved understanding of important related clinical issues. Abridged, correlating embryology is included in site-specific discussions of developmental disorders as it is appropriate. Nonvascular developmental abnormalities that appear at more than one head and neck site or are illustrative of the concepts in this discussion are presented here in more general terms. For information regarding vascular developmental abnormalities, refer to Chapter 25.
While ultrasound can be used to image these lesions, computed tomography (CT) and magnetic resonance imaging (MRI) are the mainstay for showing their nature and extent. In general, ultrasound will show a mass that may have any combination of cystic and solid components, high- and low-flow vessels, manifestations of calcification, ossification and other highly refractory tissue like hair.
Treatment of epidermoids, dermoids, teratomas, and hamartomas is surgical or just observation. Prognosis is good when gross total resection is possible and accomplished when it is necessary.
EPIDERMOID AND DERMOID CYSTS
Clinical Perspective and Pathology
Epidermoid cysts are of ectodermal origin, lined solely by stratified squamous epithelium.1 The lining of dermoids includes skin appendages, such as hair follicles, sebaceous glands, and sweat glands, all of which are also of ectodermal derivation.1,2 Both cysts arise from inclusion of epithelial elements in an abnormal location during embryogenesis. When the central nervous system is involved, this most likely occurs between the third and fifth week of fetal life at the time of neural tube closure.2,3 This accounts for the tendency of dermoid cysts to be midline lesions with an associated bone and/or skin defect and frequently the threat of a communication to the central nervous system (Fig. 8.1).4


FIGURE 8.1. A: T1-weighted contrast-enhanced magnetic resonance (MR) showing an inflamed nasal dermoid cyst (C) extending through the anterior skull base but not connected to the brain. B: T2-weighted MR image showing the cyst (C) and tract components more completely.
