Ophthalmic ultrasound is an invaluable tool that provides quick and noninvasive evaluation of the eye and the orbit. It not only allows the clinicians to view structures that may not be visible with routine ophthalmic equipment or neuroimaging techniques but also provides unique diagnostic information in various ophthalmic conditions. In this article, the basic principles of ophthalmic ultrasound and examination techniques are discussed. Its clinical application is illustrated through a variety of ocular pathologic abnormalities (eg, narrow angles, ciliary body tumor, detached retina, choroidal melanoma, and papilledema).
Key points
- •
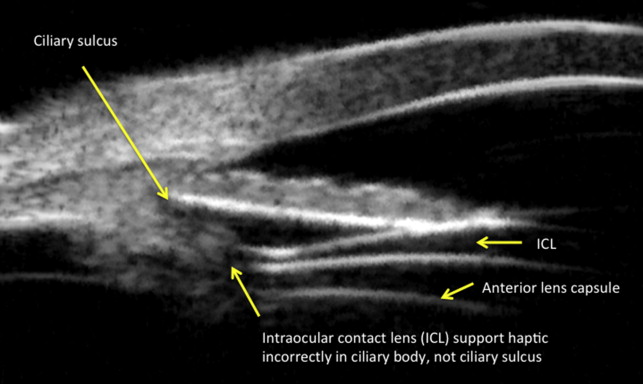
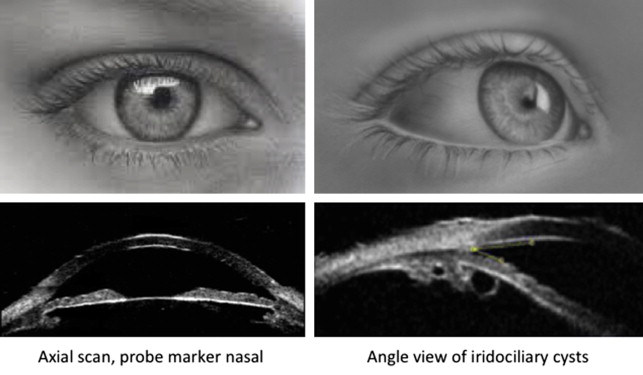
Ultrasound biomicroscopy provides high-resolution images of the anterior segment of the eye, allowing examination of iris, angles, ciliary body, and intraocular lens.
- •
Ophthalmic B-scan is commonly used to evaluate the posterior segment of the eye in the presence of opaque optical media. It helps in detecting optic nerve head drusen, retinal detachments, and tumors and is useful for examining the eye and the orbit.
- •
Ophthalmic A-scan is commonly used for measuring axial eye length in order to calculate intraocular lens power for implantation during cataract surgery.
- •
Standardized A, a special type of A-scan, is primarily used for differentiating ocular tumors and measuring optic nerve sheath diameters and extraocular muscle sizes.
Basic principles
Ophthalmic ultrasound (A-scan and B-scan) is performed primarily for the 3 following reasons:
- 1.
When opaque media prevent direct view of the ocular fundus and periphery, ultrasound determines the presence or absence of ocular tumors, retinal detachment, foreign bodies, or other pathologic abnormality.
- 2.
When media are clear, ultrasound allows imaging of intraocular and extraocular structures, such as optic nerve head drusen, orbital structures and lesions, and internal structure of intraocular lesions.
- 3.
Ultrasound allows the measurement of axial length before cataract surgery in order to determine intraocular lens power.
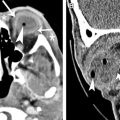
B-mode, or brightness mode, is a 2-dimensional sector image used to characterize ocular structures and determine the status of the globe and orbit. These gray-scale images are generated by changes in tissue medium that reflect sound. In ophthalmology, sector images of the globe are displayed 90° from traditional medical ultrasound. Body ultrasound images are oriented with the probe surface at the top of the display, whereas ophthalmic images display the probe surface on the left. Fig. 1 shows the orientation difference between abdominal and ophthalmic ultrasound image presentations. A probe orientation marker indicates the top of the display, so a B-scan with the marker line facing the nose would have the nasal retina at the top of the screen and temporal retina displayed in the lower aspect of the screen (see Fig. 1 ). Traditional ophthalmic ultrasound frequencies for globe and orbit imaging are 10 to 12 MHz. High-frequency posterior probes are 17 to 20 MHz and are focused to provide highest resolution at the optic nerve/retina surface, but have minimal orbital penetration.
