Figure 12.1 Physiologic SPNBF. A, Anteroposterior (AP) view of the left femur in a two-month-old infant demonstrates SPNBF along the medial (open arrow) and lateral (solid arrows) aspects of the femoral shaft. The thickness of the new bone measured from the original cortex to the outer margin of the new bone is 1.4 mm laterally. Note that the margins of the new bone are ill defined. B, A radiograph one month later shows blending of the SPNBF with the original cortex. A faint linear radiolucency separates these two regions (arrows). At this stage, the finding may be characterized as a “double” or “split” cortex.
Figure 12.2 Physiologic SPBNF. AP view of the right forearm in a six-week-old infant shows a distinct zone of SPNBF along the medial aspect of the proximal ulna (bold white arrows). SPNBF is evident along the lateral aspects of the shafts of the radius and ulna, which blend with the underlying cortex (thin white arrows). Note also the nutrient canal in the proximal ulna (black arrow).
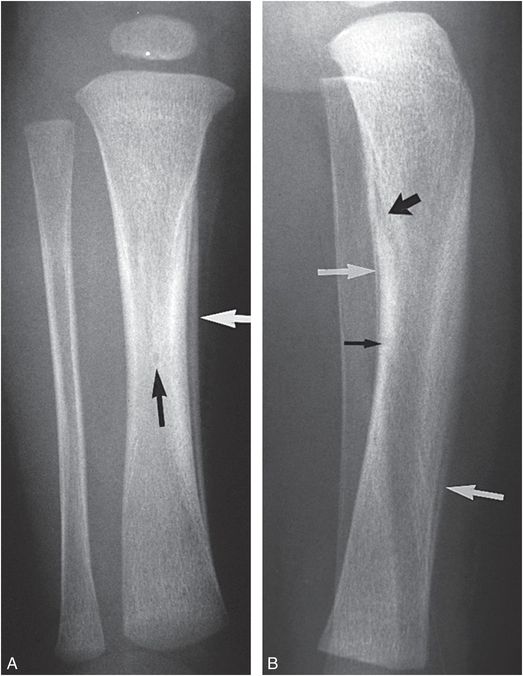
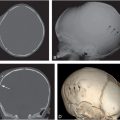
Figure 12.3 Physiologic SPNBF; nutrient canal tibia. AP (A) and lateral (B) views of the tibia in a young infant demonstrate well-organized SPNBF medially and to a lesser extent anteriorly and posteriorly (white arrows). Note that the new bone is restricted to the diaphysis. Physiologic SPNBF along the lateral aspect of the tibia is a rare occurrence. Note the nutrient canals (black arrows).
Figure 12.4 Physiologic SPNBF humerus. AP view of the right humerus in a one-month-old infant demonstrates SPNBF along the medial aspect of the proximal humeral shaft (straight arrow). Haziness of the lateral cortex probably reflects SPNBF, which is insufficiently distinct to produce a discrete band of radiodensity. Note the nutrient canal (curved arrow).
Figure 12.5 Step-off. AP view of the distal right radius and ulna in a two-month-old infant demonstrates an acutely angulated cortical margin, or step-off, at the junction of the SPBC and adjacent metaphyseal cortex (small arrows). Note that the cortical margin at this site is indistinct in relation to active bone resorption in this region of rapid remodeling. Note also the indistinct cortical margin along the lateral aspect of the distal radial diaphysis, related to rapid deposition of SPNBF, which is not discretely separated from the remainder of the cortex (large arrows). (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
Figure 12.6 Physiologic SPNBF; step-off; proximal tibial cortical irregularity. Faint SPNBF is noted along the medial aspect of the tibial diaphysis (thin arrows). A conspicuous step-off configuration is noted along the medial aspect of the proximal tibial metaphysis (bold solid arrow). In addition, there is a proximal tibial cortical irregularity (open arrow). (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
Postmortem radiographic studies have further delineated the characteristics of SPNBF in young infants. Kwon and colleagues used complete skeletal surveys (SSs) to study 101 infants who died of the sudden infant death syndrome (SIDS) (7). SPNBF occurred in 35 cases (35%). The prevalence of SPNBF between 1 and 2 months, 2 and 3 months, and 3 and 4 months of age was 37%, 55%, and 35%, respectively. No instance of SPNBF was observed in infants under one month or over four months of age. After four months, SPNBF showed evidence of incorporation into the cortex. The tibia was involved in 29% of cases; two-thirds bilateral, one-third unilateral. Femoral SPNBF was noted in 14% of cases; 79% bilateral, 21% unilateral. Humeral involvement was noted in 12% of infants; 42% bilateral, 58% unilateral. Ulnar SPNBF occurred in 7 infants; 70% bilateral, 30% unilateral. Radial involvement was uncommon, noted in only 2% of cases. In addition to the tendency for bilaterality, SPNBF was frequently noted to involve different long bones in the same patient. Combined femoral and tibial SPNBF was noted in 31%, tibial and humeral involvement in 29%, and femoral and humeral or tibial and ulnar SPNBF in 20% of infants.