Dermoid cysts of the head and neck probably account for <10% of dermoids at all sites in the body. In the extracranial head and neck region, about 50% will be orbital (Fig. 8.2), 25% will arise in the floor of the mouth and submandibular and submental spaces (Fig. 8.3); 13% will be nasal; and the remainder will be scattered between the lip, palate, neck, and frontal and occipital regions (Fig. 8.1). Intracranial dermoids are uncommon compared to epidermoids (Fig. 8.4), often occurring in the midline in the posterior fossa and involving the vermis, fourth ventricle, and vallecular regions.1,5

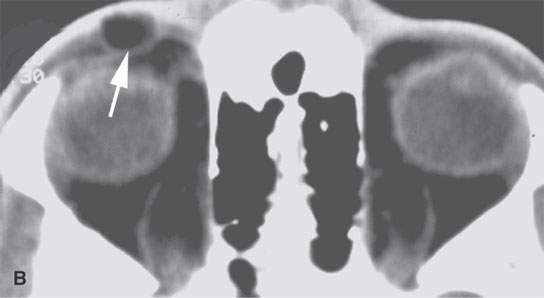
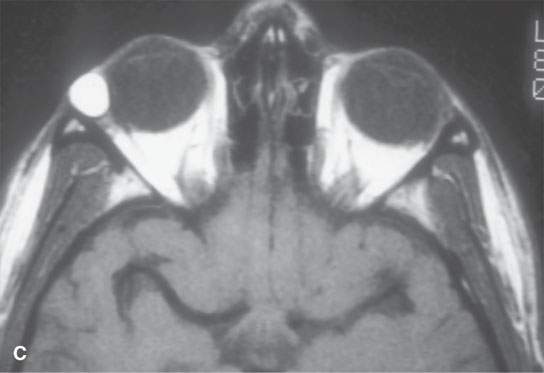
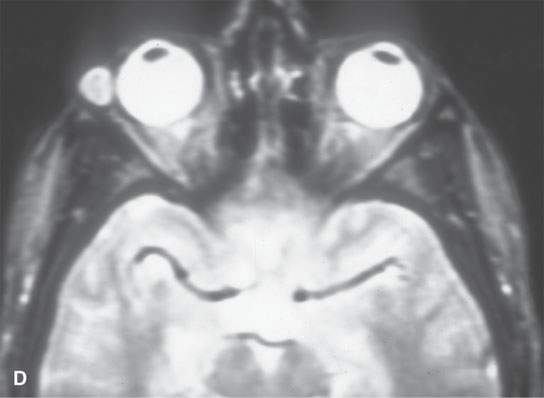
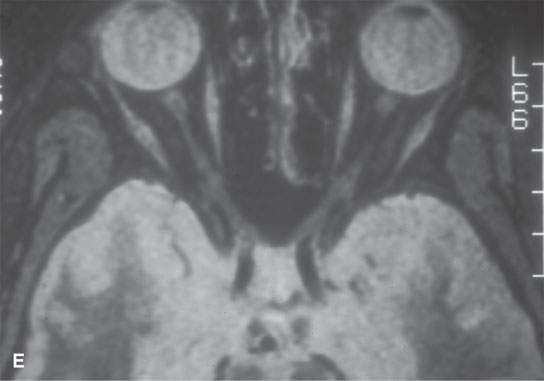
FIGURE 8.2. A: Contrast-enhanced computed tomography (CT) of a complex orbital dermoid with a small calcification (arrow). B: Non–contrast-enhanced CT of a small orbital dermoid (arrow) that is predominantly fatty. C: T1-weighted non–contrast-enhanced magnetic resonance (MR) shows bright signal in an orbital dermoid cyst. D: T2-weighted MR of the patient in (B) shows the cyst is less intense than fat. E: Short T1 inversion recovery (STIR) MR of the patient in (B) and (C) shows signal in the dermoid to be nulled, so it could be fat or some other tissue—the STIR image is therefore ambiguous with regard to cyst content.
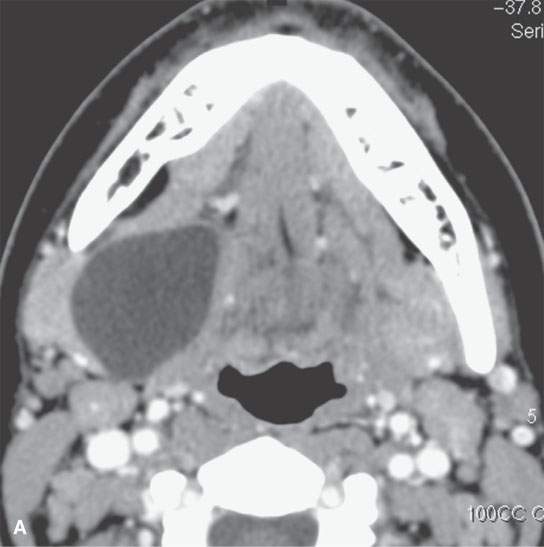
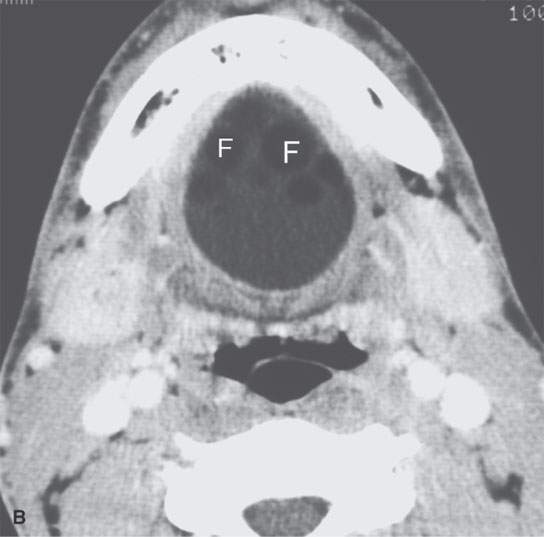
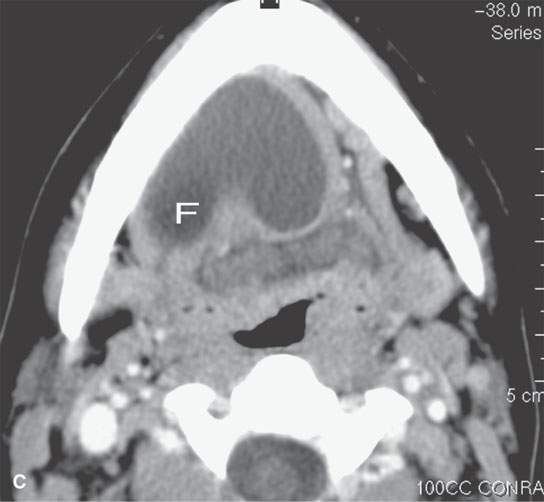
FIGURE 8.3. Three cysts in the floor of the mouth submandibular space region showing variability of anatomic localization. A: Contrast-enhanced computed tomography (CECT) of a dermoid cyst containing fatty (F) globules confined to the midline floor of the mouth. B: CECT of an epidermoid cyst extending from the sublingual to the submandibular spaces. C: CECT of a dermoid with low-density, likely fat (F) content predominantly in the midline floor of the mouth but protruding into the sublingual space.