B-scans are systematically performed to examine all clock hours with both transverse (across several clock hours) and longitudinal (along a single meridian) scans. In Fig. 1 , placing the probe on the cornea with the marker line facing the nose performs an axial transverse scan. It shows nasal structures at the top of the screen and temporal structures below, a curved bright line from posterior lens capsule, and a V-shaped acoustic shadow from the optic nerve. Sound is systematically swept through all ocular quadrants obtaining transverse scans of several clock hours at once. Longitudinal scans image along just one clock hour, or meridian, from the optic nerve to the anterior periphery. They are used to document anterior/posterior extent of anatomy and pathologic abnormality. Examples are found later in the Basic Examination and Clinical Cases sections in this article.
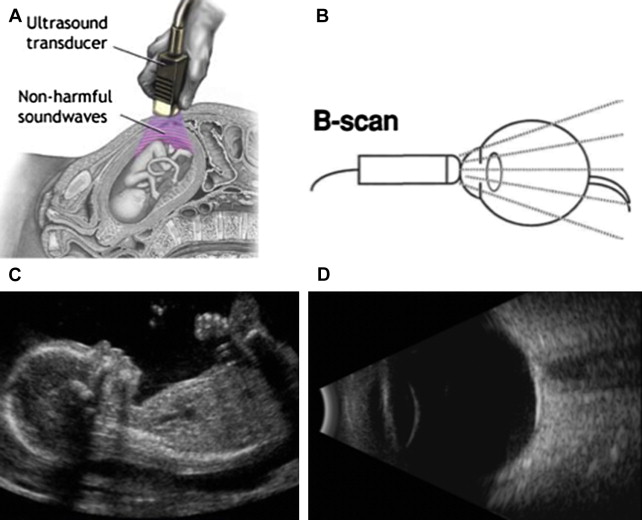
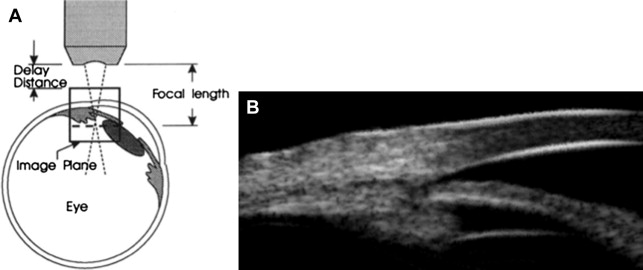
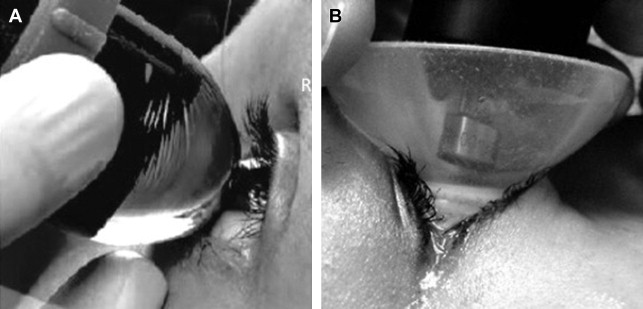
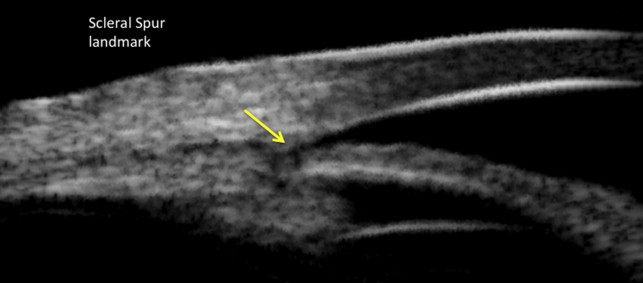
High-frequency ophthalmic ultrasound, for anterior segment imaging, is referred to as UBM, ultrasound biomicroscopy, and uses 35 to 70 MHz with 50 MHz being the most common. The higher frequency provides higher resolution but less tissue penetration. Its shallow depth of penetration would not be useful for evaluation of the optic nerve, but rather to show, in detail, structures, such as the cornea, anterior chamber, angles, iris, and ciliary body ( Figs. 2 and 3 ). The UBM is ideal for examining the eye for narrow or closed angles and structures behind the iris, such as cysts, tumors, and dislocated crystalline and intraocular lenses. UBM is performed with a sterile, fluid-filled ClearScan bag or a saline-filled plastic or silicon shell resting on the sclera ( Fig. 4 ). Axial and other transverse scans are routinely performed to document normal tissue or the extent of pathologic abnormality (see Fig. 2 , left). Scans for examining the angle between cornea and iris in glaucoma patients are performed primarily with longitudinal scans (see Fig. 2 , right). Most ophthalmic UBM probes use sector scanning, but some use linear transducer movement. Sector probes pivot a single transducer so that sound is generated in a fan-shaped display. Sector scans make sense for the eye because it allows the sound waves to be more perpendicular to a wider area of the fundus, thereby producing more clinically useful data. Linear probes are sometimes used in UBM scans. They also have a single transducer, but it is moved back and forth linearly, thereby producing a rectangular image ( Figs. 5–8 ).