The radiologic appearances of SPNBF at different anatomic sites vary, but they share the feature of a smooth, regular band of mineralized density separated from the underlying cortex by a zone of radiolucency (Figs. 12.1A, 12.2–12.4, 12.6). This sharp separation is most evident in infants under four months of age, but mature, organized SPNBF may not be distinctly separate from the underlying cortex (Figs. 12.1B, 12.2, 12.5) up to six months of age. Our studies suggest that SPNBF greater than 2 mm in thickness is an abnormal finding (7). Furthermore, physiologic SPNBF appears to be very unusual under one month and over five months of age.
A practical problem often arises when SPNBF is suspected in an anatomic region which is not the focus of the radiographic examination. A view of the abdomen in a young infant may show smooth regular SPNBF bilaterally, and detection can prompt additional imaging (Fig. 12.7). Given the prevalence of physiologic SPNBF, such additional radiographic assessment is usually unnecessary; however, a judicious use of supplementary imaging may occasionally be appropriate when the imaging features, patient age, and clinical setting do not permit a confident determination.
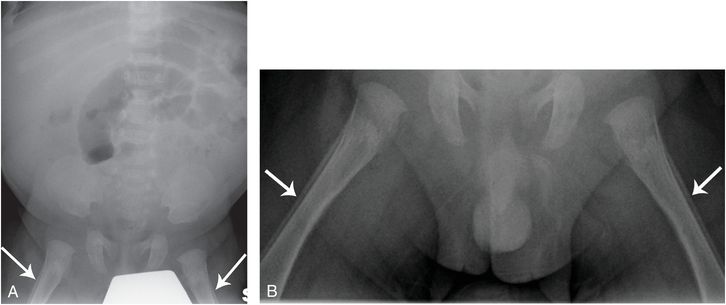
Figure 12.7 Physiologic SPNBF. A seven-week-old infant with projectile vomiting. A, Supine radiograph of the abdomen shows SPNBF involving both femurs (arrows). Additional imaging of the femurs was requested. B, Frontal view of the femurs shows regular symmetric SPNBF measuring greater than 2 mm consistent with normal physiologic SPNBF. No further skeletal imaging was done.
Although SPNBF of various etiologies may involve the humeri, the position and radiographic projection of the humeri can result in the spurious appearance of SPNBF (Fig. 12.8). This results from projection of two adjacent cortical margins with an apparent intervening lucency. The pattern can usually be identified by an abrupt change in the character of the cortex, rather than a gradually tapering margin of SPNBF. In problematic cases, additional views will be required to resolve the issue. A related misleading image can be evident in the ribs when superimposed cortical margins of the lateral rib arc suggest SPNBF (see Fig. 12.11).