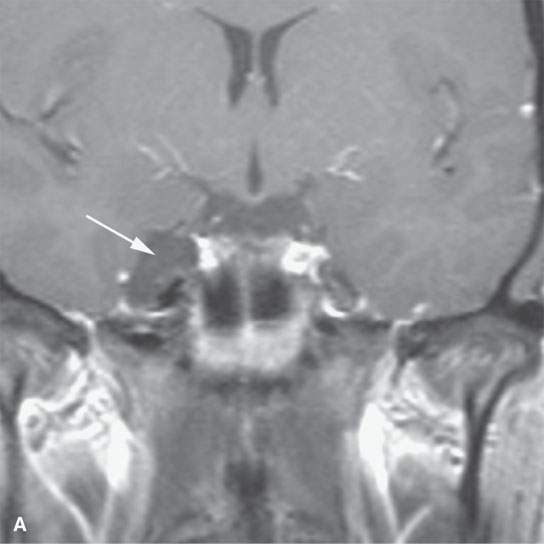
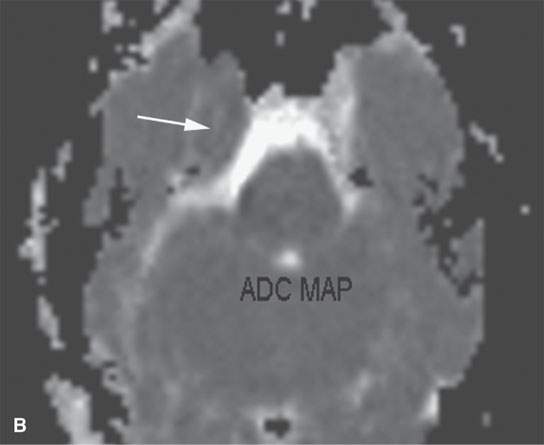
FIGURE 8.4. A: Contrast-enhanced computed tomography of a paracavernous epidermoid cyst (arrow). B: Apparent diffusion coefficient magnetic resonance map showing restricted diffusion (arrow) characteristic of epidermoid cysts.
Epidermoid cysts (congenital cholesteatomas) occur more frequently than dermoids in the cranial cavity.1,6 They may also involve the diploic space of the cranial vault (Figs. 8.5 and 8.6). There is a tendency for epidermoids to present off the midline.4,5 The cerebellopontine angle (CPA), parasellar, and middle cranial fossa are favored sites.1,2 Frontal and parietal bones are the most frequent sites of cranial vault lesions. All portions of the temporal bone may be involved (Fig. 8.7). Extracranial lesions outside of those involving the temporal bone are unusual. They may occur in the floor of the mouth, submandibular space, and neck.

FIGURE 8.5. Plain film of a calvarial epidermoid (arrow) showing typical benign expansile lesion of the diploic space.