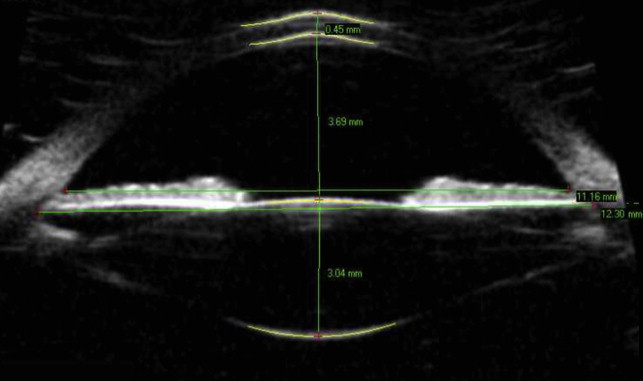
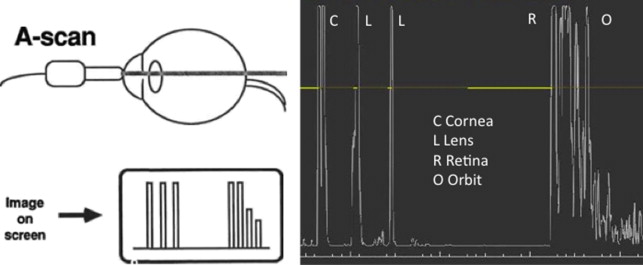
A-mode, or Amplitude, scans are also displayed with the ocular surface at the left of the screen and are one-dimensional, up-and-down spikes. Axial eye lengths measured by A-scan are used to calculate intraocular lens power for implantation during cataract surgery.
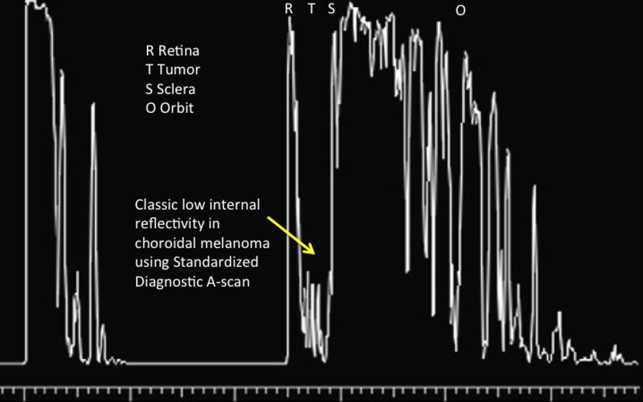
All of the above modes for anterior and posterior B-scans and eye length A-scans use fixed-focus transducers. The only exception is a second, very specific A-mode, referred to as Standardized A-scan, that uses a transducer emitting parallel sound beam and a unique amplifier ( Fig. 9 ). This mode is used to characterize a lesion’s internal structure and to perform measurements of intraocular and extraocular structures. The operator determines tissue or tumor structure by interpreting the relative amplitude of each. Tissue reflection and absorption produce an A-scan pattern of varying heights or amplitudes. For example, choroidal melanoma produces a low to medium height of echoes from within the tumor due to the homogeneity of the cells. In contrast, a choroidal hemangioma will show an echo pattern from within the lesion of high-amplitude echoes, because of the irregular cellular pattern. Solid tumors such as melanomas have a steeper and uniform falloff of echoes from within the lesion than a vascular lesion. Vascular lesions present with an irregular pattern of both high and low echoes. Although extremely useful in experienced hands, the examination technique has a steep learning curve and is not universally used.