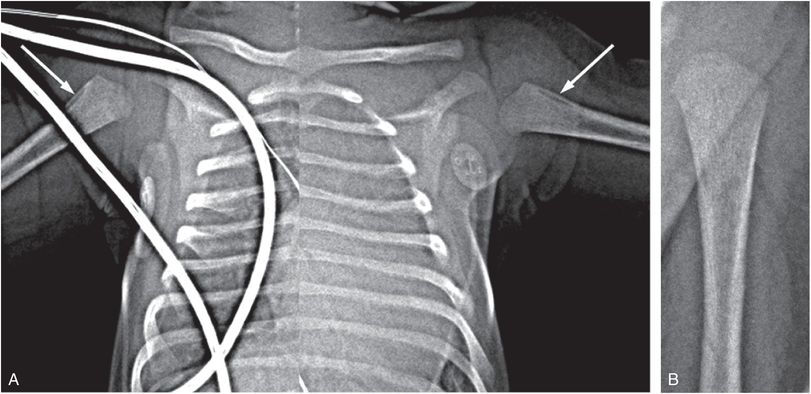
Figure 12.8 Spurious SPNBF related to radiographic projection. A 14-day-old with congenital heart disease, and pre-aortic balloon dilatation. A, Supine radiograph of the chest cropped to the shoulders shows apparent SPNBF involving the proximal humeri (arrows). B, AP radiograph of the left humerus in a different position shows no SPNBF.
Acute fractures, particularly those involving the femur, can occur through regions of physiologic SPNBF. The physiologic new bone may be erroneously construed as post-traumatic, suggesting that the shaft fracture is in a healing phase (see Fig. 3.23) (8).
Normal metaphyseal variants
Variations in the radiographic appearances of the metaphyses in infancy can be explained by the distinctive morphology of these portions of the growing skeleton. The subperiosteal bone collar (SPBC), an osseous ring that surrounds the primary spongiosa of the metaphysis and to a variable extent the physis, has been described in depth in Chapters 1 and 2 (9–14). This osseous collar, or “bone bark,” explains the appearance of a number of the metaphyseal variants that may be confused with the classic metaphyseal lesion (CML) (1, 15, 16).
Step-off
The step-off is an apparent abrupt angulation of the metaphyseal cortex as it approaches the physis (Figs. 12.5, 12.6, 12.9, 12.10). As seen histologically, this occurs at the junction of the SPBC and the adjacent cortex (see Fig. 3.27). The subperiosteal collar is generally quite well defined and the adjacent cortical margin is indistinct secondary to bone resorption at this site of rapid remodeling. The step-off configuration was noted in the distal radius (15%), distal ulna (5%), distal femur (3%), proximal tibia (4%), and proximal fibula (1%) in Kleinman and associates’ study. It was bilateral in 41% and unilateral in 59% of infants (15).
Figure 12.9 Distal femur step-off. AP view of the distal right femur in a five-month-old infant shows step-off configurations (arrows), most notable medially. (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
Figure 12.10 Step-off proximal fibula; beak proximal tibia. A step-off pattern is evident along the lateral aspect of the proximal fibula (curved arrow). The physeal margin of the proximal tibial metaphysis joins the medial metaphyseal cortex with an acute angulation (straight arrow). (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
The step-off configuration may be difficult to distinguish from a CML, because a principal morphologic feature of the CML is undercutting of the SPBC by the fracture line (see Chapter 2) (14). A lucent line that extends obliquely from the margin of the SPBC centrally toward the chondro-osseous junction (COJ) is commonly present with the CML. Normal variants usually blend with the cortex and if an intervening lucency is present, it is usually oriented parallel to the adjacent cortex. Therefore, the presence of an apparent cortical discontinuity at the site of a prominent SPBC is not sufficient to diagnose a CML; an oblique fracture line that appears to actually separate an osseous metaphyseal fragment points to an injury.
A normal step-off contour can be incidentally noted on a chest radiograph, and this may prompt an assessment for a suspected inflicted injury (Fig. 12.11). A careful analysis reveals this finding to be a prominent SPBC that extends around the periphery of the COJ. The step-off configuration can be striking in toddlers and a comparison view of the opposite side may reveal an identical normal finding, usually putting concerns of inflicted injury to rest (Fig. 12.12).
Figure 12.11 Normal step-off appearance of the proximal humerus. A 3½-month-old infant with respiratory distress. AP radiograph of the chest, cropped to the right shoulder, shows a step-off configuration of the proximal humerus (thick white arrows). Note that the osseous density can be followed across the metaphysis (thin white arrows) consistent with the normal SPBC. Also note spurious SPNBF (black arrows) along the lateral rib margin, related to projection.