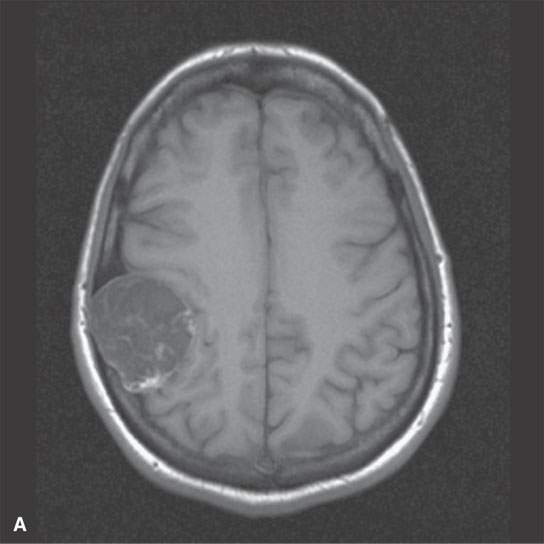
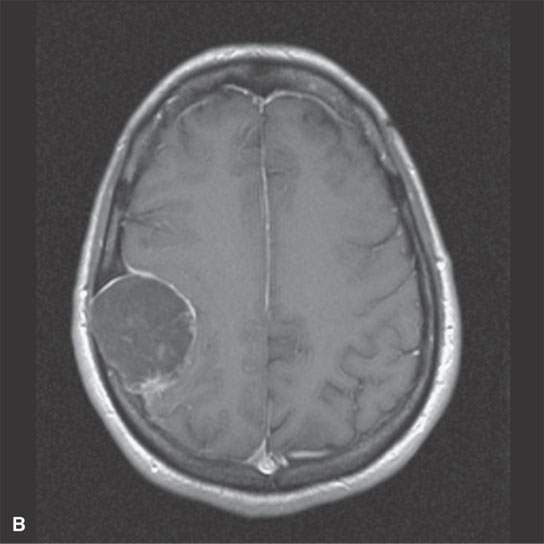
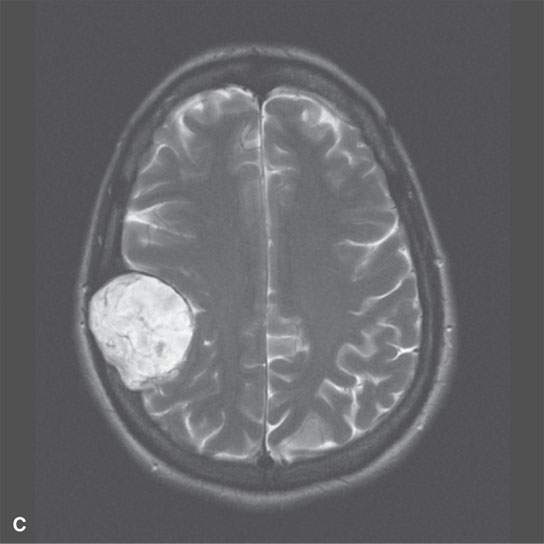
FIGURE 8.6. Magnetic resonance imaging of a calvarial/diploic origin epidermoid cyst to illustrate lack of enhancement and internal signal characteristics. A: Non–contrast-enhanced T1W image showing slightly inhomogeneous interstices with some focal higher signal intensity at the posterior margin. B: Contrast-enhanced T1-weighted image showing enhancement of the displaced dura but not of the epidermoid. C: T2-weighted image showing bright but inhomogeneous interstices of the cyst.
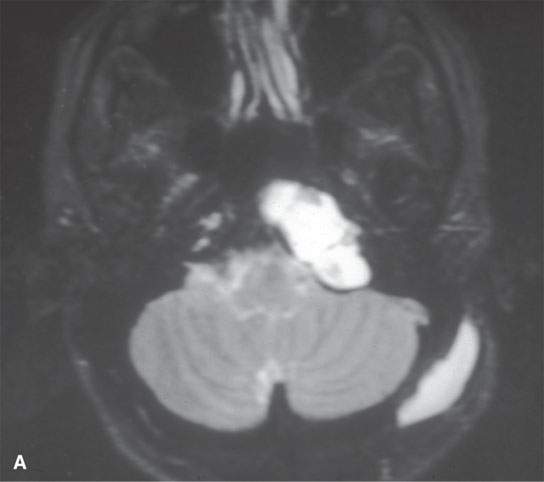
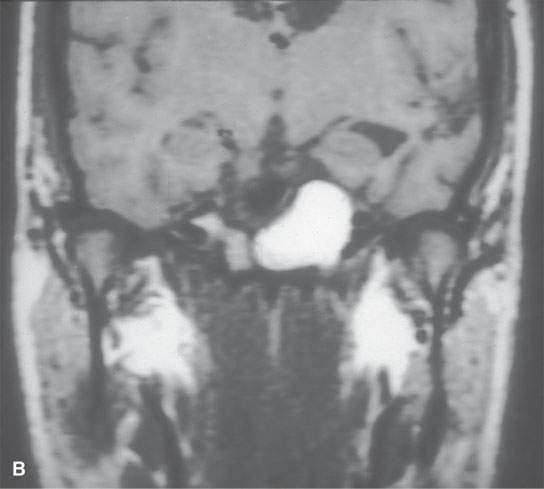
FIGURE 8.7. Magnetic resonance imaging of a surgically proven epidermoid cyst of the petrous apex. A: T2-weighted image shows septated mass with content brighter than cerebrospinal fluid. B: Non–contrast-enhanced T1-weighted image shows a high signal visible equivalent to fat, likely in part related to cholesterol in solution rather than a more bound state—this is an unusual appearance for an epidermoid.