The relationship between A-scan and B-scan echoes is that a tall echo on A-scan will correspond to a bright echo on B-scan, both indicating high structural density.
Diagnostic ultrasound is significantly different from low-frequency, high-power therapeutic ultrasound in the following 2 ways:
- 1.
It does not generate heat in ocular tissues with the US Food and Drug Administration (FDA) required low energy limits.
- 2.
The frequency is in the megahertz range of millions of cycles per second, whereas therapeutic ultrasound is in the kilohertz range of thousands of cycles per second.
Ophthalmic ultrasound uses a fixed energy system, whereas other forms of body scanning may use equipment that allows the operator to adjust the amount of sound energy that is being directed into tissue. The FDA limits power levels for sound energy used in ocular examinations. However, confirmation should be made with the Regulatory Department if there are any limits in effect for using superficial scanning probes on the eye. Some small probes on general ultrasound systems may be labeled “For Ophthalmic Use” and would be the optimal choice if available.
A clinically useful echo display depends on the 3 following factors (see Fig. 3 ):
- 1.
Angle of incidence between sound beam and interface with structure
- 2.
Difference between structural mediums at the interface
- 3.
Surface condition of the interface
Very dissimilar mediums produce larger echoes ( Fig. 10 A), whereas mediums that are closer in consistency produce smaller echoes (see Fig. 10 B). Note that if the probe is not perpendicular, then there will be marked weakening of the reflected sound (see Fig. 10 C, D).
Artifacts are echoes that do not represent true structures. The eye’s crystalline lens is a primary culprit for producing an abnormally curved peripheral retina due to attenuation and scattering of sound waves as they travel through the lens. This particular artifact is found in axial B-scans that direct sound through the lens and is called Baum bumps ( Fig. 11 ) for Gilbert Baum, MD, a pioneer in medical ultrasound imaging from the 1960s forward.
Another example of artifact is shown in Fig. 12 . In the case of calcified optic nerve head drusen, it is common to see a weaker duplicate drusen echo in the orbit. The reverberation artifact is displayed at the same distance to the right of the actual drusen echo as the real drusen is from the probe surface. A low gain setting is important to differentiate drusen from the surrounding highly reflective orbital tissue.
Basic principles
Ophthalmic ultrasound (A-scan and B-scan) is performed primarily for the 3 following reasons:
- 1.
When opaque media prevent direct view of the ocular fundus and periphery, ultrasound determines the presence or absence of ocular tumors, retinal detachment, foreign bodies, or other pathologic abnormality.
- 2.
When media are clear, ultrasound allows imaging of intraocular and extraocular structures, such as optic nerve head drusen, orbital structures and lesions, and internal structure of intraocular lesions.
- 3.
Ultrasound allows the measurement of axial length before cataract surgery in order to determine intraocular lens power.
B-mode, or brightness mode, is a 2-dimensional sector image used to characterize ocular structures and determine the status of the globe and orbit. These gray-scale images are generated by changes in tissue medium that reflect sound. In ophthalmology, sector images of the globe are displayed 90° from traditional medical ultrasound. Body ultrasound images are oriented with the probe surface at the top of the display, whereas ophthalmic images display the probe surface on the left. Fig. 1 shows the orientation difference between abdominal and ophthalmic ultrasound image presentations. A probe orientation marker indicates the top of the display, so a B-scan with the marker line facing the nose would have the nasal retina at the top of the screen and temporal retina displayed in the lower aspect of the screen (see Fig. 1 ). Traditional ophthalmic ultrasound frequencies for globe and orbit imaging are 10 to 12 MHz. High-frequency posterior probes are 17 to 20 MHz and are focused to provide highest resolution at the optic nerve/retina surface, but have minimal orbital penetration.
B-scans are systematically performed to examine all clock hours with both transverse (across several clock hours) and longitudinal (along a single meridian) scans. In Fig. 1 , placing the probe on the cornea with the marker line facing the nose performs an axial transverse scan. It shows nasal structures at the top of the screen and temporal structures below, a curved bright line from posterior lens capsule, and a V-shaped acoustic shadow from the optic nerve. Sound is systematically swept through all ocular quadrants obtaining transverse scans of several clock hours at once. Longitudinal scans image along just one clock hour, or meridian, from the optic nerve to the anterior periphery. They are used to document anterior/posterior extent of anatomy and pathologic abnormality. Examples are found later in the Basic Examination and Clinical Cases sections in this article.