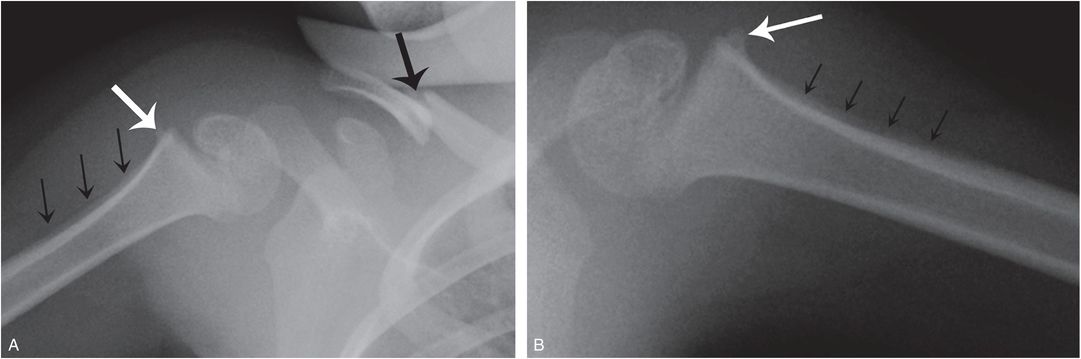
Figure 12.12 Normal step-off configuration – the value of a comparison view. A 2¾-year-old who became inconsolable after reportedly falling off a kitchen chair onto the right shoulder. A, AP radiograph of the right shoulder shows a displaced clavicular fracture (large black arrow). There is a step-off appearance of the proximal humeral metaphysis (white arrow), with the suggestion of SPNBF (small black arrows) that was viewed as concerning for a healing, unreported injury. B, A comparison of the left shoulder at one week follow-up showed an identical appearance on the left, consistent with a normal SPBC (white arrow) and spurious SPNBF (black arrows).
Spur
The SPBC frequently extends beyond the metaphysis, forming a discrete linear mineralized structure at the periphery of the physis (Figs. 12.13–12.15) (also see Figs. 3.27, 4.2). This occurs at a variety of sites, including the distal radius (3%), distal ulna (3%), and distal femur (1%), and can also be identified in the metacarpals (1%) and metatarsals (1%). It is bilateral in 25% of cases. The appearance in the lateral aspect of the distal femur is characteristic, and an example with histologic correlation is shown in Figure 3.27. As with the step-off, the feature that allows differentiation of the metaphyseal spur from the CML is the absence of a fracture line that undercuts the SPBC and extends centrally toward the physis.
Figure 12.13 Spur. AP view of the distal right forearm in a two-month-old infant demonstrates bony projections (arrows) extending from the peripheral margins of the distal radius and ulna. The spur conforms to a prominent SPBC that surrounds the zone of hypertrophied chondrocytes of the physis. (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
Figure 12.14 Spur. PA view of the left hand in a three-month-old infant shows a spur arising from the radial aspect of the base of the first metacarpal (arrow). (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
Figure 12.15 Spur. AP view of the foot in a six-week-old infant demonstrates a spur (arrow) arising from the lateral aspect of the base of the fifth metatarsal. (From Kleinman PK, Belanger PL, Karellas A, Spevak MR. Normal metaphyseal radiologic variants not to be confused with findings of infant abuse. AJR. 1991;156:781–3.)
Beak
When a concave metaphyseal contour forms an acute angle with the adjacent physeal margin, an osseous projection or “beak” may be formed. This is most notable in the medial aspect of the proximal humerus (16%) and is often quite sharply defined; it should not produce confusion with osseous injury (see Fig. 4.2). Less commonly, the feature occurs in the medial aspect of the proximal tibia (1%) (see Fig. 12.10). At this site, the cortex can be indistinct and the finding may suggest a metaphyseal injury. In our study, the beak was bilateral in 77% of cases (15).