Dermoids or epidermoids may rupture during surgery or spontaneously.7 Rarely, fatty density globules have been seen scattered throughout the subarachnoid space (Fig. 8.8). Leptomeningeal enhancement may reflect the “chemical” meningitis induced by the cyst contents (Fig. 8.9).8 It is useful for a neurosurgeon to be aware if the lesion is a dermoid or epidermoid so that care can be taken to avoid spillage of the cyst contents.
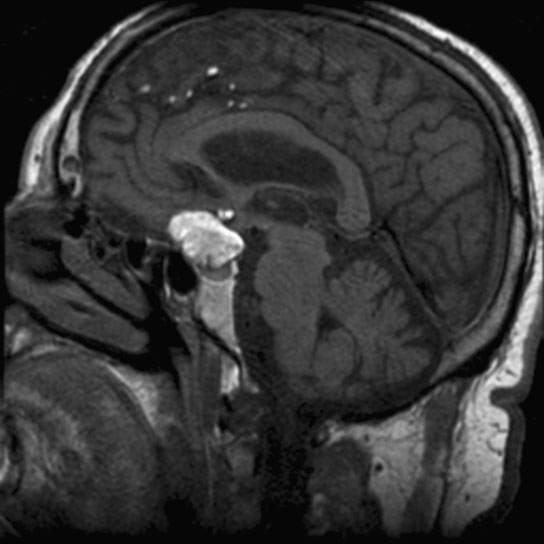
FIGURE 8.8. T1-weighted non–contrast-enhanced magnetic resonance showing a midline suprasellar dermoid cyst that ruptured, resulting in globules of high signal intensity content being deposited in the subarachnoid space.
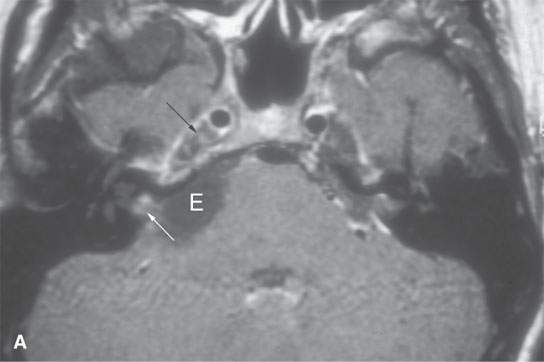
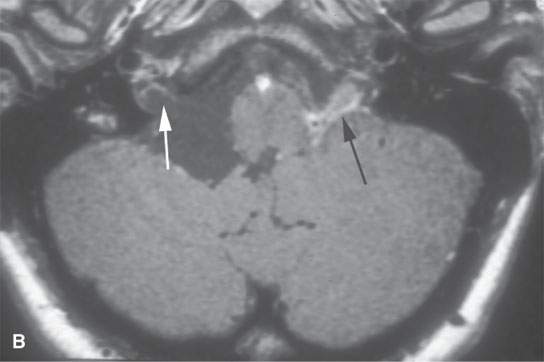
FIGURE 8.9. Contrast-enhanced T1-weighted magnetic resonance images of a ruptured cerebellopontine angle epidermoid cyst (E) showing chemical arachnoiditis. A: Nodular leptomeningeal enhancement within the internal auditory canal (white arrow) and trigeminal cistern (black arrow). B: “Cake” of enhancement around lower cranial nerves in the left medullary cistern (black arrow) and in the jugular fossa region on the right (white arrow).