High-frequency ophthalmic ultrasound, for anterior segment imaging, is referred to as UBM, ultrasound biomicroscopy, and uses 35 to 70 MHz with 50 MHz being the most common. The higher frequency provides higher resolution but less tissue penetration. Its shallow depth of penetration would not be useful for evaluation of the optic nerve, but rather to show, in detail, structures, such as the cornea, anterior chamber, angles, iris, and ciliary body ( Figs. 2 and 3 ). The UBM is ideal for examining the eye for narrow or closed angles and structures behind the iris, such as cysts, tumors, and dislocated crystalline and intraocular lenses. UBM is performed with a sterile, fluid-filled ClearScan bag or a saline-filled plastic or silicon shell resting on the sclera ( Fig. 4 ). Axial and other transverse scans are routinely performed to document normal tissue or the extent of pathologic abnormality (see Fig. 2 , left). Scans for examining the angle between cornea and iris in glaucoma patients are performed primarily with longitudinal scans (see Fig. 2 , right). Most ophthalmic UBM probes use sector scanning, but some use linear transducer movement. Sector probes pivot a single transducer so that sound is generated in a fan-shaped display. Sector scans make sense for the eye because it allows the sound waves to be more perpendicular to a wider area of the fundus, thereby producing more clinically useful data. Linear probes are sometimes used in UBM scans. They also have a single transducer, but it is moved back and forth linearly, thereby producing a rectangular image ( Figs. 5–8 ).
A-mode, or Amplitude, scans are also displayed with the ocular surface at the left of the screen and are one-dimensional, up-and-down spikes. Axial eye lengths measured by A-scan are used to calculate intraocular lens power for implantation during cataract surgery.
All of the above modes for anterior and posterior B-scans and eye length A-scans use fixed-focus transducers. The only exception is a second, very specific A-mode, referred to as Standardized A-scan, that uses a transducer emitting parallel sound beam and a unique amplifier ( Fig. 9 ). This mode is used to characterize a lesion’s internal structure and to perform measurements of intraocular and extraocular structures. The operator determines tissue or tumor structure by interpreting the relative amplitude of each. Tissue reflection and absorption produce an A-scan pattern of varying heights or amplitudes. For example, choroidal melanoma produces a low to medium height of echoes from within the tumor due to the homogeneity of the cells. In contrast, a choroidal hemangioma will show an echo pattern from within the lesion of high-amplitude echoes, because of the irregular cellular pattern. Solid tumors such as melanomas have a steeper and uniform falloff of echoes from within the lesion than a vascular lesion. Vascular lesions present with an irregular pattern of both high and low echoes. Although extremely useful in experienced hands, the examination technique has a steep learning curve and is not universally used.
The relationship between A-scan and B-scan echoes is that a tall echo on A-scan will correspond to a bright echo on B-scan, both indicating high structural density.
Diagnostic ultrasound is significantly different from low-frequency, high-power therapeutic ultrasound in the following 2 ways:
- 1.
It does not generate heat in ocular tissues with the US Food and Drug Administration (FDA) required low energy limits.
- 2.
The frequency is in the megahertz range of millions of cycles per second, whereas therapeutic ultrasound is in the kilohertz range of thousands of cycles per second.
Ophthalmic ultrasound uses a fixed energy system, whereas other forms of body scanning may use equipment that allows the operator to adjust the amount of sound energy that is being directed into tissue. The FDA limits power levels for sound energy used in ocular examinations. However, confirmation should be made with the Regulatory Department if there are any limits in effect for using superficial scanning probes on the eye. Some small probes on general ultrasound systems may be labeled “For Ophthalmic Use” and would be the optimal choice if available.
A clinically useful echo display depends on the 3 following factors (see Fig. 3 ):
- 1.
Angle of incidence between sound beam and interface with structure
- 2.
Difference between structural mediums at the interface
- 3.
Surface condition of the interface
Very dissimilar mediums produce larger echoes ( Fig. 10 A), whereas mediums that are closer in consistency produce smaller echoes (see Fig. 10 B). Note that if the probe is not perpendicular, then there will be marked weakening of the reflected sound (see Fig. 10 C, D).