Distal ulnar cupping
Glaser noted a concave appearance of the distal ulnar metaphyseal margin (1, 5, 15, 16). He observed that this cupped appearance was due to projection of the physeal margin of the metaphysis at an obliquity. The medial margin of the metaphysis may also appear angulated (Fig. 12.16).
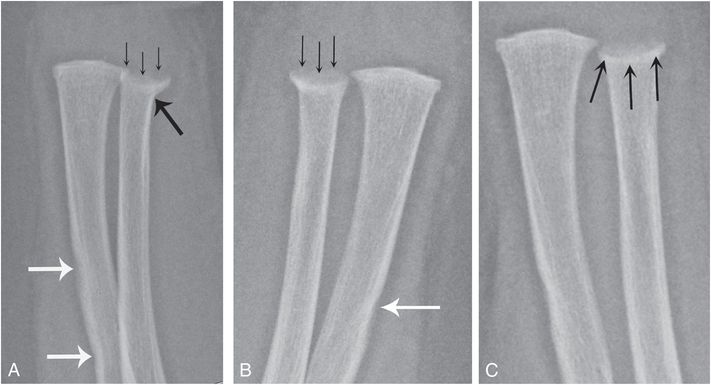
Figure 12.16 Normal distal ulnar cupping. A five-month-old infant undergoing SS for abusive injuries noted in triplet sibling (shown in Fig. 17.6). A, B, Frontal views of the left and right forearms shows a cupped appearance of both distal ulnar metaphyses (thin black arrows). The finding is more evident on the right where there is also apparent adjacent cortical angulation (thick black arrow in A). These findings were initially concerning for metaphyseal injury. Note normal cortical indistinctness along the lateral aspects of both radial shafts (white arrows). C, Two-week follow-up shows less conspicuous cupping, likely related to a more tangential view of the SPBC (arrows). The finding on the right was unchanged (not shown).
In most instances, these normal metaphyseal variants are readily distinguished from injury, but on occasion, despite high-quality radiographs in several projections, it may be impossible to exclude trauma entirely. In these instances, a follow-up radiologic examination in two weeks will resolve matters, because a CML evolves and resolves with healing, whereas a normal radiologic variant will typically be unchanged.
Distal femoral and proximal tibial metaphyseal irregularities in the weight-bearing child
Particularly problematic metaphyseal variants are encountered in the medial aspects of the distal femurs and proximal tibias in toddlers with physiologic bowing of the lower extremities (17). Physiologic genu varum is a common orthopedic condition found in weight-bearing infants and children. Blount differentiated this self-limited process from infantile tibia vara (18). Holt et al. drew attention to variations in ossification involving the posteromedial aspects of the femurs in children with physiologic bowing (19). He cautioned that these “transient vagaries in development” should not be misconstrued as pathologic.
Kleinman and others found distal femoral and/or proximal tibial irregularities in 17 (11%) of 162 toddlers evaluated for physiologic bowing. The age at documentation of metaphyseal irregularities ranged from 15 to 26 months (mean: 18 months). There were 17 instances of distal femoral metaphyseal fragmentation identified in 13 children (8%); unilateral in 9 cases (left N = 6 cases, right N = 3), and bilateral in 4 (Fig. 12.17) (17).
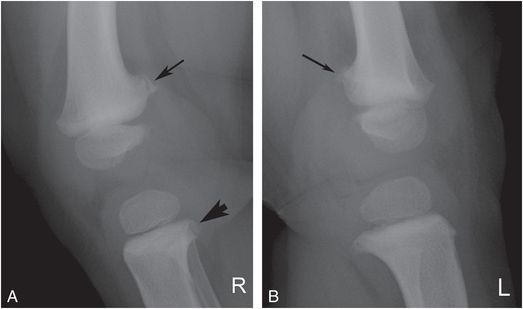
Figure 12.17 Normal metaphyseal fragmentation with physiologic bowing. A, B, Lateral radiographs of right and left knees in a 24-month-old child with bowed legs show bilateral distal femoral fragmentation (arrows) and unilateral proximal tibial fragmentation (arrowhead, A). (From Kleinman PK, Sarwar ZU, Newton AW, Perez-Rossello JM, Rebello G, Herliczek TW. Metaphyseal fragmentation with physiologic bowing: a finding not to be confused with the classic metaphyseal lesion. AJR. 2009;192:1266–8.)