Imaging Appearance
Dermoids are usually well-circumscribed, round, or lobulated lesions (Figs. 8.1–8.8).3 Calcifications may be present (Fig. 8.2). A thick, semisolid composition of secretions of sebaceous glands and desquamated epithelium fills its cavity. The lesions themselves do not enhance with intravenous (IV) contrast unless there is an associated pachymeningitis, rupture with chemical arachnoiditis, or the very rare associated cancer.3 The cyst contents may range from hypodense to slightly hyperdense to normal brain on CT, but hyperdense lesions are uncommon. On T1-weighted magnetic resonance (MR) images, the cyst contents may range from hypointense to markedly hyperintense (Fig. 8.8) to brain with an equally variable appearance on T2-weighted images.1,2,8 T2-weighted images will usually suggest the “cystic” nature of the lesion (Fig. 8.10), but the contents are not fluid. Diffusion-weighted imaging (DWI) will show restricted diffusion in frankly cystic-appearing areas (Fig. 8.10).
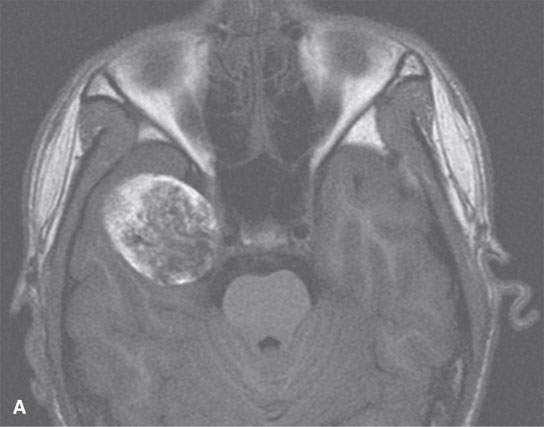
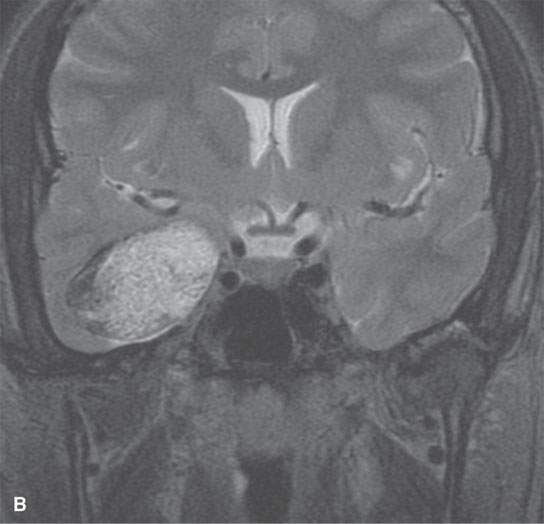
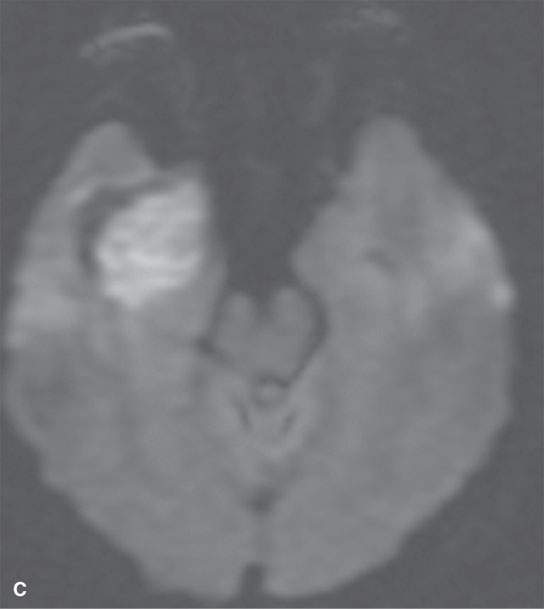
FIGURE 8.10. Magnetic resonance of paracavernous/middle cranial fossa showing complexity possible in the internal appearance of dermoid cysts. A: Non–contrast-enhanced T1-weighted image. B: T2-weighted image. C: Diffusion-weighted image showing mainly restricted diffusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