In all but one case the finding was evident only on the lateral projection. Six children (4%) had proximal tibial metaphyseal fragmentation (17). All cases displayed unilateral findings, evident only on the anteroposterior (AP) view in five instances, and only on the lateral projection in one case. Two children (1%) had both distal femoral and proximal tibial fragmentation (Fig. 12.17) (17). All of Kleinman et al.’s cases were well beyond infancy, the age group in which the CML is seen. In all but one case, the femoral metaphyseal fragmentation was only evident on the lateral projections, in contrast to the CML, which is usually noted on the frontal view (20). The fragments were quite discrete, a feature shared with the corner fracture CML pattern, but no crescentic or bucket handle patterns were seen. There was a tendency for the fragments to be somewhat elongated along the long axis of the femur compared with the typical corner fracture pattern described by Caffey (21). One of Kleinman et al.’s cases bore a striking similarity to the example illustrated by Bateson, who also distinguished the findings from those of early Blount’s disease (Fig. 12.18) (22).
Figure 12.18 Normal metaphyseal fragmentation with physiologic bowing. Frontal radiograph of a 15-month-old boy with physiologic bowing shows a conspicuous osseous fragment (arrow) along medial aspect of proximal tibial metaphysis. (From Kleinman PK, Sarwar ZU, Newton AW, Perez-Rossello JM, Rebello G, Herliczek TW. Metaphyseal fragmentation with physiologic bowing: a finding not to be confused with the classic metaphyseal lesion. AJR. 2009;192:1266–8.)
Based on the 10% prevalence of the metaphyseal irregularities in Kleinman’s 162 toddlers with physiologic genu varum, the authors postulated that the abnormal stresses associated with physiologic bowing predispose to irregular metaphyseal ossification in the distal femur and proximal tibia. In one case, concerns of child abuse were raised on a radiograph done for genu varum, leading to Child Protection Team (CPT) consultation and a SS. In neither case was abuse supported. A similar case of unsubstantiated allegations of abuse in a 13-month-old infant is illustrated in Fig. 12.19.
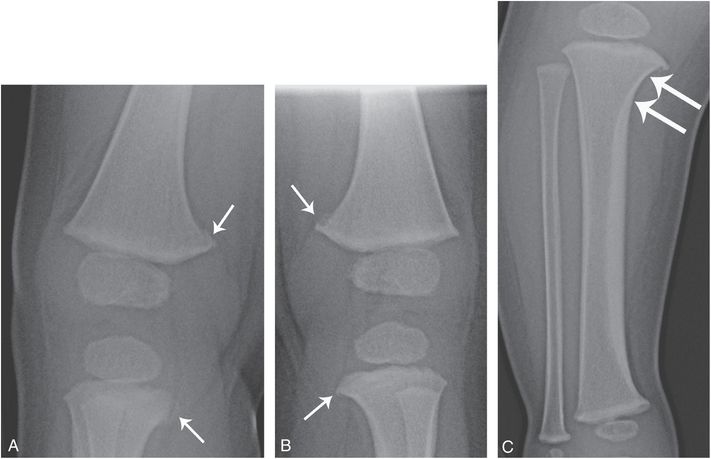
Figure 12.19 Metaphyseal irregularity with physiologic bowing. A 13-month-old infant with a history of bowed legs who reportedly fell with subsequent transient unwillingness to bear weight. Concerns of CMLs were raised on radiographs obtained elsewhere and a report was filed with Child Protective Services (CPS). Right (A) and left posterior oblique (LPO) (B) views of the right and left knees from the subsequent SS show conspicuous fragments along the posteromedial aspects of the distal femoral and proximal tibial metaphyses (arrows). C, AP view of the right lower leg shows a varus orientation of the tibia, centered at the knee. Note the accentuated concavity of the medial metaphysis of the proximal tibia (arrows) and a thick medial diaphyseal cortex, characteristic of physiologic bowing. There were no other findings to suggest abuse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree